
Component Separation or Mesh Repair for Ventral Hernia Repair - The Role of Mesh in Covering all the Abdominal Wall in the Component Repair
*Corresponding Author(s):
Eldo E FrezzaEastern New Mexico University, Health Science Center, Roswell NM, United States
Tel:+1 9563577355,
Email:eefrezza@msn.com
Abstract
Simple repair of the hernia opening, Ventral Hernia Repair (VHR) has been confronted by a more definitive goal of restoration of abdominal muscular strength and wall function accomplished by mobilizing abdominal wall muscles and closing with inlay mesh, Component Separation Repair (CSR). Our observation was based on the notion that shear forces cause herniation and therefore that is an affliction of the entire abdominal wall, not a localized event. We took that information and we compare a series of VHR patients with a series of CSR pa-tients would provision evidence to improve the relative value of the techniques.
Material: Retrospective comparison of 30 consecutive CSR patients and 30 consecutive VHR patients was obtained. All abdominal wall hernia defects were at least 10 cm2 in size. T tests with unequal variances were used to evaluate differences in means of continuous variables and to estimate 95% confidence intervals of differences.
Results: Although CSR patients were older, had higher BMI’s and higher ASA scores than did VHR patients, the odds of recurrence for CSR patients were less than for VHR patients (P<0.0001). Differences in respects to ileus and wound complications, while they favored CSR patients, might have been due to chance (P>0.05 for each analysis). In VHR group 11 patients required CSR after 9-24 months, 14 patients have prolonged ileus. In the CSR group two patients were reoperated for removal of midline skin changes, two for severe seromas requiring wash up of the subcutaneous and fascia area and placement of a wound vacuum on top of the mesh.
Conclusion: This study supports the notion that a ventral hernia reflects a defect in the abdominal wall not just the point at which the hernia forms. To avoid a point of rupture, we support highly the CSR technique, since hernia is an abdominal disease not just a hole.
Keywords
INTRODUCTION
The correction of abdominal wall hernias has presented a surgical challenge for decades. Simple repair of the hernia opening, Ventral Hernia Repair (VHR), has been confronted by a more definitive goal of restoration of abdominal muscular strength and wall function, accomplished by mobilizing abdominal wall muscles and clos-ing with inlay mesh, Component Separation Repair (CSR) [1]. CSR mobilizes fresh muscle medially to reinforce the region of herniation, while preserving fascia associated muscle, and fascia of the rectus muscle, with closure at the line a alba [1]. Both synthetic and non-synthetic mesh has been used for VHR and CSR; non-synthetic mesh, now more popular because of its decreased infection risk, has been derived from human dermis, porcine dermis and bovine small intestinal submucosa [2,3].
The abdominal wall has been exposed to many shear force stress during a life cycle from exercise to pregnancy, from aging to support extra weight in the obesity scenario and wall function [4,5]. We understand that all her-nias repair need a mesh, but we hypothesize that by placing the mesh after mobilization of the muscle decrease the tension on the mesh and therefore decrease the recurrences. We retrospectively compare a cohort of VHR patients with one of CSR patients with similar age and BMI with the provision evidence to resolve the relative value of the techniques. Our Hypothesis was that the CSR patient will have fewer recurrences than VHR specif-ically in the case a mesh will used to cover all the abdominal wall and not just part of it during the repair.
MATERIALS AND METHODS
Comparisons of CSR and VHR patient series
| CSR | VHR | |||
| Continuous Variables | Mean (SD) | Mean (SD) | P* | Difference (95% CI) |
| Age(y) | 59 (7) | 48 (5) | <0.0001 | 11 (8, 14) |
| BMI kg/m2 | 48 (8) | 39 (5) | <0.0001 | 9 (6, 12) |
| Size Hernia (cm) | 18 (5) | 12 (2) | <0.0001 | 6 (4, 8) |
| OR time (min) | 125 (35) | 118 (65) | 0.6 | 7 (-20, 34) |
| Categorical Variables | N (%) | N (%) | P** | Odds Ratio (95% CI) |
| ASA 1 | 0 (0%) | 0 (0%) | ||
| ASA 2 | 6 (20%) | 15 (50%) | ||
| ASA 3 | 20 (67%) | 12 (40%) | ||
| ASA 4 | 4 (13%) | 3 (10%) | ||
| Total | 30 (100%) | 30 (100%) | 0.048 | N/A |
| Ileus | 6 (20%) | 14 (47%) | ||
| No Ileus | 24 (80%) | 16 (53%) | ||
| Total | 30 (100%) | 30 (100%) | 0.0539 | 0.29 (0.07, 1.02) |
| Wound Problems | 4 (13%) | 7 (23%) | ||
| No Wound Problems | 26 (87%) | 23 (77%) | ||
| Total | 30 (100%) | 30 (100%) | 0.51 | 0.51 (0.10, 2.32) |
| Reoperation | 0 (0%) | 11 (37%) | ||
| No Reoperation | 30 (100%) | 19 (63%) | ||
| Total | 30 (100%) | 30 (100%) | 0.0003 | 0.00 (0.00, 0.30) |
**Two tailed Fisher exact test
VHR Group
1. Ventral hernia
2. Incisional Hernia
3. Follow up more than 36 months
CSR Group
1. Ventral hernia
2. Incisional hernia
3. Recurrent ventral hernia
4. Failure of other procedures
5. Follow up more than 36 months
Patient were selected to match age and gender to create 2 cohorts, similar to achieve a good potential compari-son. The number 30 was based on the potential to obtain statistical significant analysis.
