
Comparing Cone Beam Tomography Images with Periapical Radiographs to Diagnose Vertical Root Fractures
*Corresponding Author(s):
Hernandez EDepartment Of Endodontic, Universidad Santo Tomas, Colombia
Tel:+57 1 5878797,
Email:ely1712@yahoo.com
Abstract
The aim was to compare the diagnostic accuracy of periapical radiographs (PR) with cone beam tomography (CBCT) in the identification of vertical root fractures (VRF) in root treated teeth. Method: This review used the Cochrane Handbook along with the recommendations given by SIGN 50, both were taken as a guide. Meta DiSc 1.4 Software was used to calculate the operative characteristics of sensitivity, specificity, positive and negative values. Results: Initially 651 articles were obtained; after the complete review 4 articles were chosen: 2 studies had a sensitivity of 60-61% PR and 80% CBCT; specificity 70-71% RP and 69% CBCT; there was no significant differences between the two (p >0.05). Digital dental radiography (DDR) had a specificity of 78% compared to 70% of the RP. Conclusions: Due to the limited number of studies and the high degree of imprecision, it was difficult to determine more precise results. Both, the DDR and CBCT are useful by selecting the case. To reduce unnecessary radiation, DDR could be useful due to its image tools before a CBCT is taken into consideration.
Keywords
Cracked tooth syndrome; Cone beam computed tomography; Diagnostic; Root canal therapy; Tooth fracture
INTRODUCTION
A vertical root fracture (VRF) is defined as a complete or incomplete fracture that begins at the root at any level, usually in the bucolingual direction [1]. A prevalence of 2% - 5% of VRF in endodontically treated teeth has been reported, compared with VRF in endodontically treated teeth that were extracted and had a prevalence of 11-20% [2]. Methods to diagnose VRF include trans illumination and dye test, radiographic projection, bite test, periodontal probing, presence of fistulous tracts and exploratory surgery if necessary [3,4]. Yoshino et al. found that 31.7% (233 teeth) were extracted because of VRF and 93.6% had endodontics [5]. On the other hand, Fuss and Col reported a 10.9% prevalence of extractions due to vertical fractures in endodontically treated teeth [6]. In a systematic review, investigated the diagnostic ability of CBCT to detect VRFs in endodontically treated teeth and found: a prevalence of 40-90%, a sensitivity of 84-100% and a specificity of 64-100%. A diagnostic aid to identify VRF is to perform a diagnosis with Periapical Radiographs (PR), which have as limitation that they show a two-dimensional image that does not allow visualizing all the surfaces of the dental structure. There are other sensitive mechanisms such as the use of Cone beam computerized tomography (CBCT), which have better results compared to PR to identify VRFs.
However, this image modality is usually not available in dental private offices and is more expensive compared to conventional periodical radiography. The early stage of a VRF and the overlapping of anatomical structures adjacent to the involved tooth may complicate the detection for the diagnosis of fracture lines in PR, although they can only be observed when the fracture line and cone of the X-ray equipment they are in the same plane or almost 4° apart.
On the other hand, the verification of the diagnosis of a VRF can be done by a direct visualization with an exploratory surgery. After flipping off the flap, the fracture line is visualized with methylene blue and the use of magnification [7]. They conducted a systematic review where they found that there is a lack of evidence in databases regarding the accuracy in the diagnostic evaluation and clinical and radiographic effectiveness to identify VRFs in teeth treated endodontically [8] reported in their study a sensitivity of 74%, specificity of 62.2% and accuracy of 67.2% of CBCT for the detection of VRF [9]. Unfortunately, the most traditional methods have limited reliability because many signs and symptoms are not specific to VRF. Therefore, distinguishing a VRF from pulpal necrosis, failure of an endodontic treatment or periodontal disease is a challenge [10]. As previously mentioned, in order to visualize a VRF with a PR, a good angulation of the X-ray cone is required and consider the superposition of surrounding anatomical structures that make it even more difficult to visualize a VRF. It is for this reason that the plane of fracture is only observed in a third of the cases in PRs [11]. Once the diagnosis is established, the prognosis of a VRF is poor; because there are currently no reliable methods to treat VRF and usually the affected tooth is removed. The presence of this pathology in an endodontically treated tooth has a great impact on the prognosis of the treatment. Therefore, an early diagnosis of VRF is of great importance to avoid overtreatment and extensive bone loss. In this stage of clinical assessment, it must be taken into account that excessive and inadequate forces during endodontic treatment result in dentinal fatigue and cause VRFs or Cracks that will induce inflammation of the adjacent periodontium. Consequently, fractures can be found in the bucolingual direction, which extend from cervical to apical [12]. They can also start in the internal part of the root and extend towards the external surface or they can be partial. The most important sign is the pain at chewing. They can resemble abscesses of periodontal origin and present fistulas. However, many teeth with a root fracture show normal patterns of periodontal probing.
