
Comment on “Type 2 Sclerotic Modic Change Affect Fusion Result in Patients Undergoing Plif with Pedicle Screw Instrumentation: A Retrospective Study”
*Corresponding Author(s):
Xiangtao XieDepartment Of Spine Orthopedics, The Fourth Affiliated Hospital Of Guangxi Medical University, Liushi Road, Liuzhou, Guangxi, China
Email:drxxt@126.com ; 2417324775@qq.com
Introduction
We have read the recent paper by Hao Li et al [1], which appeared in BMC Musculoskeletal Disorder with great interest. The authors make a conclusion that type 2 sclerotic Modic change could be an important factor that affects solid bony fusion in patients undergoing Posterior Lumbar interbody Fusion (PLIF) with Pedicle Screw Instrumentation (PSI). Finally, the authors propose a simple algorithm for imaging patients with type 2 Modic change. If the patients’ MRI scan shows type 2 Modic change, CT should be performed as a routine examination before surgery. It might also provide a definitive imaging basis for the most advantageous location for spinal fusion. If the endplate sclerosis is mild or local, we would have a choice of interbody fusion or avoiding inter body fusion through the sclerotic area. If the endplate sclerosis is severe and widespread, their choice would be postero lateral fusion. Although we appreciate the authors' efforts to give us a novel point and a standardized guidelines for surgical treatment of type 2 Modic change patients. Objectively, besides the deficiencies raised in the discussion section, we think there are several defects in this study. We also outlined below a few comments.
The main point of this paper just focuses on the imaging level to explain the relationship between Type 2 Modic change with lumbar endplate sclerosis and lumbar fusion. It is known that chemical and mechanical stimulation of nociceptors adjacent to damaged endplates are likely a source of pain. Modic Changes may be not just a coincidental imaging finding in low back pain (LBP) patients and rather represent an underlying pathology that should be a target for treatment [2]. Growing evidence suggests that LBP patients with Modic changes have a clinically different presentation than LBP patients without Modic changes [3], LBP patients with Modic changes report a greater frequency and duration of LBP episodes [4]. Despite the limitations of a retrospective study, which only studied lumbar fusion with bony fusion, the postoperative imaging findings were not effective in assessing the difference between patients with Modic change and those without Modic change. At the very least, the study should have added a comparative analysis of clinical symptoms at the last postoperative follow-up. So the study lacks comprehensive evaluation of preoperative and postoperative clinical symptoms (such as visual analouge scale (VAS) score and oswestry disability index (ODI score) to explain whether the presence of type 2 Modic change or type 2 sclerosis Modic change before surgery aggravates the clinical symptoms of patients, and whether them affect the improvement of patients' postoperative clinical symptoms and affects the time of bony fusion. What's more, we are also very interested in the clinical efficacy of non-fused cases (Figures 1 & 2).
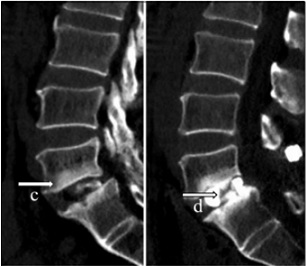 Figure 1: is taken from the reviewed paper. A patient with type 2 sclerotic Modic change and lumbar spondylolisthesis is at the 12-month follow-up evaluation.
Figure 1: is taken from the reviewed paper. A patient with type 2 sclerotic Modic change and lumbar spondylolisthesis is at the 12-month follow-up evaluation.
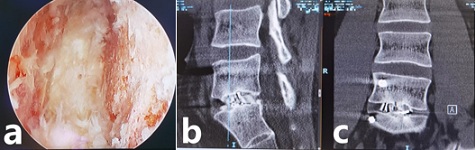 Figure 2: A patient with type 2 sclerotic Modic change lumbar and spinal stenosis is at the 8-month follow-up evaluation. The processed lumbar endplate at L5-S1 level (a) in the endoscopic transforaminal lumbar inter body fusion (Endo-TLIF). Sagittal reconstructed (b) Computed Tomography (CT) and coronal reconstructed (c) CT scan show that trabecular bone formation extend from the upper or lower endplate of L5-S1 (fully fusion). The plane shown in the straight line in Picture b shows the formation of numerous bone Bridges outside the cage in coronal reconstructed (c) CT.
Figure 2: A patient with type 2 sclerotic Modic change lumbar and spinal stenosis is at the 8-month follow-up evaluation. The processed lumbar endplate at L5-S1 level (a) in the endoscopic transforaminal lumbar inter body fusion (Endo-TLIF). Sagittal reconstructed (b) Computed Tomography (CT) and coronal reconstructed (c) CT scan show that trabecular bone formation extend from the upper or lower endplate of L5-S1 (fully fusion). The plane shown in the straight line in Picture b shows the formation of numerous bone Bridges outside the cage in coronal reconstructed (c) CT.
In the inclusion criteria of the study, subjects of lumbar spondylolisthesis and lumbar spinal stenosis were also included. It is better to further divide the studies into subgroups according to different diagnoses, because different etiology and biomechanical differences may affect the postoperative incidences of bony fusion. (Figure 1 just shows a patient with type 2 sclerotic Modic change lumbar spondylolisthesis.)
In terms of operative technique in the paper, as the co-first author of the reviewed paper, I have found that interlumbar bone graft in PLIF surgery was mainly concentrated on autogenous cortical bone in the cage device, and intervertebral bone grafted may be not enough. In most of the cases studied, a large number of external cage intervertebral bone bridging and trabecular bone formation extending from the upper or lower endplate were not observed. If a lot of intervertebral bone grafting or the addition of ostcoinductive growth factor materials (such as rh-BMP-2) were performed during the operation, or if endoscopic lumbar inter body fusion is used, the lumbar endplate can be processed more fully under visual endoscopy during the operation, and the scattered blood seepage on the surface of the osseous endplate can be clearly observed, so the incidences of bony fusion in group A (type 2 sclerosis Modic change) may be effectively improved (Figure 2). Therefore, in the discussion section, the authors propose a simple algorithm that we think needs a little extra content: if the endplate sclerosis is severe and widespread, our choice would be posterolateral fusion or endoscopic-assisted TLIF surgery.
References
- Li H, Chen S, Wei HY, Han CY, Zeng FY, et al. (2021) Type 2 sclerotic modic change affect fusion result in patients undergoing PLIF with pedicle screw instrumentation: A retrospective study. BMC Musculoskeletal Disorders 22: 598.
- Dudli S, Fields AJ, Samartzis D, Karppinen J, Lotz JC (2016) Pathobiology of modic changes. Eur Spine J 25: 3723-3734.
- Kjaer P, Korsholm L, Bendix T, Sorensen JS, Yde CL (2006) Modic changes and their associations with clinical findings. Eur Spine J 15: 1312-1319.
- Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, yde CL (2008) Vertebral endplate signal changes (Modic change): A systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J 17: 1407-1422.
Citation: Chen S, Peng XZ, Xie XT (2022) Comment on “Type 2 Sclerotic Modic Change Affect Fusion Result in Patients Undergoing Plif with Pedicle Screw Instrumentation: A Retrospective Study”. J Phys Med Rehabil Disabil 8: 73.
Copyright: © 2022 Shou Chen, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

