
Case Series of an ICT-Based Multimodal Intervention Program for People with Major Neurocognitive Disorders: The SENSE-GARDEN Project
*Corresponding Author(s):
Rozeta Draghici“Ana Aslan” National Institute Of Gerontology And Geriatrics, Bucharest, Romania
Tel:+40 744673819,
Email:rozetadraghici@gmail.com
Andreea Georgiana Marin
Discipline Of Rehabilitation Medicine, “Elias” University Hospital, “Carol Davila” University Of Medicine And Pharmacy, Bucharest, Romania
Email:andreea.budrica@gmail.com
Abstract
Introduction: There are an increasing number of older persons living with major Neurocognitive Disorders (NCDs). Psychosocial interventions are effective in the management of cognition, mood disorders, behavioural and psychological symptoms.
Methodology: This case series presents the impact of a non-pharmacological multimodal intervention which associates reminiscence therapy with multisensory stimulation, training of perception, memory and executive function, as well as physical training elements, to stimulate the person’s reconnection with self, others and environment. The SENSE-GARDEN intervention was applied on 7 participants (Clinical Dementia Rating 2), for 20 sessions, over the course of 4 weeks. Assessments were performed at baseline, after the intervention program and at follow-up, 8 weeks after baseline.
Results: Benefits have been achieved in terms of functioning, participation and quality of life.
Discussion: The outcomes are not of clinical significance but are statistically significant.
Conclusion: This study shows the impact of an innovative intervention applied intensively on persons with major NCD. Further research is required to determine the optimal combination of stimuli for users’ best experience and benefits and to determine the most suited assessment method for such interventions. Study’s International registered report identifier is DERR1-10.2196/14096.
Keywords
Cognitive and physical training; Major neurocognitive disorders; Non-pharmacological multimodal intervention; Reminiscence therapy; Therapeutic environment.
Introduction
Globally, there is an accelerated process of population aging and, within this process, the number of older persons living with Neurocognitive Disorders (NCDs) is also increasing, being estimated that by 2050 this number will exceed 130 million [1]. Non-pharmacological interventions provide efficient alternative strategies for improving Behavioural and Psychological Symptoms of Dementia (BPSD), as well as the quality of life of the older persons with NCDs; they improve cognition and mood disorders [2] and also facilitates the care process [3]. The environment for such non-pharmacological interventions plays an important role in enhancing their effectiveness [4,5]. Multimodal interventions based on Information and Communication Technology (ICT) has been an emerging practice in recent years for people with NCDs [6]. Designed for care facilities, the SENSE-GARDEN spaces are self-contained physical rooms where digital technology is used to create immersive emotional experiences [7]. The novelty of the method consists in the use of ICT based system to offer visual, audio, touch, olfactive and proprioceptive stimuli in a smooth cognitive flow and a complex experience, for a complex and personalized cognitive and physical training. The intervention is based on emotional reconnection, used to enable the improvement of self and reality orientation.
Methodology
The objective of the present study is to assess the impact of a personalized, innovative multimodal intervention in regards to the well-being of older adults living with major neurocognitive disorders.
Study design
This study is a case series. Study’s International registered report identifier is DERR1-10.2196/14096. SENSE-GARDEN study protocol is published elsewhere [8].
Participants
The participants for this study were recruited from inpatients at the Neurological Rehabilitation Department of Elias University Hospital, presenting neurocognitive disorders. Inclusion criteria: age 55+, Clinical Dementia Rating Score: 2 or 3, signed informed consent form. Exclusion criteria: mood disorders, other psychiatric diagnoses, changes in medication for NCD or cardiovascular disease in the last 3 months, extreme frailty, inability to perform the tasks due to physical disabilities.
Assessment tools and schedule
Relevant parameters were assessed at T0 - baseline, before the start of the intervention; T1 - after the 20 sessions (4 weeks after T0), at the end of the intervention program; T2 - follow-up (8 weeks after T0) [8]. In regards to the evaluation of the impact of the intervention program, a mixed evaluation methodology was applied. Standard quantitative assessment tools were applied to all domains of human functioning, based on the International Classification of Functioning (ICF) framework and domains [9]. All screening and evaluation sessions were conducted by 2 clinician psychologists, in part by means of remote video-audio communication, as adaptation to the special situation generated by the COVID-19 pandemic and the requirements regarding disease prevention and spreading reduction.
Intervention space and time coordinates
The study was performed between August 2019 and December 2020, in the Neurological Rehabilitation Department of the Elias University Emergency Hospital in Bucharest, Romania.