It is worth mentioning that in a PR a root fracture may not be seen because the intact segment can be superimposed over the fractured segment. In these cases, the diagnosis could be difficult clinically [13]. With the CBCT, the images are in three dimensions (3D) of high resolution that allow improving the diagnosis; however, there are few studies regarding the value of CBCT for diagnosing radicular fracture [14-16]. Undoubtedly, being able to determine the position, direction, and size of the fracture is of great value in choosing the treatment plan.
The aim of this review was to determine if CBCT or PR can identify and diagnose an early stage of VRF. For this reason, the purpose was to perform this search in four databases and to be able to make an analysis of the findings found.
METHODS
A systematic review of the literature was performed using the PubMed, Scopus, Cochrane and Web of Science databases between the years 2009-2018. The CONSORT statement guides were used [17].
Formulation of the research question
This means reducing the question to clear and precise terms, identifying its main components using the PICOS mnemonic. In the present Systematic Literature Review (SLR) the PICOS mnemonic applied to the clinical question is the following: P: Teeth with VRF, I: Cone Beam Computerized Tomography, C: Periapical Radiograph, OR: Early diagnosis of VRF, S: Experimental studies. Allowing determining the following research question: Which diagnostic tool allows the early identification of vertical root fractures between Cone Beam Computerized Tomography and Periapical Radiograph in endodontic practice?
The inclusion and exclusion criteria were defined to perform the article search (Table 1).
|
Inclusion Criteria |
Exclusion Criteria |
|
1. Experimental studies |
1. Animal studies |
|
2. Study population: human teeth |
2. Case series studies |
|
3. Publications: 10 last years |
3. Case report studies |
|
4. Language: english and spanish |
4. Dental alveolar trauma |
|
5. Teeth endodontically treated |
5. Intraradicular retainers |
|
6. VRFs caused by implants located |
6. Insufficient information |
|
on antagonists or proximal teeth |
|
Table 1: Inclusion and exclusion criteria
Search strategy:
Using the keywords, some formulas were established to perform the search in Pub Med, Cochrane, Scopus and Web of Science: Formula 1: 1 and 2 and 3 and 5. Formula 2: 1 and 2 and 4 and 5. Formula 3: 1 and 2 and 3. Formula 4: 1 and 2 and 4. Formula 5: 1 and 2 and 5. (Table 2) specifies the formulas with their keywords. The following filters were used: AND human, AND English, AND Spanish, AND 2009-2018.
|
Formula |
Combinations |
|
1 |
Diagnostic techniques AND procedures OR diagnosis, differential OR diagnosis, oral OR early diagnosis |
|
2 |
Tooth fracture OR Vertical root fracture OR Crack OR Root fracture OR Cracked tooth syndrome |
|
3 |
Cone-Beam Computerized Tomography OR CBCT OR Cone Beam Computed Tomography |
|
4 |
Dental Digital Radiography OR Dental Radiology OR Periapical Radiography |
|
5 |
Endodontics* |
Table 2: Formula combination to perform the search.
Information gathering and analysis
We searched through a list of results from the four electronic databases to identify relevant or potentially relevant studies. Two authors of the review independently reviewed and selected the relevant studies, extracted the non-relevant ones and gathered the information of the eligible final articles using a table (Table 3). The checklists for the precision quality assessment of the articles were made according to the recommendation of the Cochrane Handbook [18]; to analyze the accuracy and diagnosis of each article. This was done by the reviewers to control the biases; any disagreement in these steps was discussed and resolved by discussing and consulting with the authors of the review. The analysis of methodological quality and level of evidence was made by the two observers, who independently assessed the methodological quality and the level of evidence of the selected articles; established in accordance with the recommendations given by SIGN 50 (Scottish Intercollegiate Guidelines Network 2012) [19], where A represents the highest level of evidence and C the lowest. The Meta DiSc 1.4 Software was used to calculate the operational characteristics of sensitivity, specificity, positive and negative values to plot the data in the "receiver operating characteristics" (ROC) plane, which is a sensitivity graph as a function of 1- specificity; 95% confidence intervals were used, which are influenced by the size of the sample [20].
