
Commentary: The Untaught Midline Retroperitoneal Approach to Repair Complex Abdominal Aortic Diseases
*Corresponding Author(s):
Tiziano TallaritaDepartment Of Cardiovascular Surgery, Mayo Clinic Health System, 1400 Bellinger St, Eau Claire, Wisconsin, United States
Email:tallarita.tiziano@mayo.edu
With increasing endovascular technology and skills, treatment of the aneurysmal and atherosclerotic occlusive aortic diseases is shifting towards a minimally invasive approach. Several prospective, randomized trials have shown decreased morbidity and mortality with the endovascular aneurysm repair (EVAR), compared to open surgery, for the treatment of infrarenal aortic aneurysms [1-4]. For aortic atherosclerotic occlusive disease, the preferred method of treatment is still controversial, with open surgical repair being considered the optimal approach in standard risk patients [5]. Endovascular treatment (kissing stents, covered endovascular reconstruction of the aortic bifurcation (CERAB), chimney-CERAB, and aorto-uni-iliac stent grafts) has been more commonly utilized in high-risk patients, but the mid and long-term patencies remain unknown [6-9]. As a result of the incessant transformation of the treatment of the aortic diseases, the vascular surgeons are becoming less comfortable performing open surgery, facing fewer but more complex open aortic repairs that require a supra renal or supra mesenteric clamp, such as for failed EVAR (“resilient”, high-pressure, endoleaks or graft infection) and for diseases involving the para visceral aorta. There are two techniques, well-illustrated in surgical books and atlas, which are taught during the surgical training to expose the abdominal aorta: The Midline Transperitoneal Approach (MTA) and the Lateral Retroperitoneal Approach (LRA). An “eternal fight” on the best modality exists between the two, with the MTA being the most familiar to the surgeons. Several retrospective studies highlighted the pros and cons of each approach, sometimes with opposite conclusions [10-12]. Historically, LRA has been utilized in patients with horseshoe kidney, inflammatory aneurysm, or history of multiple intraperitoneal procedures (hostile abdomen). Besides, LRA has been preferred for the exposure of the para visceral aorta. However, the LRA requires division of the lateral abdominal wall muscles with frequent muscular and/or flank bulging from muscle denervation and significant postoperative pain [13]. Furthermore, the LRA does not allow the exposure of the right iliac bifurcation and provides limited visualization of the right renal artery.
In the middle of the “battle” between MTA and LRA, there is a third approach that, timidly, has been mentioned in few studies [14-17], the Midline Retroperitoneal Approach (MRA). The MRA seems to integrate the pros of both MTA and LRA, circumventing the need to divide the lateral abdominal wall muscles (similar to the MTA and with, theoretically, less post-operative pain [14], yet maintaining a total, extraperitoneal route (like in LRA), very convenient for the surgeon in hostile abdomens, presence of horseshoe kidneys or inflammatory aneurysms. Previously described to treat only infrarenal aorta aneurysms [14-17], Buckarma et al. has recently published a further development of the technique, which enhances the ability to control of the right renal artery and right iliac artery bifurcation [18]. Briefly, the procedure starts with the patient in supine position. The retroperitoneal space can be accessed either by dividing the anterior rectus sheath in the inferior half of the abdomen, about 2 cm left lateral to the midline (Figure A) or by dissecting off the peritoneum sac from the abdominal wall, starting just below the xiphoid process (Figure B). Afterwards, the patient is moved to a lateral position by rotating the surgical bed, to facilitate the mobilization of the peritoneal sac (Figure C). The peritoneal sac and its content are retracted towards the right of the patient, exposing the aorta. In this technique, the left kidney is left in place. The right common iliac bifurcation can also be exposed at the beginning of the procedure by dividing the anterior rectus sheath, 2 cm right lateral to the midline. After the peritoneal sac is dissected off and retracted towards the left of the patient, the right common iliac artery bifurcation can be dissected free (Figure D). At the end of the procedure, after the aortic repair is completed, the anterior rectus sheath is closed with a running, monofilament, nonabsorbable suture (Figure E). Despite obvious advantages over the LRA, the MRA remains untaught (and unknown by many surgeons). In fact, the technique is not described in any surgical book or atlas, as now. We hope for the future that non usus non tollit usum! (“the unuse does not eliminate the possibility to use it!”) and to find the MRA technique described in all major vascular books and atlas.
