
Challenging Neurological Manifestations in Large-Cell Neuroendocrine Carcinoma (LCNEC): A Case Study of Extensive Intracranial and Intradural Metastases
*Corresponding Author(s):
Julia MahlerDepartment Of Neurosurgery, Cantonal Hospital Of Winterthur, Winterthur, Switzerland
Email:neurochirurgie@ksw.ch
Abstract
This case study explores the challenging neurological manifestations in a 59-year-old female diagnosed with large-cell neuroendocrine carcinoma (LCNEC). The patient initially presented with aphasia, which led to the discovery of an intracranial cystic-necrotic metastasis. Despite surgical and aggressive radio-chemotherapy treatments, her condition progressed to extensive leptomeningeal carcinomatosis (LMC) and intradural spinal metastases. This resulted in right dominant paraparesis, saddle hypesthesia, and urinary incontinence, developing into paraplegia even after emergency radiotherapy of the complete spine. The unprecedented extent of LCNEC metastases in both intracranial and intraspinal regions raises important considerations for diagnostic assessment in neuroendocrine tumors with neurological symptoms. Despite aggressive intervention, the prognosis remains poor, emphasizing the challenges in managing advanced LCNEC stages with widespread metastases.
Keywords
Intradural metastases; Intracranial metastases; Large-cell neuroendocrine carcinoma
Introduction
Large-cell neuroendocrine carcinoma (LCNEC) is a rather rare lung tumor. Little data is available on the diagnosis and treatment of advanced stages in particular. This tumor usually metastasizes isolated to the lungs, brain, liver or bones or combined as multiorgan metastases [1]. Extensive metastasis to the entire nervous system, intracranial and intraspinal, has not yet been described.
Case Presentation
A 59-year-old female with LCNEC presented with progressive neurological symptoms, leading to a comprehensive re-evaluation. Initially, an intracranial cystic-necrotic metastasis in the left frontal lobe was identified (Figure 1), correlating with new-onset aphasia and confusion. Post-surgical analysis confirmed high-proliferation LCNEC, positive for synaptophysin, chromogranin A, CD56, and RB1 wild type. Primary lung involvement was evident in the right upper lobe. Despite cisplatin and etoposide-based radio-chemotherapy, extensive neurocranial and leptomeningeal carcinomatosis (LMC) developed (Figure 2). Whole-brain irradiation (10 x 3Gy) was administered as palliation. By October 2023, the patient experienced right dominant paraparesis, saddle hypesthesia, urinary incontinence, and weakened sphincter function. MRI revealed extensive intradural LMC, compressing the cauda equina at the L4/L5 level (Figure 3). Emergency radiotherapy (Th12-S1, 10 x 3Gy) was initiated, with extended coverage to C1-Th11. Initial improvement was noted; however, the patient's condition progressed to paraplegia.
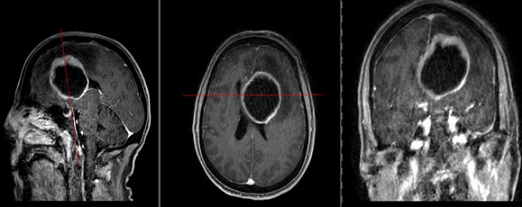 Figure 1: T1-weighted MRI of the skull with contrast agent (sagittal, axial, and coronal views). The image reveals a cystic mass in the left frontal lobe, accompanied by a pronounced midline shift toward the opposite side.
Figure 1: T1-weighted MRI of the skull with contrast agent (sagittal, axial, and coronal views). The image reveals a cystic mass in the left frontal lobe, accompanied by a pronounced midline shift toward the opposite side.
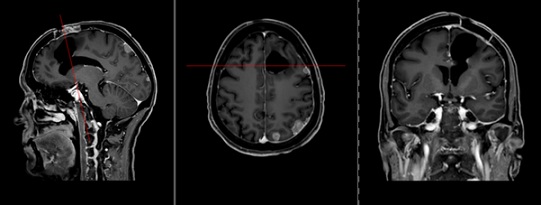 Figure 2: T1-weighted MRI of the skull with contrast agent (sagittal, axial, and coronal views). There is a pre-existing resection cavity in the left frontal lobe. Multiple intracerebral metastases are noted, including in the left frontal medial gyrus, left parietal gyrus, left precuneus, and left temporal gyrus. Increased dural enhancement is observed in the left parietal and frontal regions, indicative of leptomeningeal carcinomatosis.