|
No |
Study |
QUEIROZ ET AL / 2016 (24) |
TOFONGCHIHA ET AL / 2011 (21) |
METSKA ET AL/ 2012 (22) |
HUANG ET AL, 2014 (23) |
|
1 |
Teeth characteristics |
|
|
|
|
|
1.1 |
Teeth endodontically treated |
20 uniradicular teeth |
230 uniradicular teeth |
39 endodontically treated teeth |
37 endodontically treated teeth with VRF |
|
1.2 |
Prevalence of VRF |
No investigated |
No investigated |
No investigated |
Not especified |
|
1.3 |
Especificity |
(0.85-0.98) |
70% (CR), 78% (DDR) |
56% ( Newton 3G) , 80% (3D Accuitomo 170) |
Not reported |
|
1.4 |
Sensibility |
(0.47-0.77) |
60% (CR), 61% (DDR) |
75% (Newton 3G),100% (3D Accuitmo170) |
Not reported |
|
1.5 |
Positive predictive value |
Not reported |
Not reported |
75% (Newton3G), 90% (3D Accuitomo 170) |
Not reported |
|
1.6 |
Negetive predictive value |
Not reported |
Not reported |
55% (Newton3G),100% (3D Accuitomo170) |
Not reported |
|
1.7 |
Test accuracy |
Not reported |
* CR - 65% |
68% Newton 3G), 93% (3D Accuitomo170) |
Not reported |
|
|
|
|
* DDR - 70% |
|
|
|
1.8 |
Bias control |
Not reported |
Not reported |
Three blinded endodontist assessed all the images independently twice. |
Not reported |
|
2 |
Study characteristics |
|
|
|
|
|
2.1 |
Study design |
Experimental in-vitro |
Experimental in-vitro |
Experimental in-vitro |
Experimental in-vitro |
|
2.2 |
Study setting |
Academic institution |
Not especified |
Academic institution |
Not especified |
|
2.3 |
Inclusion criteria |
Not especified |
Single rooted human teeth with closed apices. |
*Patients from 2009-2011 with clinical and radiographic signs suggesting the presence of VRF in endodontically treated teeth. |
*Teeth extracted after clinical diagnosis of VRF. |
|
|
|
|
|
*Pain on percussion and/or palpation, presence of deep isolated periodontal pocket (bone loss), presence of multiple sinus tracts, and halo or J-type radiolucency around the corresponding tooth on the periapical radiograph (PR). |
*Only extracted teeth without evident root surface damage. |
|
|
|
|
|
|
*All teeth must have had at least 1VRF line on the root surface confirmed by 2 endodontists. |
|
2.4 |
Exclusion criteria |
Not especified |
Internal or external fracture and roots with severe curvatures |
Not especified |
Not especified |
|
2.5 |
Level of evidence |
2- |
2+ |
2+ |
2- |
|
2.6 |
Grade of recomendation |
C |
B |
B |
C |
|
2.7 |
Ranking |
Q1 |
Q1 |
Q2 |
Q1 |
|
3 |
* Index test |
|
|
|
|
|
3.1 |
CBCT model (voxel size) |
N/A |
N/A |
* Newtom 3G. 110 kv, 3.90 - 5.6 mA (QR SLR, Verona, Italy). |
μ - CT (Trimph X-0 Ct System; Gamma medical Ideas, Northridge, California) |
|
|
(tamaño del Voxel) |
|
|
* 3D Accuitomo 170. 90 kv, 5 mA (J. Morita, Kyoto, Japan). |
|
|
3.2 |
Periapical machine model |
* GX-770 periapical machine (Gendex Dental Systems, Lake Zurich, IL; 70 Kvp, 7 mA, exposure time 0.08") |
Plameca Dental X-ray unit |
N/A |
N/A |
|
|
|
*DBSWIN software (DüRR Dental, Bietigheim-Bissingen, Germany) |
(Plameca, Finland) |
|
|
|
3.3 |
Imaging parameters |
|
|
|
|
|
|
CBCT |
N/A |
N/A |
Voxel size for Newtom 3G - 2mm |
80 kv, 90 μA, field of view 29.59 mm |
|
|
|
|
|
Voxel size for 3D accuitomo - 0.08 mm |
Acquisition time 5 minutes y 512 slices. |
|
|
Periapical Radiograph |
* Radiographs were taken in an orthoradial incidence (0° horizontal and vertical angles indicated by a protractor) with the aid of a custom holder designed to maintain the specimen, the film holding device, and the image receptor in a reproducible relationship. |