Intervention
An intensive multimodal intervention was applied, through an innovative technology that associates reminiscence therapy with multisensory stimulation, perception, space retrieval training, memory and executive function training as well as physical training elements. The equipment included a computer providing an innovative ICT-based technical platform ensuring the integration of the user-technology interfaces, a tablet for remote control of the therapeutic experiences, a short-throw interactive projector, an All-in-One PC and a four-limb stationary bicycle. The application on the tablet offers the means to create personal profiles and workflows. It also offers the therapist the possibility to give real time feedback to the system.
The SENSE-GARDEN space within the Elias Hospital is a rectangular room with an area of about 30sqm. The elongated shape of this space is conductive, enhancing a linear, possibly sequential or, conversely, complete traversal approach of the different experiences in SENSE-GARDEN. The space benefits from natural lighting almost entirely on one of the long sides. The walls have neutral colour, white. In the SENSE-GARDEN space, the participants were actively involved in a succession of different emotional reminiscence experiences used as base for reconnection and cognitive and physical training. Sessions lasted from 60 to 90 minutes, depending on the level of deficit of each patient, in addition to the usual rehabilitation program (physical modalities for musculoskeletal symptoms for 4 participants, physical therapy for 5 participants). No other intervention aiming to improve cognitive or emotional functioning was applied to participants during the study.
The therapeutic process was conducted by one clinical psychologist. One family caregiver was invited to participate in the SENSE-GARDEN sessions.
Ethical approval
All aspects regarding ethics of research and development of technologies and therapeutic interventions for people presenting NCDs, personal data protection during intervention and results processing, as well as safety aspects for all participants were taken into account [10]. The study had the approval of the Ethics Commission in Elias University Emergency Hospital, Bucharest, Romania (number 8223/ 09 November 2018). Written consent was obtained from all participants - people with NCDs (primary users) and family caregivers (secondary users). All personal data and parameters were pseudonymized for data processing.
Statistical analysis
Statistical analysis was performed using version 3.6.2 of R programming language. Tables were produced in Excel - Microsoft 365 for Enterprise package. To assess whether the data within a sample were normally distributed or not, the Shapiro-Wilk test was used, with a significance threshold of 0.05. For the comparison of paired sample (T1 - T0), we used paired t-test when data were normally distributed. For non-normally distributed data, Wilcoxon signed ranks sum test was applied.
Results
There were 8 participants enrolled. 1 participant had to withdraw after 2 sessions, due to deterioration of health condition not related to the intervention. All the remaining 7 participants completed 20 individual personalised sessions of the SENSE-GARDEN intervention as well as all three assessment sessions (T0, T1 and T2).
Demographic data
The mean age of participants was 71.14 years old (standard deviation of 12.17 years). The sample included 5 females and 2 males. All participants were rated 2 on the Clinical Rating Dementia Scale, indicating significant cognitive decline (3 with vascular major NCD, 2 with major NCD due to Alzheimer’s disease, 2 with major NCD due to mixed aetiology) and presented with sensory profile scores in with the range of their age group. One of the participants was wheelchair user.
Health and functioning related outcomes
The participants showed improvements in all parameters considered (Figure 1).
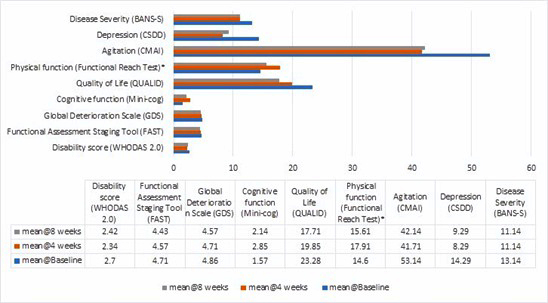 Figure 1: Health and functioning related outcomes (means).
Figure 1: Health and functioning related outcomes (means).
Note: WHODAS 2.0 = World Health Organization Disability Assessment Scale 2.0; FAST = Functional Assessment Staging Tool; GDS = Global Deterioration Scale; QUALID = Quality of Life in Late-Stage Dementia Scale; FRT = Functional Reach Test; CMAI = Cohen-Mansfield Agitation Inventory; CSDD = Cornell Scale for Depression in Dementia; BANS-S = Bedford Alzheimer Nursing Scale – Severity. *Based on 6 participants. One participant was unable to perform the test due to being a wheelchair user.
- Cognitive functions
The average score on the GDS decreased after 4 weeks of SENSE-GARDEN use, indicating a reduction in cognitive decline. The average score decreased after the control period. Mini-Cog scores showed improvements at the end of the intervention programme, but also a slight decrease at the follow-up.
