Root canal preparation and filling should not extend beyond the tooth root nor leave uninstrumented areas inside the root canal. Accurate determination of working length during root canal treatment is a challenge. Anatomically, the Apical Constriction (AC), also called the minor apical diameter or minor diameter, is a logical location for working length since it often coincides with the narrowest diameter of the root canal [1,2]. However, locating the AC clinically is problematic. Dummer et al., concluded that it is impossible to locate the minor foramen clinically with certainty because of its position and topography [3]. The Cementodentinal Junction (CDJ) has also been suggested as the location for WL because it represents the transition between pulpal and periodontal tissue (Grove 1931). The location of the CDJ is widely accepted as being 0.50 mm to 0.75 mm coronal to the apical foramen but, as with the AC, the exact location of the CDJ is impossible to identify clinically [4]. In general, the CDJ is considered to be co-located with the minor foramen; however, this is not always the case [2,5].
Working length is defined as “the distance from a coronal reference point to the point at which canal preparation and filling should terminate” [3]. Radiographic determination of working length has limitations such as distortion, shortening and elongation, interpretation variability, and lack of three-dimensional representation. Even when a paralleling technique is used, elongation of images has been found to be approximately 5% [6].
A working length 1 mm short of the radiographic apex may result in over or under instrumentation because of the variability in distance between the terminus of the root canal (minor foramen) and the radiographic apex [7]. Thus, this often-used “rule” is not predictable or reliable.
Custer was the first to determine working length electronically [8]. Suzuki investigated the electrical resistance properties of oral tissues and developed the first electronic apex locator [9]. The device was resistance-based and measured the resistance between two electrodes to determine the location of an instrument in the canal. Later devices were impedance-based and used multiple frequencies [10]. More recently, resistance and capacitance-based devices emerged that measure resistance and capacitance, directly and independently.
The Root ZX (Tokyo, Japan) uses the “ratio method” to locate the minor foramen by the simultaneous measurement of impedance using two frequencies [11,12]. The Root ZX claims to work in the presence of electrolytes and non-electrolytes and requires no calibration [13].
CanalPro (Coltene Whaledent, Inc.), a modern apex locator uses multiple frequencies (unlike conventional apex locators, two measuring frequencies are alternated, not mixed, eliminating noise and the need for signal filtering. Signal intensity is used to calculate the file tip position, making the measurement immune to electromagnetic interference) in an attempt to eliminate the influence of canal conditions.
In addition to improving working length accuracy EAL address concerns about radiation as they have the potential to reduce the number of radiographs taken during root canal treatment [10,14].
The purpose of this study was to evaluate in vivo of the accuracy and predictability of two EALs for determining working length as compared to radiographs: RootZX and CanalPro. The null hypothesis is that these apex locators provide identical results related to working length determination in vivo.
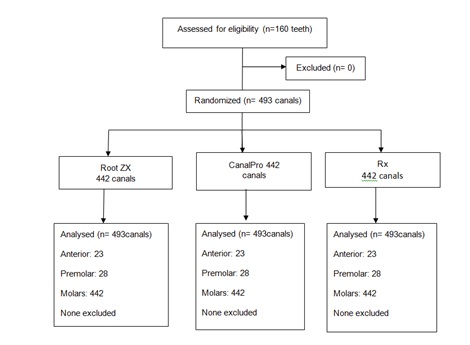
Root ZX and CanalPro Apex Locators (ALs) with equal working frequencies (0.4 kHz and 8 kHz) were used. One hundred and eighty patients, ages 28-75 years, contributed in the study. One hundred and sixty teeth (493 canals) with fully formed apices (confirmed by radiographic evaluation before treatment) and apical periodontitis were used (Table 1 and Figure 1). Pulps in 31 teeth were nonvital; rests of the teeth gave positive responses to hot and cold tests and were scheduled for extraction for periodontal or prosthodontic reasons. Approval by the institutional review and ethical board before commencement of the study was obtained and written consent was obtained from each patient.