* 63 kVp, 8 mA |
N/A |
N/A |
|
|
type/parameters |
|
*Exposure time: |
|
|
|
|
|
|
Conventional Radiograph (CR) - 0.16" |
|
|
|
|
|
|
Direct Digital Radiograph (DDR) - 0.1" |
|
|
|
|
|
|
* Kodak E speed No 2 periapical film (Eastman-Kodak Co, Rochester, NY, USA) |
|
|
|
|
|
|
Processed manually for 15" at 22°C with Teifsaz chemicals |
|
|
|
|
|
|
(Teifsaz, Tehran, Iran) |
|
|
|
4 |
Interpreters |
|
|
|
|
|
4.1 |
Interpreters |
3 calibrated examiners |
2 observers (who had more than 10 years’ experience in dental radiography). |
3 observers assessed all images twice and independently. |
2 endodontists confirmed the presence of VRF on the root surface. |
|
4.2 |
Blinding |
Not especified |
The observers were not aware of the fractured teeth distribution. |
The observers did not receive clinical information before examination. |
Not defined |
|
4.3 |
Agreement |
Intra-observer and inter-observer reproducibility was evaluated by using Kappa test. The scores were compared with the gold standard by use the operating characteristics curve (ROC). Significance level of 5% |
* Coher's kappa statistics. |
Intra-observer agreement (Cohen Kappa) was calculated for each observer and for each scanner independently. Used the interclass correlation coefficients (ICCs). |
Fisher exact test was used to evaluate fracture width >100 μm y ≤100 μm, fracture line extension within the apical 3mm were associated with the number of fracture lines. |
|
|
|
|
* X² test to compare two observers ‘diagnosis. |
|
|
|
5 |
Reference test |
N/A |
N/A |
Orthograde retreatment endodontic surgery, or tooth extraction. |
N/A |
|
|
(eg. surgical exploration, extraction, retreatment) |
|
|
|
|
|
6 |
Conclusions |
Digital subtraction radiography could be considered as an alternative tool or the investigation of VRFs because of its comparable diagnostic accuracy to existing methods. |
No significant difference was seen between the two techniques. The specificity of DDR was slightly better than CR, and their accuracy and sensibility showed small differences. |
The results of our study support the use of 3D Accuitomo 170 for the detection of VRFs in endodontically treated teeth. They also suggest that the reproducibility and accuracy in VRF detection depend on the CBCT system used. |
Application of 9-μm CT can be accurately used for early detection of VRF. Fracture characteristics (eg. number of fracture lines, extension of fracture line) may affect the fracture width. Appropriate use of μ-CT technology can be helpful for early diagnosis of VRF. |
Table 3: Summary of characteristics of the included studies
RESULTS
Results of the search
A total of 651 articles were identified in the search made in the databases (Pub Med, Scopus, Cochrane and Web of Science), unrelated and duplicate articles were eliminated (n=409); obtaining a total of (n= 242) items in the electronic search. The review of abstracts was made and those that did not meet the inclusion criteria were eliminated (n=212); there were 26 eligible articles; they were read in full text. The remaining 4 articles were analyzed (Graph 1). A critical reading was made of the validity and applicability of the results of the research published in the selected articles, according to the CONSORT guidelines, leaving a total of 4 articles; which were analyzed in the review [21-24].
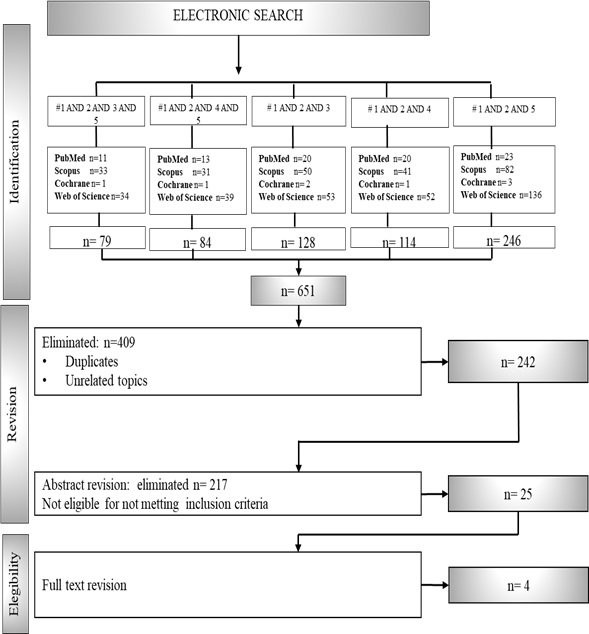 Graph 1: Study flow diagram showing the process of selection of studies for the systematic review.