- Physical functioning
Average scores indicate an improvement in physical function after 4 weeks of SENSE-GARDEN use. Scores decreased at follow-up.
- Agitation
On average, CMAI scores decreased from 53.14 to 41.71 after 4 weeks of intervention, indicating a reduction in agitation. The average score slightly increased to 42.14 after the control period.
- Depression
CSDD scores dropped on average from 14.29 to 8.29 after 4 weeks of intervention. This suggests that SENSE-GARDEN may be an effective intervention for reducing depression amongst people with major NCDs.
- Disease severity
On average, BANS-S scores decreased after using SENSE-GARDEN for 4 weeks, indicating a reduction in disease severity. The average score remained stable after 4 weeks of control period, indicating that participating in the intervention may have a lasting effect.
- Functional level and ability to carry out activities of daily living
On average, there was a slight decrease in FAST scores after 4 weeks of SENSE-GARDEN use, indicating an improvement in the participants’ level of functioning. The intervention may have lasting effects on the level of functioning amongst people with major NCDs.
- Disability level
On average, WHODAS 2.0 scores decreased indicating an improvement in functioning. However, the average score slightly increased after the control period, indicating a slight decline in functioning [11], after the intervention program stopped.
- Quality of life
QUALID scores decreased, indicating a higher perceived quality of life. Furthermore, in some cases, the average score continues to decrease after the control period, suggesting that the SENSE-GARDEN intervention may offer a beneficial long-term effect on quality of life.
- Statistical significance of results
As shown in table 1, important indicators of quality of life (perceived disability, cognition, physical ability, mood and behaviour) suffered changes with statistical significance after the intervention program, at T1 (significance threshold at .05). V-statistic is the sum of ranks assigned to the differences with positive signs. When running a Wilcoxon Signed Rank test, R calculates a sum of negative ranks and a sum of positive ranks. V is the positive ranks related value. The changes after the intervention differ on individual basis. Some benefits of the intervention seem to be maintained even at 8 weeks follow up, in a statistically significant manner.
|
Indicator |
baseline vs. 4 weeks |
baseline vs. 8 weeks |
4 weeks vs. 8 weeks |
|||
|
WHODAS |
V = 26 |
p-value = 0.05191 |
V = 23 |
p-value = 0.1508 |
V = 13 |
p-value = 0.9326 |
|
mini_cog |
V = 0 |
p-value = 0.05447 |
V = 1.5 |
p-value = 0.5862 |
V = 13 |
p-value = 0.1675 |
|
QUALID |
V = 25 |
p-value = 0.07593 |
V = 21 |
p-value = 0.03552 |
V = 19 |
p-value = 0.4436 |
|
FRT |
V = 1 |
p-value = 0.05917 |
V = 6 |
p-value = 0.4017 |
V = 17 |
p-value = 0.2084 |
|
FAST |
V = 4 |
p-value = 0.7728 |
V = 3 |
p-value = 0.3458 |
V = 1 |
p-value = 1 |
|
GDS |
V = 1 |
p-value = 1 |
V = 3 |
p-value = 0.3458 |
V = 1 |
p-value = 1 |
|
CMAI |
V = 28 |
p-value = 0.02201 |
V = 28 |
p-value = 0.02249 |
V = 13 |
p-value = 0.932 |
|
CSDD |
V = 21 |
p-value = 0.03603 |
V = 21 |
p-value = 0.03401 |
V = 3 |
p-value = 0.5839 |
|
BANSS_S |
V = 15 |
p-value = 0.05447 |
V = 10 |
p-value = 0.08897 |
V = 6 |
p-value = 0.8539 |
Table 1: Statistical significance of changes in the scores related to health and functioning.
Discussion
The results show a positive impact of the intensive multimodal intervention pro-posed, addressing multiple modifiable risk factors influencing cognitive decline. The results are in line with the conclusion of a recent systematic review on multimodal interventions [12]. Intensive personalised rehabilitation interventions are beneficial in terms of functioning and attaining desired goals [13]. The changes in the scores related to health and functioning after the intervention show statistical significance, even if the lot was small and the group is not homogenous. This suggests that the intervention programme is effective.
The improvement of CSDD score from 14,29 to 8,29 after intervention indicates an important improvement of mood, as a score > 10 indicates a probable major depressive episode and a score >18 definite major depressive episode, while a score below 6 is associated with absence of significant depression [14]. The changes in CSDD score are consistent with those on CMAI.
