
Chronic Leg Swelling and Venous Ulcer as a Late Complication of Post-Traumatic Arteriovenous Fistula: A Case Report
*Corresponding Author(s):
José Maciel Caldas Dos ReisDivision Of Vascular Surgery, AORN Dei Colli, Clinic Hospital, Belém, Pará, Brazil
Tel:+55 9140052551,
Email:macielreis.angiovasc@gmail.com
Abstract
Chronic post-traumatic arteriovenous fistula is a late complication of vascular injury and presents symptoms of venous hypertension and ulceration, as well as congestive heart failure in advanced stages. We present rare case of chronic leg swelling and ulceration in an adult caused by post-traumatic arteriovenous fistula.
Keywords
Arteriovenous fistula; Popliteal artery; Trauma
INTRODUCTION
An Arteriovenous Fistula (AVF) is an abnormal communication between an artery and a vein, caused by different vascular injuries. It was first described as a medical entity by William Hunter in 1757, followed by the first attempted surgical correction in 1837 by Breschet [1,2].
Post-traumatic AVF is a well-described phenomenon, associated with bone fractures, penetrating or high-injury blunt trauma and sport activities, and less frequently with post-orthopedic injuries. The clinical presentation and interval between trauma and the diagnosis of AVF can vary, even up to decades after injury in some cases [2,3]. Treatment options include endovascular intervention, artery ligation or reconstruction, hybrid procedure, coil embolization, or echo-guided thrombin injection [2-4].
The clinical manifestations of AVF are steal phenomenon, congestive heart failure, or distal ischemia, which have been reported to occur anywhere from a few weeks or months to more than 50 years after the injury. Ischemia and skin ulceration may occur due to blood stealing through the fistula and venous insufficiency, but this is a very rare cause of leg ulcer [5-7].
CASE PRESENTATION
A 42-year-old male caucasian patient had a complaint of pain, ulceration, and swelling in the right leg. He had suffered from a penetrating gunshot injury in the right knee 12 years ago. Traumatic AVF was detected 10 years ago, but he did not undergo any treatment due to difficulty in hospitalization. In the last 7 years, his symptoms were leg pain and exaggerated swelling with sudden open ulceration on the leg. Physical examination revealed increased diameter of the right lower extremity (Figure 1), thrill on the right femoral region, and presence of a distal pulse. Duplex scan examination revealed the presence of an AVF arterial flow in the venous structures. Digital subtraction angiography revealed an AVF between the popliteal artery and popliteal vein (Figure 2). Iliac, common femoral and superficial femoral arteries were aneurysmatic, and the flow of the arteries distal to the fistula had reduced diameter and velocity.
 Figure 1: A foul-smelling, irregularly-shaped ulcer seen pre-operatively, covered with yellowish necrosis in part of the leg with black eschar in the periphery.
Figure 1: A foul-smelling, irregularly-shaped ulcer seen pre-operatively, covered with yellowish necrosis in part of the leg with black eschar in the periphery.
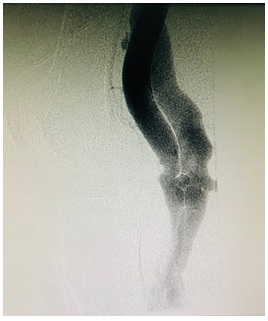 Figure 2: Digital subtraction angiography reveals arteriovenous fistula between the popliteal Artery (A) and popliteal Vein (V).
Figure 2: Digital subtraction angiography reveals arteriovenous fistula between the popliteal Artery (A) and popliteal Vein (V).
After adequate pre-operative examinations, the patient was prepared for surgery and the site of injury was accessed. The wound was deep and the fistula was found between the popliteal artery and vein. While approaching the site of the AVFs, the artery was accessed both proximally and distally. Following systemic heparinization (100 IU/kg), arterial and venous clamps were placed both proximally and distally. With occlusion of the proximal and distal ends of the vessels, the artery and vein were separated and the fistula was closed using 5-0 Prolene sutures. The postoperative course was very smooth and the patient's symptoms of edema and ulceration improved (Figure 3).
 Figure 3: Right leg during follow-up after 2 months.
Figure 3: Right leg during follow-up after 2 months.
The patient had no postoperative venous thrombosis, and he was discharged after 6 days without any complications. During follow-up, success of the surgery and healing of the AVF was checked using Doppler ultrasound, 30 days postoperatively.
DISCUSSION
Vascular injury is found in 1.6-4.4% of all general trauma admissions and is more common in males [8]. It is complicated by AVFs in 5% of the cases and can occur in different parts of the body [2,5-7]. The lower extremities are usually involved due to several types of trauma, and post-traumatic AVFs have been reported in the femoral, popliteal, and infrapopliteal regions, commonly associated with a pseudoaneurysm [5-7]. More than half of all traumatic AVFs occur in the lower extremities, and the most common etiological factors include gunshot injuries, penetrating injuries, or fractures [1,2].
Late complications of AVF include arterial and venous dilatation, distal ischemia, venous congestion, and congestive heart failure [5-7]. Although AVF complicated by leg ulceration has been reported after popliteal or tibial AVF causing venous congestion, our patient did not have the blood steal syndrome, but there was increased diameter of effected vessels with normal echocardiography findings [3,6-8].