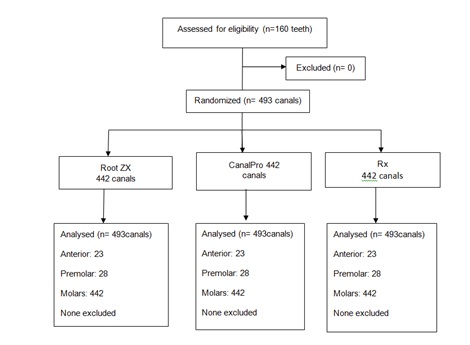 Figure 1:
Figure 1: Consort flowchart for this study.
|
No. of canals
|
|
Tooth
|
n
|
Maxillary
|
Mandibular
|
|
Central Incisor
|
10
|
7
|
3
|
|
Lateral Incisor
|
8
|
6
|
2
|
|
Canine
|
5
|
3
|
2
|
|
Premolar
|
17
|
22
|
6
|
|
Molar
|
120
|
225
|
217
|
|
Total
|
160
|
263
|
230
|
Table 1: Distribution of 160 teeth (493 canals).
After local anesthesia, rubber dam isolation and access cavity preparation was prepared in such a way that straight-line access to the root canals was provided and undercuts were avoided. After the identification of the root canals, the canals were flared coronally with size 1 and 2 Orifice Shapers (Dentsply Tulsa Dental, Tulsa, OK, USA) using 2.5% sodium hypochlorite for irrigation. The final rinse was aspirated but no attempt was made to dry the canals.
The Apical Constriction (AC) of each tooth was located with two electronic apex locators. A single operator then determined the working lengths. The Root ZX and the CanalPro were used according to the manufacturer’s instructions. The lip clip was attached to the patient’s lip and a size 15 file was coupled to the electrode of the apex locators.
The minor foramen was located with the Root ZX by advancing a size 15 stainless steel K- file in the canal until the locator indicated that the minor foramen had been reached, according to the manufacturer’s instructions (Root ZX operation guide).The LCD showed a flashing bar between APEX and 1 and a flashing tooth. The silicone stop on the file was positioned at the reference point. The instrument fixed within a removable light curing composite pattern (Ceram X; Dentsply, Konstanz, Germany).
This was the insertion length. Then the composite pattern removed from the tooth. The procedure was repeated in the same tooth with another instrument using the CanalPro. In each case, the composite pattern was repositioned exactly in the respective tooth. The AC was located with the CanalPro by advancing the same size 15 K file in the canal until the locator indicated that the minor foramen had been reached as per the manufacturer’s instructions. The stop positioned at the reference point and the insertion length measured. The sequence of testing alternated between the two locators.
According to the CanalPro (CanalProTM Apex Locator, users guide) apical zone is divided into 11 segments graduated from 1.0 to 0 (Apex) as visual information of file progression. When the apex is reached (read bar at the mark “0” and reading “APEX”), solid tone is emitted. To determine the working length for shaping, it is recommended to subtract 0.5 mm from the apical length.
The minor foramen was located radiographically by advancing the size 15 K file until its tip was 1.0 mm from the radiographic apex (determined from a pretreatment parallel technique radiograph). A radiograph was exposed and if the file tip was seen not to be 1.0 mm from the radiographic apex the file was repositioned and another radiograph taken to ensure that it was. The distance from the stop to the tip was the insertion length. The file was then re-inserted to the insertion length (1 mm from the radiographic apex) and cemented in place with Fuji II LC dual-cure glass ionomer cement (GC Corp, Tokyo, Japan). The file handle was sectioned with a high-speed bur and the tooth was extracted without disturbing the file, placed in 6% NaOCl for 15 min to remove remaining tissue from the root surface and stored in a 0.2% Thymol solution. The principal investigator conducted all of the clinical procedures.
After the tooth was removed from the solution and with the file still in place, the apical 5 mm of the root was ground parallel to the long axis of the canal with a fine diamond bur and abrasive discs. When the file became visible, additional dentine was removed under 20X magnification (OPMI Pico microscope, Carl Zeiss, Munich, Germany) until the file tip, the canal terminus, and the foramen were in focus. The first digital image taken and stored in Adobe Photoshop 5.5 (Adobe Systems Inc., San Jose, CA, USA) and the distance of the file tip to the minor foramen measured. This distance was recorded as being: -1.0 mm from the minor foramen; -0.5 mm from the minor foramen; at the minor foramen; +0.5 mm from the minor foramen or +1.0 mm from the minor foramen. A minus symbol (-) indicated a file short of the minor foramen; A plus symbol (+) indicated it was long.