Graph 1: Study flow diagram showing the process of selection of studies for the systematic review.
FINDINGS
The samples sizes of the 4 studies were from 20 to 230 teeth treated endodontically. For the "index test" the models of the equipment that were reported in 4 studies [25,26] were taken into account, where there was a variety of equipment and parameters; in addition, the interpreters in the studies were experienced oral radiologists or endodontists. In the agreement between observers; only one study reported an "agreement score" of 25%. As for the "reference test", which consists of surgical exploration, extraction or retreatment, this was only reported in 1 study. Sensitivity values reported in 2 studies vary between 60-61% in PRs and 80% in CBCT, specificity values vary between 70-71% in RP and 69% in CBCT, and better sensitivity was observed in the Metska study (81%), there was no significant difference between the two (p> 0.05), (Graph 2). In the specificity it was observed that DDR is more specific for the diagnosis of VRFs compared to conventional PR due to its variety of image tools that let to observe the teeth with different color shades.
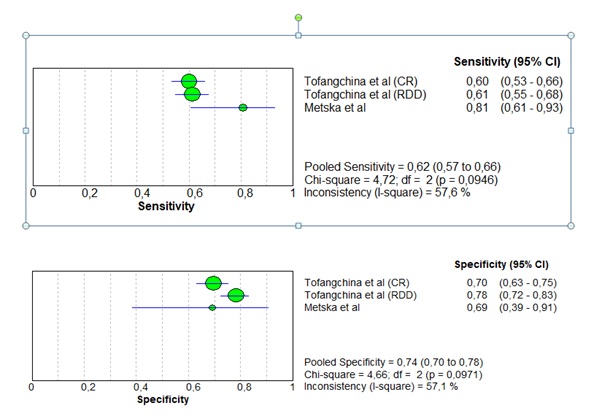 Graph 2: Regarding sensitivity, no statistically significant differences were found between tests (p> 0.05). However, it can be observed descriptively that the test in all reports greater sensitivity. Regarding the specificity, no statistically significant differences were found between tests (p> 0.05), however it can be observed descriptively that the test in (RDD/DDR) reports greater specificity.
Graph 2: Regarding sensitivity, no statistically significant differences were found between tests (p> 0.05). However, it can be observed descriptively that the test in all reports greater sensitivity. Regarding the specificity, no statistically significant differences were found between tests (p> 0.05), however it can be observed descriptively that the test in (RDD/DDR) reports greater specificity.
Values were plotted in a plane that showed the "ROC Curve" where it was observed that the two studies are located above the diagonal, indicating an acceptable sensitivity and specificity (Graph 3). One of the final articles found in the review, using PR / DAR (Digital Abduction Radiography) reported a Specificity of 85-98% and Sensitivity of 47-77% another article found in this review, did not report specificity or sensitivity in their study using CBCT.
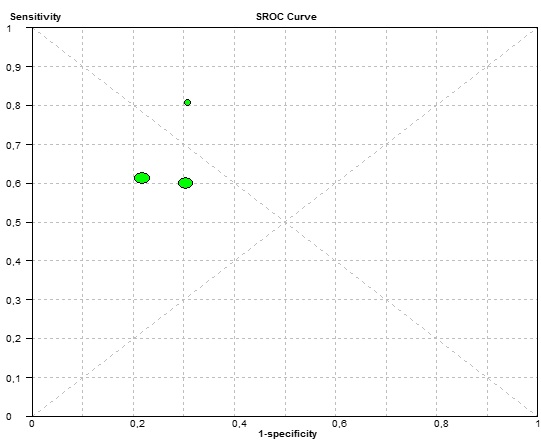 Graph 3: In the ROC plot of studies used, the 3 studies are above the main diagonal, which indicates that the sensitivity and specificity as a whole are appropriate.
Graph 3: In the ROC plot of studies used, the 3 studies are above the main diagonal, which indicates that the sensitivity and specificity as a whole are appropriate.
DISCUSSION
This systematic review sought to determine, according to the literature, which of the two diagnostic tools (CBCT and PR) has helped to identify VRFs in early stages. According to the Cochrane handbook, there are reviews that could end up with a small number of articles that can be lead to make an analysis of it. Four studies were considered eligible for inclusion; although all showed a high risk of bias due to the fact that imprecision in the reported ranges of diagnostic ability was identified in three studies because they had a small sample size used in them, all used different models of radiographic equipment and CBCT, and parameters of different images and different techniques used in each diagnostic tool. The results of this review should be analyzed with caution because the radiological interpretation is not the same in each situation; which may affect the final sensitivity and specificity values [27].
