
Comfort Levels of Physical Medicine & Rehabilitation Residents during Call: A Survey Study
*Corresponding Author(s):
Jane Hwang , MDDepartment Of Orthopaedic Surgery And Rehabilitation, Loyola University Medical Center, Illinois, United States
Tel:+1 7082164254,
Email:jane.hwang@lumc.edu
Abstract
There are few studies in the literature reviewing how comfortable residents are during call, especially in the field of Physical Medicine & Rehabilitation (PM&R). The aim of this study was to review how prepared residents feel during call as well as gather general information about residency call in the field of PM&R in the hope of improving the quality of call.
Methods
An anonymous online survey made up of 7 questions addressing level of comfort during call, reason for paging, level of training, type of internship was sent out to the ACGME PM&R programs in the United States/US territories.
Results
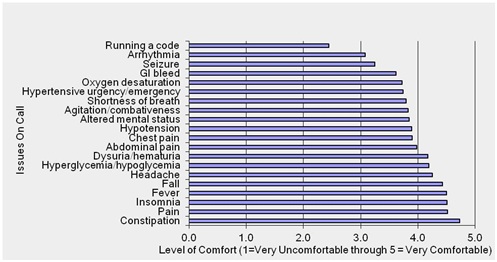
A total of 221 PM&R residents from at least 48 programs across 25 states/US territories participated in the survey. The top 3 reasons for which residents were getting paged during call were pain, abnormal vital signs, and bowel/bladder issues. The top 3 items residents were least comfortable with handling during call were running a code, arrhythmias and seizures. The top 3 items residents were most comfortable with were constipation, pain and insomnia. 50% of unique programs were found to take home call, 19% in-house call and 31% home and/or in-house call. 46% of residents completed their PGY-1 training in a preliminary medicine program, 36% in a transitional year program, 6% in a preliminary surgery program, and 12% in another type of program.
Conclusion
This study gives an idea of the common reasons why residents are getting paged during call and what residents feel comfortable and uncomfortable handling while on call. This information can better guide residency programs in regards to their educational conferences and improve the quality of PM&R residency call and ultimately patient care.
Keywords
INTRODUCTION
Although there is a fair amount of literature looking at residency call in other specialties, there has been little research in regards to residency call in the field of Physical Medicine and Rehabilitation (PM&R). The primary objective of this study was to look at resident comfort level during call in the field of PM&R; specifically looking at what residents are being paged about and how comfortable they feel handling common and uncommon issues that arise during call. The secondary objective was to look at if resident comfortability is correlated with the type of preliminary internship that was done and the Postgraduate Year (PGY) level. With more knowledge regarding what residents are being paged about and better preparation of residents, the hope of this study is to provide a smoother transition into residency call, improve the quality of call for all residents and ultimately improve patient care.
METHODS
|
Survey Questions |
|
1. How comfortable do you feel when handling the following issues while on call? * |
|
2. Please list any other issues not mentioned above that you felt uncomfortable dealing with while on call (FR). |
|
3. What are the top three issues you get paged about while on call? (FR) |
|
4. Do you take home call or in house call? |
|
5. What is your PGY level? |
|
6. If applicable, what type of internship did you complete? |
|
7. Name of your residency program (FR). |
* 20 issues listed: Fever, Pain, Fall, Hyperglycemia/Hypoglycemia, Hypertensive urgency/Emergency, Hypotension, Chest pain, Arrhythmia, Shortness of breath, Oxygen desaturation, Abdominal pain, Constipation, GI bleed, Dysuria/Hematuria, Headache, Seizure, Altered mental status, Agitation/Combativeness, Insomnia, Running a code.
Statistical analysis
RESULTS
|
Top Reasons for Getting Paged |
|
1. Pain |
|
2. Abnormal vital signs |
|
3. Bowel/Bladder issues |
|
4. Insomnia |
|
5. Blood sugars |
|
6. Agitation/AMS |
|
7. Falls |
|
Death of a patient |
|
“Anything pediatric” |
|
Autonomic dysreflexia |
|
Sympathetic storming |
|
Baclofen pumps |
|
Social issues and family questions |
|
Tube issues |
|
LVAD patients |
|
Cancer patients |
|
Reading EKGs |
In regards to the type of preliminary training year, there were statistically significant differences in comfort levels for arrhythmia, constipation and dysuria/hematuria (Table 5). Those residents trained in a preliminary medicine year were more comfortable handling the abovementioned issues followed by those trained in a transitional year followed by those trained in a preliminary surgical year. Although there were no other statistically significant differences in comfort levels across the remaining issues, there was a general trend with higher comfort levels seen in those trained in preliminary medicine.