The second image made with the repositioned composite pattern for the measurement with the Root ZX and the third image made with the composite pattern for the working length determination with CanalPro.
Once the actual length to the minor foramen was measured visually, the distance from the minor foramen determined by the two EAL was also completed (-1.0 mm from the minor foramen; -0.5 mm from the minor foramen, etc.,), by comparing their insertion lengths to the actual length (distance to the AC) (Tables 2, 3 and 4).
|
Distance from minor foramen (mm)
|
Root ZX
|
CanalPro
|
Radiograph
|
|
n = 23(%)
|
n = 23(%)
|
n = 23(%)
|
|
-1.0
|
-
|
-
|
-
|
|
-0.5
|
-
|
-
|
-
|
|
MF
|
19 (82.60)
|
16 (69.56)
|
5 (21.7)
|
|
+0.5
|
4 (17.39)
|
7 (30.43)
|
12 (52.17)
|
|
+1.0
|
|
6 (26.08)
|
|
Table 2: Distance of file tip from minor foramen determined by Root ZX, CanalPro and Radiograph (anterior teeth).
MF: Minor Foramen
(+) and (-) values indicate file tip beyond (+) or short (-) of the AC.
|
Distance from minor foramen (mm)
|
Root ZX
|
CanalPro
|
Radiograph
|
|
n = 28(%)
|
n = 28(%)
|
n = 28(%)
|
|
-1.0
|
-
|
-
|
-
|
|
-0.5
|
-
|
-
|
-
|
|
MF
|
21 (75)
|
18 (64.28)
|
8 (28.57)
|
|
+0.5
|
7 (25.0)
|
10 (35.71)
|
15 (53.57)
|
|
+1.0
|
|
|
5 (17.85)
|
Table 3: Distance of file tip from minor foramen determined by Root ZX, CanalPro and Radiograph (premolar teeth).
MF: Minor Foramen
(+) and (-) values indicate file tip beyond (+) or short (-) of the AC.
|
Distance from minor foramen (mm)
|
Root ZX
|
CanalPro
|
Radiograph
|
|
n = 442
|
n = 442
|
n = 442
|
|
Canal
|
Canal
|
Canal
|
| |
MB
|
ML
|
D
|
DB
|
DL
|
PA
|
MB
|
ML
|
D
|
DB
|
DL
|
PA
|
MB
|
ML
|
D
|
DB
|
DL
|
PA
|
|
-1.0
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
|
-0.5
|
2
|
2
|
-
|
-
|
-
|
-
|
6
|
15
|
17
|
-
|
-
|
8
|
10
|
-
|
20
|
-
|
-
|
10
|
|
MF
|
60
|
56
|
73
|
21
|
19
|
53
|
61
|
54
|
59
|
19
|
19
|
18
|
16
|
13
|
16
|
11
|
05
|
4
|
|
+0.5
|
53
|
40
|
22
|
12
|
12
|
17
|
43
|
46
|
23
|
17
|
18
|
29
|
56
|
36
|
42
|
13
|
15
|
23
|
|
+0.5
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
-
|
43
|
34
|
26
|
11
|
12
|
26
|
Table 4: Distance of file tip from minor foramen determined by Root ZX, CanalPro and Radiograph (molars).
MF: Minor Foramen
(+) and (-) values indicate file tip beyond (+) or short (-) of the AC.
The measurements obtained by the two EALs and radiographs relative to the actual location of the minor foramen were compared using a paired samples t test, X2 test and a repeated measure Anova evaluation was conducted at the 0.05 level of significance.
For anterior teeth, the Root ZX, CanalPro and radiographs located the minor foramen 83%, 70% and 22% of the time, respectively. For premolar teeth, the Root ZX, CanalPro and radiographs located the minor foramen 75%, 64% and 28% of the time, respectively. For molar teeth, the Root ZX, CanalPro and radiographs located the minor foramen 63%, 51% and 14% of the time, respectively. There was no statistically significant difference between the two EAL but there was a difference when the EAL and radiographs were compared (Tables 2, 3 and 4).