Surgical techniques
Component Surgical Repair (CSR)
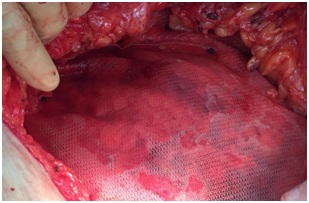 Figure 1: Phasix mesh in place after CSR.
Figure 1: Phasix mesh in place after CSR.Mesh was then inspected for tightness and wrinkles; wrinkles, seen in only two patients, were repaired with fig-ure-of-eight stitches to fascia. The abdominal wall was then washed with saline. Two Jackson-Pratt #10 drains were inserted on each side of the flank coming down to the pubis area, secured to skin with 2-0 nylon. Subcutis was reapproximated with 2-0 vicryl. Skin was closed with staples. One dose of first generation cephalosporin was given before surgery; one dose, after surgery.
Ventral Hernia Repair (VHR)
Mesh used
Postoperative care
Patient follow up was as follow: 2 and 6 weeks. 3-6-9-12 months then every six months.
Our follow up was: 48+9 months in VHR group and 38+6 months in CSR group.
Statistical methods
RESULTS
Table 1 displays the data and statistical analyses for this study. Although CSR patients were older, had higher BMI’s and higher ASA scores than did VHR patients, the odds of recurrences for CSR patients were less than for VHR patients (P<0.0001). Differences in respects ileus and wound complications, while they favored CSR patients, might have been due to chance (P>0.05 for each analysis).
One patient was discharged after twenty-one days; three patients after nine days. Discharge delays stemmed from extensive lysis of adhesions with associated ileus. One patient developed pneumonia postoperatively re-quiring a pulmonary consult and a bronchoscopy with lavage. She went home on postoperative day #9 with antibiotics. No surgical complications were found. All the patients got the drainage out within 2 weeks since all the patients followed up 1 week after surgery with us in the office where the Jackson-Pratt was taken off, and in the case of the patient that stayed longer, both the Jackson-Pratt and the staples were taken out in appropriate time which is 1 week after surgery for the Jackson-Pratt and 2 weeks for removal of the staples. In VHR group 11 patients required CSR after 9-24 months, 14 patients has prolonged ileus, 7 had seroma required interven-tional radiology drainage. In the CSR group 1 patient that had the surgery plus very extensive lysis of adhesions which we waited 4 days when she had some flatus before starting to be fed, and she spent almost 3 weeks in the hospital. In the CSR group two patient were reoperated for removal of midline skin changes, two for severe se-romas requiring wash up of the subcutaneous and placement of a wound vacuum.
DISCUSSION
Abdominal wall defect represents is a surgical challenge, given that in many years we did not achieved a con-sensus on what was the best operation. It requires appropriate management and decision making for acceptable results [5,6]. CSR and VHR have been employed satisfactorily when mesh has been used, with CSR being recommended when fistula is present, when infection is likely, and after ileostomy or colostomy closure [6-8]. In general CSR has been using for complex cases and given that a non absorbable mesh is rarely indicated given the risk of infection, as in our case when we have to close the gap we always used the porcine derived mesh which is more resistant to infections and do better in case we need to use wound vacuum. This paper shows, in terms of reoperative rates, a marked preference for CSR as a first-choice procedure, a recommendation that concurs with the findings of others [9]. What the physical experiments demonstrated was that differences in reoperative rate might relate to the body habitus and local factors with respect to the abdominal wall strength [4]. Based on this research we thought that one way to improve the strength of the abdominal wall was to reinforced the abdomen by placing an absorbable mesh from the relaxing incision.