For example, a more conservative observer might interpret root fractures as such, only if a bony area that would produce a high specificity value and a low sensitivity value is clearly seen in the image; compared to a less conservative observer, who can report the presence of a fracture despite artifacts near the area [28]. The difference in training and experience (eg. oral radiologists vs. endodontists) can be a significant variable of the diagnostic source. Therefore, these findings cannot reflect the interpretation capacity of the observers. Due to the limited number of studies included in the current review, it is not possible to make an objective analysis to determine more accurately the impact of the use of diagnostic tools (CBCT and PR).
However, the interpretations presented in the included studies were based on interpretations of endodontists and oral radiologists trained in these diagnostic tools. The reproducibility of the 4 studies is limited because there was no information in two studies on the scores of "agreement between observers" ; it was presented as a limitation. It should also be mentioned that only 2 studies reported the positive and negative predictive values; which was considered another limitation to be able to make a descriptive statistical analysis of positive and negative predictive values. However, there was information in two articles (to be able to graph this information in a plane the values of ROC, where the sensitivity is compared and specificity. After an in-vivo diagnostic study of VRF, reported a sensitivity of conventional radiograph (CR) of 23% [29], found that although many fractures are not accessible to the clinical examination, it is worth mentioning that the PRs and the dental digital radiographs (DDR) serve very well as diagnostic tools. The intraoral film can provide a resolution of more than (20 lp mm) 1. While current digital systems are capable of providing a resolution of (7 lp mm) 1. Despite this fact, the level of agreement in his study with digital system and with radiographic film were the same in this study. These studies support the results of who reported a specificity between 85-98% and a sensitivity between 47-77%, considering the use of the subtraction radiograph (SR) as an alternative tool to diagnose VRF due to the diagnostic accuracy comparable with existing methods.
The visualization is difficult due to the superposition of the fracture line by the sealing material. Even with methods such as CBCT, the presence of guttapercha decreases the diagnostic accuracy [30]. The CBCT allows to acquire 3D (3-dimension) volumes of the dental arches with high spatial resolution and low radiation compared with the Computed Tomography (CT) [31]. Some studies support the use of CBCT to detect VRF in endodontically treated teeth [32,33]. However, in these studies fractures were created artificially, which may differ from those that occur "naturally." Also, when the identification of VRFs with CBCT was compared, there were always differences between the precision between ex vivo and in vivo [34,35]. It has been studied that CBCT has a greater sensitivity and specificity than periodical radiographs (PRs) to detect fracture lines in teeth. In contrast to these studies, reported that, due to the imprecision of reported ranges and biases observed in their systematic review, they determined that there is insufficient evidence to suggest that CBCT is reliable for detecting VRF in teeth endodontically treated. The resolution of the CBCT depends on the size of the voxel, the focal point, kV and different CBCT settings [36]. The smaller the voxel size, the higher the CBCT resolution. Therefore, a higher resolution may be required to detect a longitudinal fracture. According to the findings of a recent systematic review, [37] evaluated the ability to diagnose both teeth with and without endodontic treatment, separately analyzing in vivo and ex vivo studies; they concluded that there is a very limited number of studies and that there is no evidence to suggest that CBCT can provide an additional benefit in the diagnosis to detect VRF in teeth with endodontic treatment. Also [38], examined the efficacy of CBCT in endodontics; they concluded that there is currently insufficient evidence to support efficacy in the diagnosis using CBCT, which means that its potential impact to improve patient outcomes and reduce the cost-benefit ratio is questionable. There is a concern about an increase in the indiscriminate and unjustified use of CBCT, the principles of "ALARA" (as low as reasonable achievable) should be taken into account when deciding to order CBCT images, because it is now known that any exposure to ionizing radiation it can have potentially harmful effects [39]. According to the American Academy of Oral and Maxillofacial Radiology and the American Association of Endodontists, the decision to order CBCT should only be considered "if in the intraoral and radiographic 2D clinical examination they are inconclusive to detect vertical root fracture" [40]. While in the European guidelines described in the SEDENTEXCT project, clinicians should keep in mind that even if a CBCT image is taken, root fillings limit diagnostic accuracy [41]. As limitations we found that there were only 4 studies with limited data availability could be included, despite the fact that additional information was requested from the authors, which could have helped to conduct a complete statistical analysis, making it difficult to draw definitive conclusions.