For anterior, premolar and molar teeth, none of the measurements was 1.0 mm short of the minor foramen. For anterior and premolar teeth, none of the measurements was 0.5 mm short of the minor foramen but for molar teeth 1%, 7% and 8% of the measurements using the Root ZX, CanalPro and radiographs, respectively were short.
For anterior teeth, the Root ZX, CanalPro and radiographs were 0.5 mm long of the minor foramen a 17%, 30% and 52% roots respectively. For premolar teeth, the Root ZX, CanalPro and radiographs were 0.5 mm long of the minor foramen 25%, 85% and 53% roots respectively and for molar teeth, it was 34%, 36% and 40%, respectively.
No EALs measurements were 1.0 mm long of the minor foramen for anterior, premolar and molar teeth, but for radiographs, it was 26% for anterior teeth, 18% for premolar teeth and 31% for molar teeth. There was no statistically significant difference between the two EALs but there was a significant difference (p= 0.05) when the EALs and radiographs were compared.
The in vivo study performed to evaluate the accuracy and predictability of two EALs for determining working length as compared to radiographs. The use of electronic devices to determine WL has gained in popularity. When using them, an important consideration is being aware of the possible sources of error such as metallic restorations, salivary contamination, dehydration, anatomic structures etc. However, as shown in this and other studies, the accuracy of EAL is superior to radiographs [6,15-17].
Accurate determination of the working length is a critical step for the success of endodontic treatment. Radiography is the most commonly used technique for WL determination in clinical practice. However, it has some drawbacks. Therefore, taking into consideration the limitations of conventional radiography, the present study was designed to evaluate the accuracy of WL measurements obtained with 2 EALs and radiograph.
One of the reasons why a radiographically determined WL lacks accuracy is that it is based on the radiographic apex rather than the canal terminus - the minor foramen. WL obtained with a radiograph by positioning the tip of a file at a certain distance (usually 1.0 mm) from the radiographic apex. Nonetheless, WL should be based on the position of the minor foramen rather than the apex because the foramen frequently is not at the apex [18]. In this study, radiographs correctly located the minor foramen 22% of the time whereas for the Root ZX and CanalPro it was 83% and 70% of the time, respectively. Both EAL were within ±0.5 mm from the minor foramen 85% of the time whereas radiographs were within ±0.5 mm of 22% of cases. An in vivo study by Shabahang et al., reported that the Root ZX was within 0.5 mm from the minor foramen 96% of the time, a value similar to the present findings [19]. In general, this study also agrees with others that EAL are more accurate than radiographs and greatly reduce the risk of instrumenting and filling short or beyond the canal terminus [20].
Since the minor foramen varies in location and anatomy (sharply defined, parallel, or missing), caution should be used to avoid over -estimating working length [10]. According to Gutierrez & Aguayo over-instrumentation of the root canal must be a common and undetected occurrence [7]. An instrument passing through a necrotic pulp and through the foramen most likely carries bacteria and toxins into the apical tissues [21,22]. An indication by an EAL of reaching the minor foramen or foramen is very helpful in avoiding mishaps. Indeed, this study showed that WL obtained with radiographs was 1.0 mm long of the AC 34% of the time but 0% for the two EAL. This high incidence of error is clinically important because a WL 1.0 mm long would result in canals instrumented outside the foramen.
Using an EAL as an aid to endodontic therapy could also help to reduce radiation dose required for WL determination, thereby reducing the radiation hazard to the patient. Under the ex vivo conditions of this study, it can be concluded that there was no significant difference between the accuracy of the 2 EALs in determining the WL when compared with conventional radiography.
I affirm that I/We have no financial affiliation (e.g., employment, direct payment, stock holdings, retainers, Consultantships, patent licensing arrangements or honoraria), or involvement with any commercial organization with direct financial interest in the subject or materials discussed in this manuscript, nor have any such arrangements existed in the past three years. Any other potential conflict of interest is disclosed.
Under clinical conditions, the EALs identified the minor foramen with high degree of accuracy. EAL were more accurate, compared to radiographs with the potential to greatly reduce the risk of instrumenting and filling beyond the apical foramen.