The issue remains to decide which operative procedure are the best. Lately the CRS has become more popular given the recurrence of the regular mesh repair and the technical difficulty of the rives stoppa repair procedure which precludes its application to all patients on a routine basis, its low reoperation rate not with standing [10]. A partitional technique involving component separation and fascia-fascia closure has both high risk of short term post-operative complications, as well as a long operative time [11]. Open ventral hernia repair with com-ponent separation is appropriate for complex hernias, not simply hernias in patients with infection or other rela-tively simple problems [12]. Staging of the ventral hernia has been helpful in surgical decision and in post-operative comparison of results [13]. The open intraperitoneal technique is appropriate for complex incisional hernias occurring in obese patients, but is contraindicated when laparoscopic access has been obtained; minimal access was shown to be feasible in patients with a larger mesh of 15 cm [14-16]. A cellular dermal matrix has been also suggested in this cases to resist to infection as well as porcine [3,17]. Open component separation, which allows autologous tissue repair with approximation of a midline fascia in patients with complex hernias, creates large skin flaps that prevent the visualization of epigastric vessels; this problem notwithstanding recurrence rates is similar for open and laparoscopic techniques [14,15,17]. Although there is a trend towards laparoscopic surgery the laparoscopic repair does not resolve the matter of the ventral hernia’s being a problem with the abdominal wall [18-23]. Component graph separation, used to correct large ventral hernias, can yields complications in few patients but this was also an early paper where this surgery was done in complicated cases [24,25]. Posterior repair have been showed similar results, if not better overall [12,26].
As showed by early research a good abdominal reconstruction was improving the physiology of the abdominal wall [4]. In our experience the CSR patient despite presented with more risk factors (higher BMI and higher ASA classification risk) did better than the VHR patient as far as recurrences since the repair was not aimed to close the abdomen gap but to mobilizing and reinforce the whole abdominal wall with a large absorbable mesh, which in our opinion was the major key for the success of our CSR procedures.
These last evidences together with the failing of the above described procedures have been the basic force for surgeons to find alternative procedure like the CRS.
On top of that there are same physic evidence could be garnered from evaluation of elastic band experiments to support or deny the notion that shear forces cause herniation and therefore that is an affliction of the entire abdominal wall, not a localized event. These observations, were emphasized by our tensile experiments, where we showed that a thicker elastic material holds more weight than a thinner one despite similar length (P<0.0001) [27]. This gives us a way to compare different materials based upon the same cross-sectional area. The tensile strength is about 1.5 times the shear strength in material. If then we considered the length of the rubber band we notice that comparing bands with the same thickness the difference in strength is significant different with a confidence level of a=95, making the short band the strongest. We are doing more works in this arena to com-pare tensile strength in elastic materials that would accurately model the muscle tissue strength by calculating the shear forces able to break a hernia repair with mesh. The “snap point” is closed to the suture line as we found often in clinical scenario. It would be helpful to compile clinical data that would identify if failure is be-tween the mesh and the muscle (as a shear force) or if the reoccurrences.
CONCLUSION
This study supported the notion that a ventral hernia reflects a defect in the abdominal wall not just the point at which the hernia forms. In our 4 years follow up we reported more recurrences in the VHR group than in the CSR one. The reoperative rates to be greater for conventional ventral hernia repair than for component separa-tion repair, even though the patients who underwent component separation repair were older, had greater body mass indexes, and more severe ASA grades. By sheer force of gravity, we increase the possibility of having a hernia, since the muscle get thinner or the stitches of previous mesh placed has too much tension. To avoid a point of rupture around the mesh and a better long term repair we support highly the CSR technique with a large mesh covering the abdominal wall, since hernia is an abdominal disease not just a hole.
REFERENCES
- Pauli EM, Rosen MJ (2013) Open ventral hernia repair with component separation. Surg Clin North Am 93: 1111-1133.
- Rosen MJ, Krpata DM, Ermlich B, Blatnik JA (2013) A 5 year clinical experience with single staged repairs of infected and contaminated abdominal wall defects utilizing biological mesh. Ann Surg 257: 991-996.
- Pomahac B, Aflaki P (2010) Use of a Non-Cross-Linked Porcine Dermal Scaffold in Abdominal Wall Reconstruction. Am J Surg 99: 22-27.
- Criss CN, Petro CC, Krpata DM, Seafler CM, Lai N, et al. (2014) Functional abdominal wall reconstruction improves core physiology and quality of life. Surgery 156: 176-182.
- Koltz PF, Frey JD, Bell DE, Girotto JA, Christiano JG, et al. (2013) Evolution of abdominal wall reconstruction: development of a unified algorithm with improved outcomes. Ann Plast Surg 71: 554-560.
- Raigani S, De Silva GS, Criss CN, Novitsky YW, Rosen MJ (2014) The impact of developing a comprehensive hernia center on the referral patterns and complexity of hernia care. Hernia 18: 625-630.
- Abdelfatah MM, Rostambeigi N, Podgaetz E, Sarr MG (2015) Long term outcomes (> 5 years follow up) with porcine acellular dermal matrix (permacol) in incisional hernias at risk for infection. Hernia 19: 135-140.