CONCLUSION
It was observed in the studies analyzed that DDR and CBCT are both useful to diagnose VRFs. However, using DDR with operator's knowledge and expertise by making good use of image tools could lead to a more accurate interpretation and, reducing the unnecessary radiation to the patient. The research question could not be answered because more studies are required. To make an early diagnosis, current imaging tools, clinical methods and patient's symptoms must be considered.
REFERENCES
- Adorno CG, Yoshioka T, Jindan P, Kobayashi C, Suda H, et al. (2013) The effect of endodontic procedures on apical crack initiation and propagation ex vivo. Int Endod J 46: 763-768.
- Chang E, Lam E, Shah P, Azarpazhooh A (2016) Cone-beam Computed Tomography for Detecting Vertical Root Fractures in Endodontically Treated Teeth: A Systematic Review. J Endod 42: 177-185.
- Tamse A (2006) Vertical root fractures in endodontically treated teeth: diagnostic signs and clinical management. Endod Top 13: 84-94.
- Meister F, Lommel TJ, Gerstein H (1980) Diagnosis and possible causes of vertical root fractures. Oral Surgery, Oral Med Oral Pathol. 49: 243-253.
- Yoshino K, Ito K, Kuroda M, Sugihara N (2015) Prevalence of vertical root fracture as the reason for tooth extraction in dental clinics. Clin Oral Investig 19: 1405-1409.
- Fuss Z, Lustig J, Tamse A (1999) Prevalance of vertical root fractures in extracted endnotically treated teeth Pg no: 283–286.
- Bayram H, Bayram E, Eren H (2015) A diagnostic dilemma: Vertical fracture case. Univers Res J Dent Pg no: 5:31.
- Tsesis I, Rosen E, Tamse A, Taschieri S, Kfir A, et al. (2010) Diagnosis of vertical root fractures in endodontically treated teeth based on clinical and radiographic indices: A systematic review. J Endod 36:1455-1458.
- Eskandarloo A, Asl AM, Jalalzadeh M, Tayari M, Hosseinipanah M, et al. (2016) Effect of time lapse on the diagnostic accuracy of cone beam computed tomography for detection of vertical root fractures. Braz Dent J 27:16–21.
- Yiit Ozer S, Unlu G, Deer Y (2011) Diagnosis and treatment of endodontically treated teeth with vertical root fracture: Three case reports with two-year follow-up. J Endod 37: 97-102.
- Bernardes RA, De Moraes IG, Hungaro Duarte MA, Azevedo BC, De Azevedo JR, et al. (2009) Use of cone-beam volumetric tomography in the diagnosis of root fractures. Oral and Maxillofacial Radiology 108: 270-277.
- Walton RE (2017) Vertical root fracture: Factors related to identification. J Am Dent Assoc 148: 100-105.
- Testori T, Badino M, Castagnola M (1993) Vertical root fractures in endodontically treated teeth: A clinical survey of 36 cases. J Endod 19: 87-90.
- Tsesis I, Kamburoglu K, Katz A, Tamse A, Kaffe I, et al. (2008) Comparison of digital with conventional radiography in detection of vertical root fractures in endodontically treated maxillary premolars: an ex vivo study. Oral Surgery, Oral Med Oral Pathol Oral Radiol Endod 106: 948-952.
- Hannig C, Dullin C, Hulsmann M, Heidrich G (2005) Three-dimensional, non-destructive visualization of vertical root fractures using flat panel volume detector computer tomography: An ex vivo in vitro case report. Int Endod J 38: 904-913.
- Brady E, Mannocci F, Brown J, Wilson R, Patel S, et al. (2014) A comparison of cone beam computed tomography and periapical radiography for the detection of vertical root fractures in nonendodontically treated teeth. Int Endod J 47: 735-746.
- Cobos Carbo A, Augustovski F (2011) CONSORT Statement 2010: Update of the checklist to report randomized parallel group clinical trials. Med Clin (Barc) 137: 213-215.
- Higgins JPT, Green S (2011) Cochrane Handbook of Systematic Reviews of Interventions. Cochrane Pg no: 1-639.
- Duellman W (1982) Quaternary climatic-ecological fluctuations in the lowland tropics: frogs and forests. Biol Diversif Trop Pg no: 389-402.
- Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A, et al. (2006) Meta-DiSc: A software for meta-analysis of test accuracy data. BMC Med Res Methodol 6: 1-12.