The average reduction of WHODAS score from 2.7 (moderate disability) to 2.34 (moderate-mild disability) indicates a better relationship with the environment as result of improved awareness and engagement. A better performance is noted in all activity domains assessed with WHODAS instrument: cognition, mobility, self-care, coping, home and professional activities as well as participation [15]. Slight reduction of average scores is noticed on both scales developed by Reisberg, defining the level of the person’s functioning deficit (Functional Assessment Staging Tool and Global Deterioration Scale).
The results of the present study in regards with physical and cognitive functioning consensual changes are in accord with the data from the literature. The distance in FRT has improved from an average of 14 cm to an average of 17 cm, which means changing the classification (averages) from the category of people with a very high risk of falling (less than 15 cm - risk of falling is 4 times higher than usual) in the category of people with medium risk of falling (15-25 cm, risk of falling is twice as high as normal) [16].
The environment in which the intervention is offered to the user is important. The space used for intervention delivery in this study has been prepared in regards to size, shape, interior design and equipment to meet the needs of the different experiences, in terms of dementia friendly principles [17,18] as well as for safe and efficient sensory-motor and visuo-spatial training [19]. The symptoms can be increased by inappropriate space size, shape, flow, colours or textures, lighting being too bright or insufficient, and by sounds difficult to interpret or misunderstood [20]. At the same time, a dementia-friendly design can alleviate some of BPSD such as wandering, spatial and temporal disorientation [21]. People with neurocognitive disorders need a higher level of lighting [22] but glare and shadows must be avoided. The lighting of the space was an important aspect, enhancing the 6 experiences depending on the type of training and the time of day. It was taken into account that natural light fights depression [23] but, at the same time, artificial light helps a good focus on different activities.
There are limitations to this study. Because of the limited number of participants, the results need to be validated in other studies with larger lot and a control group or a baseline trend to compare natural progression of functioning, activity and participation with the outcome of the intervention period.
Conclusion
The results of this study provide a comprehensive picture of the impact a cognitive, emotional and physical multimodal intervention has on persons with major NCD, when applied intensively by means of an ICT based system. Improvements have been documented in regards of cognitive and physical functioning, as well as in emotional condition, behaviour and quality of life. Continuous active engagement of the people with major NCD as well as continuous adaptation of the intervention are needed in order to provide sustained benefits. Further research is required to determine the optimal combination of stimuli able to provide users with the best experience and most benefits, as well as to determine the best means for evaluating the impact of complex multimodal interventions in neurocognitive disorders.
Author Contributions
IC, AGM, MVZ, AI, RD, GG, JAS, MB: conceived and designed the study. MB, MNP, GG: critical review of paper. IC, AGM, JAS, MB: intervention design. IC, AGM, AI, MVZ, MZ, RD, MB: writing of paper, analysis, interpretation of findings, and conducting literature searches. IC, AGM: intervention program, data collection and quality measure. IC, AGM, MZ, MB: space requirements, setting and navigation design. MNP and MB: inclusion and exclusion process. All authors contributed to the article and approved the submitted version.
Acknowledgment
We would like to thank the members of the SENSE-GARDEN project team, to all the participants in our studies and to Mrs Roxana Popa, who helped us with the statistical analysis.
Funding
This research was funded by the European Commission through the EU Active and Assisted Living Programme, Project “Virtual and memory adaptable spaces creating stimuli for the senses in ageing people with dementia” - SENSE-GARDEN (AAL/Call2016/054-b/2017), with implementation period June 2017 - November 2020) co-funded by the European Commission and National Funding Authorities of Norway, Belgium, Romania and Portugal.
Conflicts of Interest
All authors are members of the SENSE-GARDEN project, AAL/Call2016/054-b/2017. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Commission in Elias University Emergency Hospital, Bucharest, Romania (decision number 8223/ 09 November 2018).
Informed Consent Statement
Informed consent was obtained in written form from all participants involved in the study (publication of study results included).
Data Availability Statement
Data are available at the corresponding authors, by request. For more details regarding SENSE-GARDEN, one may access also the project’s website: https://sense-garden.eu.
References
- Chan KY, Adeloye D, Asante KP, Calia C, Campbell H, et al. (2019) Tackling dementia globally: The Global Dementia Prevention Program (GloDePP) collaboration. J Glob Health 9: 020103.
- Marin AG, Ciobanu I, Zamfir MV, Mikolajczyk T, Berteanu M (2017) Work Protocol for Cognitive Optimization Intervention Using Computer Applications in Patients with Cognitive Impairment after Stroke. International Journal of Modeling and Optimization 7: 245-250.
- Berg-Weger M, Stewart DB (2017) Non-Pharmacologic Interventions for Persons with Dementia. Mo Med 114: 116-119.