|
Residency Call, n (%) |
Prelim. Medicine 99 (51.8%) |
Prelim. Surgery 14 (7.3%) |
Transitional Year 78 (40.8%) |
Total |
p |
|
(N=191) |
|||||
|
Fever |
96 (97.0%) |
12 (85.7%) |
72 (92.3%) |
180 (94.2%) |
0.09 |
|
Pain |
97 (98.0%) |
13 (92.9%) |
74 (94.9%) |
184 (96.3%) |
0.3 |
|
Fall |
92 (92.9%) |
12 (85.7%) |
72 (92.3%) |
176 (92.2%) |
0.64 |
|
Hyperglycemia/Hypoglycemia |
83 (84.7%) |
10 (71.4%) |
59 (75.6%) |
152 (80.0%) |
0.23 |
|
Hypertensive urgency/Emergency |
72 (72.7%) |
10 (71.4%) |
51 (65.4%) |
133 (69.6%) |
0.57 |
|
Hypotension |
80 (80.8%) |
9 (64.3%) |
57 (73.1%) |
146 (76.4%) |
0.26 |
|
Chest pain |
81 (81.8%) |
9 (64.3%) |
56 (71.8%) |
146 (76.4%) |
0.16 |
|
Arrhythmia |
48 (48.5%) |
3 (21.4%) |
26 (33.3%) |
77 (40.3%) |
0.04 |
|
Shortness of breath |
76 (76.8%) |
10 (71.4%) |
51 (65.4%) |
137 (71.7%) |
0.25 |
|
Oxygen desaturation |
70 (71.4%) |
9 (64.3%) |
50 (64.1%) |
129 (67.9%) |
0.56 |
|
Abdominal pain |
83 (83.8%) |
11 (78.6%) |
60 (77.9%) |
154 (81.1%) |
0.59 |
|
Constipation |
99 (100%) |
12 (92.3%) |
74 (96.1%) |
185 (97.9%) |
0.04 |
|
GI bleed |
64 (64.7%) |
7 (50.0%) |
45 (57.7%) |
116 (60.7%) |
0.45 |
|
Dysuria/Hematuria |
84 (84.9%) |
8 (57.1%) |
61 (79.2%) |
153 (80.5%) |
0.05 |
|
Headache |
92 (93.9%) |
11 (78.6%) |
70 (89.7%) |
173 (91.1%) |
0.15 |
|
Seizure |
48 (49.0%) |
5 (35.7%) |
33 (42.3%) |
86 (45.3%) |
0.51 |
|
Altered mental status |
74 (75.5%) |
8 (57.1%) |
56 (71.8%) |
138 (72.6%) |
0.35 |
|
Agitation/Combativeness |
68 (68.7%) |
9 (64.3%) |
51 (65.4%) |
128 (67.0%) |
0.88 |
|
Insomnia |
93 (94.9%) |
11 (84.6%) |
73 (94.8%) |
177 (94.2%) |
0.29 |
|
Running a code |
20 (20.6%) |
5 (38.5%) |
13 (17.3%) |
38 (20.5%) |
0.21 |
Valid N:
N=190 for the following residency calls: Hyperglycemia/Hypoglycemia, Oxygen desaturation, Dysuria/Hematuria, Headache, Seizure and Altered mental status.
Constipation (N=189)
Insomnia (N=188)
Running a code (N=185)
Comparing across training level, PGY-3’s and 4’s were found to be more comfortable handling hyperglycemia/hypoglycemia, hypotension, seizure, altered mental status and agitation/combativeness compared to their PGY-2 counterparts (Table 4). The difference in comfortability between the two groups was the largest in handling altered mental status with 81% of PGY-3’s and 4’s feeling comfortable handling altered mental status compared to 60.9% of PGY-2’s (p=0.003). The smallest difference in comfort level was for handling hyperglycemia/hypoglycemia with 84.3% of PGY-3’s and 4’s feeling comfortable compared to 72.5% of their PGY-2 counterparts (p=0.49). There were no other statistically significant differences in comfort levels across the remaining issues although higher comfortability was seen across all items in the senior residents.