- Tofangchiha M, Bakhshi M, Fakhar HB, Panjnoush M (2011) Conventional and digital radiography in vertical root fracture diagnosis: A comparison study. Dent Traumatol. 27: 143-146.
- Metska ME, Aartman IHA, Wesselink PR, Ozok AR (2012) Detection of vertical root fractures in vivo in endodontically treated teeth by cone-beam computed tomography scans. J Endod 38: 1344-1347.
- Huang CC, Chang YC, Chuang MC, Lin HJ, Tsai YL, et al. (2014) Analysis of the width of vertical root fracture in endodontically treated teeth by 2 micro-computed tomography systems. J Endod 40: 698-702.
- Queiroz PM, Nascimento HAR, Da Paz TDJ, Anacleto FN, Queiroz FD (2016) J Endod 42: 896-899.
- Neves FS, Freitas DQ, Campos PSF, Ekestubbe A, Lofthag Hansen S, et al. (2014) Evaluation of cone-beam computed tomography in the diagnosis of vertical root fractures: The influence of imaging modes and root canal materials. J Endod 40: 1530-1536.
- Silva Fuente Alba C, Molina Villagra M (2017) Likelihood ratio (likelihood ratio): definition and application in Radiology. Rev Argentina Radiol 81: 204-208.
- Macaskill P, Gatsonis C, Deeks J, Harbord R, Takwoingi Y, et al. (2010) Chapter 11: Interpreting results and drawing conclusions. In: Deeks JJ, Bossuyt PM, Gatsonis C (editors), Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 0.9. Pg no: 1-61.
- Menezes D, Araujo NC, Santa Rosa JMC, Carneiro VSM, Santos Neto AP dos, et al. (2016) Detection of vertical root fractures in endodontically treated teeth in the absence and in the presence of metal post by cone-beam computed tomography. BMC Oral Health 16:16-21.
- Youssefzadeh S, Gahleitner A, Dorffner R, Bernhart T, Kainberger FM, et al. (1999) Dental Vertical Root Fractures: Value of CT in Detection. Radiology 210: 545-549.
- Patel S, Brady E, Wilson R, Brown J, Mannocci F, et al. (2013) The detection of vertical root fractures in root filled teeth with periapical radiographs and CBCT scans. Int Endod J 46: 1140-1152.
- Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, et al. (2012) Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol. 81: 267-271.
- Hassan B, Metska ME, Ozok AR (2009) Detection of Vertical Root Fractures in Endodontically Treated Teeth by a Cone Beam Computed Tomography Scan. J Endod 35: 719-22.
- Yiit Ozer S (2011) Detection of vertical root fractures by using cone beam computed tomography with variable voxel sizes in an in vitro model. J Endod 37: 75-79.
- Hassan B, Metska ME, Ozok AR, Van der Stelt P, Wesselink PR, et al. (2010) Comparison of Five Cone Beam Computed Tomography Systems for the Detection of Vertical Root Fractures. J Endod 36: 126-129.
- Edlund M, Nair MK, Nair UP (2011) Detection of vertical root fractures by using cone-beam computed tomography: A clinical study. J Endod 37: 768-772.
- Scarfe WC, Farman AG (2008) What is Cone-Beam CT and How Does it Work? Dent Clin North Am 52: 707-730.
- Corbella S, Del Fabbro M, Tamse A, Rosen E, Tsesis I, et al. (2014) Cone beam computed tomography for the diagnosis of vertical root fractures: A systematic review of the literature and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 118: 593-602.
- Rosen E, Taschieri S, Del Fabbro M, Beitlitum I, Tsesis I, et al. (2015) The Diagnostic Efficacy of Cone-beam Computed Tomography in Endodontics: A Systematic Review and Analysis by a Hierarchical Model of Efficacy. J Endod 41: 1008-1014.
- Preston RJ (2008) Update on linear non-threshold dose-response model and implications for diagnostic radiology procedures. Health Phys 95: 541-546.
- Beam C, Tomography C (2015) AAE and AAOMR Joint Position Statement. J Endod 41: 1393-1396.
- Honer K, Rushton VE (2012) Radiation Protection Protection: Cone Beam CT for Dental and Maxillofacial Radiology (Evidence-based Guidelines). Radiat Prot Eur Comm Pg no: 156.
Citation: Hernandez E, Mendez C and Jimenez PM (2020) Comparing Cone Beam Tomography Images with Periapical Radiographs to Diagnose Vertical Root Fractures. J Transl Sci Res 3: 012.
Copyright: © 2020 Hernandez E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