- Trivedi DP, Braun A, Dickinson A, Gage H, Hamilton L, et al. (2019) Managing behavioural and psychological symptoms in community dwelling older people with dementia: 1. A systematic review of the effectiveness of interventions. Dementia (London) 18: 2925-2949.
- de Oliveira AM, Radanovic M, de Mello PC, Buchain PC, Vizzotto AD, et al. (2015) Nonpharmacological Interventions to Reduce Behavioral and Psychological Symptoms of Dementia: A Systematic Review. Biomed Res Int 2015: 218980.
- Goodall G, Taraldsen K, Serrano JA (2021) The use of technology in creating individualized, meaningful activities for people living with dementia: A systematic review. Dementia 20: 1442-1469.
- Serrano JA (2021) SENSE-GARDEN – A concept and technology for care and well-being in dementia treatment. IET - The Institution of Engineering and Technology. In: Ray PK, Liaw S-T, Serrano JA (eds.). Digital Methods and Tools to Support Healthy Ageing. Healthcare Technologies. Pg no: 360.
- Goodall G, Ciobanu I, Taraldsen K, Sørgaard J, Marin A, et al. (2019) The Use of Virtual and Immersive Technology in Creating Personalized Multisensory Spaces for People Living With Dementia (SENSE-GARDEN): Protocol for a Multisite Before-After Trial. JMIR Res Protoc 8: 14096.
- Maki Y, Sakurai T, Okochi J, Yamaguchi H, Toba K (2018) Rehabilitation to live better with dementia. Geriatr Gerontol Int 18: 1529-1536.
- Ciobanu I, Marin AG, Draghici R, Goodall G, Anghelache I, et al. (2019) Safety Aspects In Developing New Technologies For Reminiscence Therapy: Insights From The SENSE-GARDEN Project. Rom J Gerontol Geriatr 8: 3-8.
- Hopper T (2007) The ICF and dementia. Semin Speech Lang 28: 273-282.
- Chalfont G, Milligan C, Simpson J (2020) A mixed methods systematic review of multimodal non-pharmacological interventions to improve cognition for people with dementia. Dementia (London) 19: 1086-1130.
- Wade DT (2020) What is rehabilitation? An empirical investigation leading to an evidence-based description. Clin Rehabil 34: 571-583.
- Alexopoulos GS, Abrams RC, Young RC, Shamoian CA (1988) Cornell Scale for Depression in Dementia. Biol Psychiatry 23: 271-284.
- Federici S, Bracalenti M, Meloni F, Luciano JV (2017) World Health Organization Disability Assessment Schedule 2.0: An International Systematic Review. Disabil Rehabil 39: 2347-2380.
- Weiner DK, Duncan PW, Chandler J, Studenski SA (1992) Functional reach: A marker of physical frailty. J Am Geriatr Soc 40: 203-207.
- Marquardt G, Johnston D, Black BS, Morrison A, Rosenblatt A, et al. (2011) Association of the spatial layout of the home and ADL abilities among older adults with dementia. Am J Alzheimers Dis Other Demen 26: 51-57.
- Marquardt G, Viehweger A (2015) Architecture for people with dementia planning principles, practices and future challenges. Dresden Saxon State Library, Dresden, Germany.
- Assed MM, Rocca CCA, Garcia YM, Khafif TC, Belizario GO, et al. (2020) Memory training combined with 3D visuospatial stimulus improves cognitive performance in the elderly: Pilot study. Dement Neuropsychol 14: 290-299.
- Zamfir M, Marin A, Ciobanu I, Bogdan DC, Zamfir MV (2020) The concept of Dementia Enabling Built Environment from an interdisciplinary perspective. Argument no.12/2020: 95-122.
- Marquardt G, Schmieg P (2009) Dementia-Friendly Architecture: Environments That Facilitate Wayfinding in Nursing Homes. Am J Alzheimers Dis Other Demen 24: 333-340.
- Dewing J (2009) Caring for people with dementia: Noise and light. Nurs Older People 21: 34-38.
- McNair D, Pollock R, Cunningham C (2019) Enlighten: Lighting for Older People and People with Dementia. La Vergne: Hammond Cre Media, Australia.
Citation: Ciobanu I, Draghici R, Marin AG, Zamfir M-V, Iliescu A, et al. (2022) Case Series of an ICT-Based Multimodal Intervention Program for People with Major Neurocognitive Disorders: The SENSE-GARDEN Project. J Gerontol Geriatr Med 8: 137.
Copyright: © 2022 Ileana Ciobanu, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