|
Residency Call |
PGY-2 69 (36.1%) |
PGY-3 and PGY-4 122 (63.9%) |
Total |
p |
||
|
(N=191) |
||||||
|
Fever |
64 |
92.80% |
117 |
95.90% |
181 (94.8%) |
0.5 |
|
Pain |
66 |
95.70% |
119 |
97.50% |
185 (96.9%) |
0.669 |
|
Fall |
61 |
88.40% |
116 |
95.10% |
177 (92.7%) |
0.089 |
|
Hyperglycemia/Hypoglycemia |
50 |
72.50% |
102 |
84.30% |
152 (80.0%) |
0.049 |
|
Hypertensive urgency/Emergency |
43 |
62.30% |
90 |
73.80% |
133 (69.6%) |
0.098 |
|
Hypotension |
46 |
66.70% |
101 |
82.80% |
147 (77.0%) |
0.011 |
|
Chest Pain |
51 |
73.90% |
98 |
80.30% |
149 (78.0%) |
0.304 |
|
Arrhythmia |
25 |
36.20% |
53 |
43.40% |
78 (40.8%) |
0.33 |
|
Shortness of breath |
46 |
66.70% |
94 |
77.00% |
140 (73.3%) |
0.119 |
|
Oxygen desaturation |
44 |
63.80% |
87 |
71.90% |
131 (68.9%) |
0.244 |
|
Abdominal pain |
55 |
80.90% |
100 |
82.00% |
155 (81.6%) |
0.853 |
|
Constipation |
65 |
97.00% |
120 |
98.40% |
185 (97.9%) |
0.616 |
|
GI bleed |
40 |
58.00% |
76 |
62.30% |
116 (60.7%) |
0.557 |
|
Dysuria/Hematuria |
50 |
73.50% |
103 |
84.40% |
153 (80.5%) |
0.069 |
|
Headache |
63 |
91.30% |
111 |
91.70% |
174 (91.6%) |
0.918 |
|
Seizure |
23 |
33.30% |
63 |
52.10% |
86 (45.3%) |
0.013 |
|
Altered mental status |
42 |
60.90% |
98 |
81.00% |
140 (73.7%) |
0.003 |
|
Agitation/Combativeness |
38 |
55.10% |
92 |
75.40% |
130 (68.1%) |
0.004 |
|
Insomnia |
62 |
92.50% |
116 |
95.90% |
178 (94.7%) |
0.332 |
|
Running a code |
12 |
18.20% |
25 |
21.00% |
37 (20.0%) |
0.645 |
Table 4: Number of residents who feel comfortable handling different issues during call categorized by post graduate year.
N=190 for the following residency calls: Hyperglycemia/Hypoglycemia, Oxygen desaturation, Abdominal pain, Dysuria/Hematuria, Headache, Seizure and Altered mental status.
Constipation (N=189)
Insomnia (N=188)
Running a code (N=185)
DISCUSSION
It is important to note that the top issues reported were in response to a free response question and not by observation. An observational study reviewing home call in a PM&R residency showed that the top reasons for getting paged were new onset of symptoms, new lab values, general issues, and bowel/bladder [2]. Insomnia, pain, change in vital signs and falls were less frequent reasons for pages (<10%). This does not coincide with the data found in our study, however the observational study was done over a short period of time of 3 months and involved just 6 participants.
There have been different strategies suggested to improve the quality of call for residents. Harvey et al., suggested placing standard orders for bowel care as well as insomnia when a patient is admitted [3]. As bowel issues and insomnia were amongst the top five reasons PM&R residents were getting paged during call, standard orders upon admission would likely reduce the number of calls. Pain was the number one reason reported on the survey for why residents were being paged. As well as standard orders for bowel care and insomnia, implementing pain medications ahead of time could also reduce the number of unnecessary overnight pages. This would improve patient care as it would avoid any delays in getting medications to patients. Goldsmith and Melvin suggested incorporating “safety rounds” during didactics which entails 30 minute sessions every month to discuss on-call issues experienced by residents. The goal of this exercise was to learn from the experiences of others [4]. Another study looked at role playing among residents and fellows using common problems encountered while on home call for nursing homes. After this exercise, there was improvement in overall attitude and skills amongst residents and fellows, including comfort level in management of common problems [5]. Implementation of these strategies into PM&R residencies may improve the comfort level and preparedness for issues not commonly experienced by residents routinely during call.
STUDY LIMITATIONS
A strength of the study was the number of responses to the survey. The data collected was able to generate enough data to ensure statistical value for certain measures. There was good geographic representation as responses were across 25 US states and territories including Puerto Rico. Also, there was similar representation across PGY-levels except for PGY-1 which is as expected as not all PM&R programs are categorical.
Future studies should include a comparison study with pre and post surveys after implementing some of the above mentioned strategies to improve the quality of residency call. It would also be interesting to look at the average hours of sleep in programs that have in-house call versus home call.
CONCLUSION
ACKNOWLEDGMENTS
REFERENCES
- Schwartz AJ, Black ER, Goldstein MG, Jozefowicz RF, Emmings FG (1987) Levels and causes of stress among residents. J Med Educ 62: 744-753.
- Neufeld KS (2015) Poster 180 Examination of home call in an ACGME accredited PM&R residency program. PM&R 7: 151.
- Harvey R, Jarrett PG, Peltekian KM (1994) Patterns of paging medical interns during night calls at two teaching hospitals. CMAJ 151: 307-311.
- Goldsmith A, Melvin JL (2012) Developing a resident quality and safety curriculum. Health Policy Newsletter 25: 3.
- Yuasa M, Bell CL, Inaba M, Tamura BK, Ahsan S, Saunders V, et al. (2013) “You’re Being Paged!” outcomes of a nursing home on?call role?playing and longitudinal curriculum. J Am Geriatr Soc 61: 1976-1982.
Citation: Hwang J, Bajaj P (2018) Comfort Levels of Physical Medicine & Rehabilitation Residents during Call: A Survey Study. J Phys Med Rehabil Disabil 4: 024.
Copyright: © 2018 Jane Hwang , MD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