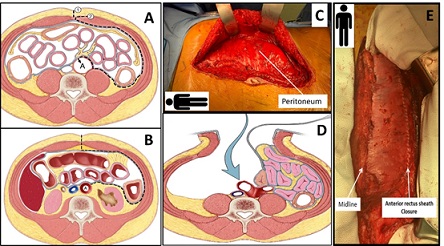 Figure 1: A) Illustration of the axial view of the lower abdomen showing how the retroperitoneal space is accessed by making a midline incision [1] and dividing the subcutaneous tissue until the fascia is identified. The left anterior rectus sheath is freed from the subcutaneous tissue for 2-3 cm left laterally and then divided [2]. The medial border of the left rectus muscle is mobilized laterally, accessing the pre-peritoneal space. The peritoneal sac is then mobilized from the lateral wall of the abdomen (dotted line) and retracted towards the right of the patient, exposing the aorta (A).
Figure 1: A) Illustration of the axial view of the lower abdomen showing how the retroperitoneal space is accessed by making a midline incision [1] and dividing the subcutaneous tissue until the fascia is identified. The left anterior rectus sheath is freed from the subcutaneous tissue for 2-3 cm left laterally and then divided [2]. The medial border of the left rectus muscle is mobilized laterally, accessing the pre-peritoneal space. The peritoneal sac is then mobilized from the lateral wall of the abdomen (dotted line) and retracted towards the right of the patient, exposing the aorta (A).
B) Illustration of the axial view of the upper abdomen showing an alternative way to expose the retroperitoneal space. The supra umbilical linea alba is incised (dotted line), identifying the pre-peritoneal fat pad. The peritoneum is dissected off the posterior aspect of the anterior wall with blunt and sharp dissection. Fibrous and fibro vascular strands of the posterior surface of the anterior abdominal wall are divided sharply with scissors to avoid peritoneal tears. The dissection continues posteriorly and laterally between the peritoneal sac and the Gerota’s fascia (dotted line). The peritoneal sac and its content are fully mobilized and retracted towards the right of the patient, exposing the aorta (A).
C) The patient is moved to a lateral position by rotating the surgical bed, to facilitate the mobilization of the peritoneal sac. In this picture, the peritoneal sac has been already fully dissected off the lateral abdominal wall and is ready to be retracted towards the right of the patient to expose the aorta.
D) Illustration of the axial view of the lower abdomen showing how to control the right common iliac artery bifurcation. The first step is similar to what seen in figure A but proceeds specularly opposite. Once the infra-umbilical midline incicion is made and the subcutaneous tissue divided with electrocautery, the right anterior rectus sheath is identified and dissected freed from the subcutaneous tissue for 2-3 cm right laterally. The right anterior rectus sheath is divided, and the medial border of the rectus muscle is mobilized laterally, accessing the pre-peritoneal space. The peritoneal sac and its content are freed and retracted towards the left of the patient, exposing the right common iliac bifurcation (blue arrow).
E) The anterior rectus sheath is closed with a running, monofilament, nonabsorbable suture. Importantly, the anterior rectus sheath was divided 2-3 cm from the midline to facilitate its closure at the end of the procedure.
References
- Chahwan S, Comerota AJ, Pigott JP, Scheuermann BW, Burrow J, et al. (2007) Elective treatment of abdominal aortic aneurysm with endovascular or open repair: the first decade. J Vasc Surg 45: 258-262.
- Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG; et al. (2004) Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomized controlled trial. Lancet 364: 843-848.
- Prinssen M, Verhoeven EL, Buth J, Cuypers PWM, van Sambeek MRHM, et al. (2004) A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med 351: 1607-1618.
- Lederle FA, Freischlag JA, Kyriakides TC, Matsumura JS, Padberg Jr FT, et al. (2012) Long-term comparison of endovascular and open repair of abdominal aortic aneurysm. N Engl J Med 367: 1988-1997.
- Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, et al. (2007) Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg 45: 65-67.
- Stewart S, Tallarita T, Wendt R, Beckermann J, Swartz H, et al. (2022) Chimney Graft Preservation of Inferior Mesenteric Artery during Endovascular Repair of Aortoiliac Occlusive Atherosclerotic Disease. J Vasc Interv Radiol 33: 861-863.
- de Cort BA, Salemans PB, Fritschy WM, Pierie MEN, Lind RC (2021) Long-Term Outcome for Covered Endovascular Reconstruction of Aortic Bifurcation for Aortoiliac Disease: A Single-Center Experience. J Endovasc Ther 28: 906-913.
- Maldonado TS, Westin GG, Jazaeri O, Mewissen M, Reijnen MMPJ, et al. (2016) Treatment of Aortoiliac Occlusive Disease with the Endologix AFX Unibody Endograft. Eur J Vasc Endovasc Surg 52: 64-74.
- Groot Jebbink E, Holewijn S, Versluis M, Grimme F, Hinnen JW, et al. (2019) Meta-analysis of Individual Patient Data After Kissing Stent Treatment for Aortoiliac Occlusive Disease. J Endovasc Ther 26: 31-40.
- Glover K, Lyden S, Bena JF, Smolock C, Parodi F (2020) Mid-Term Outcomes of Retroperitoneal and Transperitoneal Exposures in Open Aortic Aneurysm Repair. Ann Vasc Surg 66: 35-43.
- Buck DB, Ultee KH, Zettervall SL, Soden PA, Darling J, et al. (2016) Transperitoneal versus retroperitoneal approach for open abdominal aortic aneurysm repair in the targeted vascular National Surgical Quality Improvement Program. J Vasc Surg 64: 585-591.
- Ma B, Wang YN, Chen KY, Zhang Y, Pan H, et al. (2016) Transperitoneal versus retroperitoneal approach for elective open abdominal aortic aneurysm repair. Cochrane Database Syst Rev 6:CD010373.
- Sicard GA, Reilly JM (1994) Left retroperitoneal approach to the aorta and its branches: Part I. Ann Vasc Surg 8: 212-219.
- Nakajima T, Kawazoe K, Komoda K, Sasaki T, Ohsawa S, et al. (2000) Midline retroperitoneal versus midline transperitoneal approach for abdominal aortic aneurysm repair. J Vasc Surg 32: 219-223.
- Quick CRG, Chan CLH, Sonoda LI, Hart AJ (1997) Midline extraperitoneal approach for elective abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg 14: 63-68.
- Endo M, Kobayashi K, Tsubota M, Seki M, Sato H, et al. (1996) Advantages of using the midline incision right retroperitoneal approach for abdominal aortic aneurysm repair. Surg Today 26: 1-4.
- Shumacker HB Jr (1982) Extraperitoneal approach for vascular operations: retrospective review. South Med J 75: 1499-507.
- Buckarma E, Beckermann J, Gurrieri C, Frodl B, Saran N, et al. (2022) A midline retroperitoneal approach for complex abdominal aortic repair: Case description and operative technique. J Vasc Surg Cases Innov Tech 8: 678-687.
Citation: Dvir M, Tallarita T (2024) Commentary: The Untaught Midline Retroperitoneal Approach to Repair Complex Abdominal Aortic Diseases. J Angiol Vasc Surg 8: 115.
Copyright: © 2024 Tiziano Tallarita, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