- Lasses Martínez B, Peña Soria MJ, Cabeza Gómez JJ, Jiménez Valladolid D, Flores Gamarra M, et al., (2016) Surgical treatment of large incisional hernias with intraperitoneal composite mesh: a cohort study. Hernia 21: 253-260.
- Sriussadaporn S, Sriussadaporn S, Pak-Art R, Kritayakirana K, Prichayudh S, et al. (2013) Management of difficult abdominal wall problems by components separation methods: a preliminary study in Thailand. J Med Assoc Thai 96: 1449-1462.
- Heartsill L, Richards ML, Arfai N, Lee A, Bingener-Casey J, et al. (2005) Open Rives Stoppa ventral hernia repair made simple and successful but not for everyone. Hernia 9: 162-166.
- Shih PK (2015) Difficult abdominal; wall closure: component separation versus partition technique. Hernia 19: 301-305.
- Pauli EM, Wang J, Petro CC, Juza RM, Novitsky YW, et al., (2015) Posterior component separation with transverses abdominis release successfully addresses recurrent ventral hernias following anterior component separation. Hernia 19: 285-291.
- Petro CC, O'Rourke CP, Posielski NM, Criss CN, Raigani S, et al. (2016) Designing a ventral hernia staging system. Hernia 2016 20: 111-117.
- Bernard C, Polliand C, Mutelica L, Champault G (2007) Repair of giant incisional abdominal wall hernias using open intraperitoneal mesh. Hernia 11: 315-320.
- Ferrari GC, Miranda A, Lernia SD, Sansonna F, Magistro C, et al. (2008) Laparoscopic repair of incisional hernia: outcomes of 100 consecutive cases comprising 25 wall defects larger than 15 cm. Surg Endosc 22: 1173-1179.
- Mommers EH, Wegdam JA, Nienhuijs SW, de Vries Reilingh TS (2016) How to perform the endoscopically assisted components separation technique (ECST) for large ventral hernia repair. Hernia 20: 441-447.
- Roth JS, Brathwaite C, Hacker K, Fisher K, King J (2015) Complex ventral hernia repair with a human acellular dermal matrix. Hernia 19: 247-252.
- Albright E, Diaz D, Davenport D, Roth JS (2011) The component separation technique for hernia repair: a comparison of open and endoscopic techniques. Am Surg 77: 839-843.
- Gonzalez R, Rehnke RD, Ramaswamy A, Smith CD, Clarke JM, et al. (2005) Components separation technique and laparoscopic approach: a review of two evolving strategies for ventral hernia repair. Am Surg 71: 598-605.
- Bachman SL, Ramaswamy A, Ramshaw BJ (2009) Early results of midline hernia repair using minimal invasive component separation technique. Am Surg 75: 572-578.
- Wright BE, Niskanen BD, Peterson DJ, Ney AL, Odland MD, et al. (2002) Laparoscopic ventral hernia repair: are there comparative advantages over traditional methods of repair? Am Surg 68: 291-296.
- Rosen MJ (2009) Polyester based mesh for ventral hernia repair: is it safe? Am J Surg 197: 353-359.
- Singh DP, Zahiri HR, Gastman B, Holton LH, Stromberg JA, et al. (2014) A modified approach to component separation using biological graft as a load sharing onlay reinforcement for the repair of complex ventral hernia. Surg Innov 21: 137-146.
- Rosen MJ, Bauer JJ, Harmaty M, Carbonell AM, Cobb WS, et al., (2017) Multicentric prospective longitudinal study of the recurrence, surgical site infection and quality of life after contaminated ventral hernia repair using biosynthetic absorbable mesh: the COBRA study. Ann Surg 265: 205-211.
- Fischer JP, Wink JD, Nelson JA, Kovach SJ 3rd (2014) Among 1,706 cases of abdominal wall reconstruction, what factors influence the occurrence of major operative complications? Surgery 155: 311-319.
- Jones CM, Winder JS, Potochny JD, Pauli EM (2016) Posterior component separation with transverses abdominis release: technique, utility and outcomes in complex abdominal wall reconstruction. Plast Reconstr Surg 137: 636-646.
- Frezza EE, Cogdill C, Wacthell M, Frezza EGP (2017) A Physic Tensile Forces Experiment to Possible Explain the Reason of Failing Ventral Hernia Repair. J Gastroenterol Hepatology Res 2: 007.
Citation: Frezza EE, Cogdill C, Wacthell M, Frezza EGP (2017) Component Separation or Mesh Repair for Ventral Hernia Repair? The Role of Mesh in Covering the all Abdominal Wall in the Component Repair. J Gastroenterol Hepatology Res 2: 008.
Copyright: © 2017 Cory Cogdill, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