The clinical diagnosis of AVF is made by clinical examination, but some cases have been reported weeks, months, or years after the trauma episode. A thorough investigation is necessary when managing patients with trauma involving vascular structures. In this case, the clinical findings of chronic venous insufficiency that indicated the diagnostic hypothesis of AVF were thrill, swelling, and right knee murmur [6-9].
Duplex ultrasonography represents a non-invasive investigation method with some utility in the diagnosis of traumatic AVFs, which demonstrates the characteristic flow patterns in the popliteal arterial and venous system [4,6,10,11]. Digital subtraction angiography confirmed the diagnosis and showed lateral-lateral AVF established between the popliteal artery and vein. No pseudoaneurysm was found.
The management of venous leg ulcers is complex and the first option was compression therapy but minimal result in our case. The endovascular repair enables a less traumatic anatomic reconstruction of such lesions [4-6]. Open surgery is the obligatory and safe method where the endovascular approach is impossible [8,9]. Open surgical repair with direct ligation of the injured vessel or reconstruction of the vessel wall can be challenging due to the elevated venous pressure and surrounding inflammation [6,8-11]. However, in this particular case, direct vision and surgical repair of the AVF was our first choice, because the patient’s condition was stable and we were in a public hospital with some difficulties in obtaining materials for endovascular procedures.
The present case represents a rare clinical presentation of a large chronic right groin AVF, 12 years after a gunshot wound, and demonstrates the successful surgical repair of this complex long-standing traumatic AVF. This case report describes a traumatic femoral AVF causing distal venous ulceration 7 years after the injury, where the ulcer healed at 2 months, and had not recurred at 6 months follow-up.
CONCLUSION
AVF should be considered in trauma involving vascular structures, especially after any penetrating trauma, particularly ballistic injuries. Clinical features can be atypical, but therapeutic management should be initiated as soon as possible.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.editage.com) for English language editing.
CONFLICT OF INTEREST STATEMENT
The authors declared no conflicts of interest.
FUNDING
The authors have no sources of funding to report.
REGISTRATION OF RESEARCH STUDIES
N/A.
ETHICAL APPROVAL
This is a case report study; no ethical approval was needed
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
REFERENCES
- Sahin M, Yücel C, Kanber EM, ?lal Mert FT, B?çakhan B (2018) Management of traumatic arteriovenous fistulas: A tertiary academic center experience. Ulus Travma Acil Cerrahi Derg 24: 234-238.
- Kalender M, Baysal AN, Dagli M, Gokmengil H (2016) Chronic leg swelling and palpitation as a late complication of post-traumatic arteriovenous fistula: A case report. Trauma Case Rep l: 16-20.
- Góes Junior AMO, Jeha SAH, Franco RSM (2014) Tratamento híbrido para fístula arteriovenosa entre vasos poplíteos. J Vasc Bras 13: 325-329.
- Mylankal KJ, Johnson B, Ettles DF (2011) Iatrogenic arteriovenous fistula as a cause for leg ulcers: A case report. AnnVasc Dis 4: 139-142.
- Lebreton G, Uzel AP, Celerien J, Roques F, Deneuville M (2010) Popliteal arteriovenous fistula due to a gunshot injury. Ann Vasc Surg 24: 17- 21.
- Rabellino M, Shinzato S, Aragón-Sánchez J, Peralta O, Marenchino R, et al. (2012) Leg ulcer as a complication of a posttraumatic tibial arteriovenous fistula treated by endovascular approach with stent-graft placement. Int J Low Extrem Wounds 11: 147-151.
- Zizi O, Naouli H, Jiber H, Bouarhroum A (2017) Post-traumatic concomitant popliteal artery pseudoaneurysm and arteriovenous fistula. J Med Vasc 42: 46-49.
- Young CJ, Dardik A, Sumpio B, Indes J, Muhs B, et al. (2015) Venous ulcer: Late complication of a traumatic arteriovenous fistula. Ann Vasc Surg 29: 836.
- Isoda H, Shimauchi T, Ogaki T, Nagano I, Baba H, et al. (2006) Stasis ulcer and dermatitis caused by artificial arteriovenous fistula created 33 years previously for the treatment of poliomyelitis. Clin Exp Dermatol 31: 470-472.
- Bokhabrine MK, Bouziane Z, Lahlou Z, Lekhal B, Bensaid Y (2010) Limb traumatic arteriovenous fistula: Experience of 26 cases. Ann Cardiol Angeiol 59: 67-71.
- Suknaic S, Erdelez L, Skopljanac A, Sef D, Novacic K (2012) Chronic ischaemic leg ulcer as a late complication of post-traumatic arteriovenous fistula. Phlebology 27: 124-127.
Citation: dos Reis JMC, Melo GS, Ribeiro FRCM, de Oliveira MV, Silva LP (2020) Chronic Leg Swelling and Venous Ulcer as a Late Complication of Post-Traumatic Arteriovenous Fistula: A Case Report. J Angiol Vasc Surg 5: 041.
Copyright: © 2020 José Maciel Caldas dos Reis, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