Figure 2: T1-weighted MRI of the skull with contrast agent (sagittal, axial, and coronal views). There is a pre-existing resection cavity in the left frontal lobe. Multiple intracerebral metastases are noted, including in the left frontal medial gyrus, left parietal gyrus, left precuneus, and left temporal gyrus. Increased dural enhancement is observed in the left parietal and frontal regions, indicative of leptomeningeal carcinomatosis.
 Figure 3: T2-weighted MRI of the complete spine (cervical, thoracic, and lumbar in sagittal view). Extensive intradural leptomeningeal tumor spread is evident.
Figure 3: T2-weighted MRI of the complete spine (cervical, thoracic, and lumbar in sagittal view). Extensive intradural leptomeningeal tumor spread is evident.
Discussion
The rarity of extensive intracranial and intraspinal LCNEC metastases is underscored by the literature, with only isolated cases of singular intraspinal lesions reported previously [2,3]. Yang et al. detailed a case with limited intraspinal and intracranial involvement [4]. In contrast, our patient exhibited widespread metastatic dissemination in both regions, a presentation not yet documented in LCNEC cases. Dural space metastases in LCNEC are notably infrequent, lacking substantial incidence data. This contrasts with the relatively higher occurrence of intracranial metastases, reported in up to 47% of advanced stages [5]. The initial presentation of intracranial metastasis in our case, followed by extensive leptomeningeal and intraspinal spread, suggests a progression pattern via cerebrospinal fluid and leptomeningeal invasion, potentially exacerbated post-surgically [6].
Prognostically, LCNEC with metastases portends a grim outlook [1]. Median survival rates are low, with brain metastases linked to a six-month expectancy and further reduced by multiorgan involvement [1]. Even with aggressive treatment, survival rarely extends beyond a few months, especially in lung cancer with LMC. Our patient’s survival, exceeding four months post-intracranial LMC diagnosis and two months following intraspinal metastasis detection, is still within the poor prognosis range.
Conclusion
This case of LCNEC with extensive intracerebral and spinal intradural metastasis underscores the need for thorough diagnostic assessment in neuroendocrine tumors presenting with neurological symptoms. The findings prompt consideration of complete neuraxis imaging upon detecting significant intracranial anomalies. Early, intensive intervention may offer marginal life expectancy benefits, with generally poor prognoses in advanced LCNEC stages.
References
- Jiang T, Sun H, Li N, Jiang T (2023) Metastasis pattern and prognosis of large cell neuroendocrine carcinoma: a population-based study. J Cancer Res Clin Oncol. 149: 13511-13521.
- Blondet E, Dulou R, Camparo P, Pernot P (2005) Lumbar intradural metastasis of a primary carcinoid tumor of the lung. Case illustration. J Neurosurg Spine. 2: 231.
- Tsimpas A, Post NH, Moshel Y, Frempong-Boadu AK (2010) Large cell neuroendocrine carcinoma of the lung metastatic to the cauda equina. Spine J. 10: e1-e5.
- Yang G, Pan Z, Ma N, Qu L, Yuan T, et al. (2017) Leptomeningeal metastasis of pulmonary large-cell neuroendocrine carcinoma: A case report and review of the literature. Oncol Lett. 14: 4282-4286.
- Naidoo J, Santos-Zabala ML, Iyriboz T, Woo KM, Sima CS, et al. (2016) Large Cell Neuroendocrine Carcinoma of the Lung: Clinico-Pathologic Features, Treatment, and Outcomes. Clin Lung Cancer. 17: e121-e129.
- Le Rhun E, Taillibert S, Chamberlain MC (2013) Carcinomatous meningitis: Leptomeningeal metastases in solid tumors. Surg Neurol Int. 4: S265-S288.
Citation: Mahler J, Halatsch ME, Alfieri A (2024) Challenging Neurological Manifestations in Large-Cell Neuroendocrine Carcinoma (LCNEC): A Case Study of Extensive Intracranial and Intradural Metastases. J Clin Stud Med Case Rep 11:225
Copyright: © 2024 Julia Mahler, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

