
Continuity of Antenatal Care Services in Chhattisgarh during COVID19
*Corresponding Author(s):
Gajendra SinghPublic Health Specialist, Indian Institute Of Health Management Research, Jaipur, India
Tel:+91 9560002061,
Email:talk2me@doctor.com
Abstract
Context: COVID 19 has enforced lockdown all-over India as a crucial step to control the infection and flatten the epidemiological curve of the disease. As Lockdown has also prohibited the gathering of people and commercial activities, this has also thrown challenge on health systems to sustain the essential health services particularly ANC services due to shift of resources towards COVID 19 response.
Aims: Study was conducted to describe pregnant women’s general concerns as well as their attitudes and preferences in relation to the COVID 19 pandemic as well as to assess the Antenatal care services and knowledge and practices among pregnant women during the pandemic of Covid-19 in Chhattisgarh. It was also an attempt to ascertain continuity of ANC services during COVID 19 pandemic.
Settings and Design: Observational, cross sectional study was conducted in eight districts of Chhattisgarh state, India
Methods and Material: Data was collected using a pre-designed and pre-tested schedule for interviews. Statistical analysis used: Microsoft Excel XLSTAT and the results were calculated in frequencies and percentages.
Results: Majority of the women (89.3%) are from 2nd and 3rd trimester. 96.7% pregnant women have done ANC visits to nearest heath facility. It is evident that coverage of ANC visits decreases from 1st ANC visit to 4th ANC visit. It is also important to note that 3.3% women have not done any ANC visits. 92.3 % pregnant women remember the date of their last ANC visit while date of last ANC visit was mentioned in MCP card for 82.7% pregnant women. More than 95% of last ANC visits were done in most critical times (15th March to 31st July 2020). In 93% cases, pregnant women visited routine places (VHND/SHC/PHC/CHC/DH) for ANC visit. 92% pregnant women covered their mouth mask/cloth during last ANC visit while in 95% cases, face was also covered by person doing ANC. 99.5% pregnant women mentioned that they have heard about COVID 19. The common source of information being front-line health worker (ASHA/Mitanin) 76.2% (1130). More than two third (69.2%) pregnant women are afraid of child delivery during uncertain times of COVID 19 followed by fear of getting infected if visit hospital for ANC (62.2%).
Conclusion: The study showed that the majority of the pregnant women believed that they were at a high risk of infection with COVID-19, and many were concerned about possible health consequences, especially for their unborn child. Almost 90% of the pregnant women isolated at home most of the time. The majority were worried about possible consequences for antenatal care. More than 60% women are afraid of giving birth in these uncertain COVID times as well as of getting infection during ANC visit to hospital.
Keywords
Antenatal Care, Mental Health, Knowledge, COVID, Chhattisgarh
Background
Health care services during pregnancy and childbirth and after delivery are important for the survival and well-being of both the mother and the infant. Antenatal care (ANC) can reduce health risks for mothers and their babies by monitoring pregnancies and screening for complications. Delivery at a health facility, with skilled medical attention and hygienic conditions, reduces the risk of complications and infections during labor and delivery. The World Health Organization (WHO) envisions a world where every pregnant woman and newborn receives quality care throughout the pregnancy. Within the continuum of reproductive health care, ANC provides a platform for important health-care functions, including health promotion, screening, and diagnosis, and disease prevention. It has been established that by implementing timely and appropriate evidence-based practices, ANC can save lives. Crucially, ANC also provides the opportunity to communicate with and support women, families, and communities at a critical time in the course of a woman’s life. Antenatal care is the importance of providing effective communication about physiological, biomedical, behavioral, and sociocultural issues, and effective support, including social, cultural, emotional, and psychological support, to pregnant women in a respectful way. These communication and support functions of ANC are key, not only to saving lives but to improving lives, health-care utilization, and quality of care. Women’s positive experiences during ANC and childbirth can create the foundations for healthy motherhood [1].
Pregnant women represent a uniquely vulnerable group in any infectious disease outbreak because of their altered physiology, susceptibility to infections, and compromised mechanical and immunological functions. The need to safeguard the fetus adds to the challenge of managing their health. Special precautions are required to minimize cross-infection of healthcare providers while performing procedures that require close physical contact and promote droplet exposure, such as vaginal delivery. Pregnancy is a physiological state that predisposes women to viral infection. Over and above the impact of COVID-19 infection on a pregnant woman, there are concerns relating to the potential effect on fetal and neonatal outcomes; therefore, pregnant women constitute a group that requires special attention in relation to prevention, diagnosis, and management [2]. Pregnancy is a journey of the new life of the baby however also indicates that pregnancy and childbirth complications are the leading causes of maternal mortality worldwide. Over 99% of those maternal deaths occur in low- and middle-income countries (LMICs, including India). Globally, 86% of pregnant women access antenatal care with skilled health personnel at least once, only two in three (65 percent) receive at least four antenatal visits. In South Asia during 2013-2018, 79% pregnant women access at least once antenatal visit, and 49% pregnant women received 4 ANC Checkup as recommended by WHO [3]. Maternal Mortality Ratio (MMR) of State Chhattisgarh has higher maternal mortality than the national average. As per (SRS -2015-17) Maternal Mortality Ratio (MMR) for India is 122 per 1, 00,000 live births and for Chhattisgarh is 141 per 1,00,000 live births (SRS -2015-17) [4]. In India, the proportion of pregnant women age 15-49 receiving the minimum 4 antenatal visits, in India raised from 77 percent in NFHS-3 (2005-06) to 84 percent in NFHS-4 (2015-16), and in NFHS-4 79 percent received ANC from a skilled provider in NFHS-4. Fifty-nine percent of women had their first ANC visit during the first trimester of pregnancy; an increase from 44 percent in 2005-06, and 51 percent had four or more ANC visits, an increase from 37 percent in 2005-06 [5].
A comprehensive understanding of the determinants of ANC utilization in India is lacking. In the context of recent focus of Indian government on ANC services, through Pradhan Mantri Matru Vandana Yojana (PMMVY), a conditional cash transfer scheme, understanding the factors driving utilization is crucial to aid the development of informed policy. In this scheme, pregnant woman is eligible if she registers her pregnancy at Anganwadi center (AWC) within four months of conception, attends at least one prenatal care session, and is taking Iron-folic acid tablets and TT (tetanus toxoid) injection [6]. In December 2019, a cluster of four cases of pneumonia of unknown etiology in Wuhan, China, were reported to the World Health Organization (WHO) [7]. Since then, coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread rapidly across the world. On March 12, 2020 the WHO defined the outbreak as a pandemic [8]. Many countries responded by restricting freedom of movement and limiting nonemergency health care to focus resources on COVID-19 care provision [9]. As pregnant women are at greater risk of complications and severe disease from infection with other coronaviruses, including Severe Acute Respiratory Syndrome (SARS) and Middle Eastern Respiratory Syndrome (MERS), they were identified as a vulnerable group and were advised to take additional precautions as the COVID-19 pandemic unfolded [10-12].
To control the spread of the infection, lockdown was enforced all-over India as well as in all districts of Chhattisgarh. Strict restriction was enforced on movement of commercial vehicles, opening of shops, hotels, markets etc. to avoid social gathering and movement of people to control the spreading of virus. Lockdown was a crucial step to control the infection and flatten the epidemiological curve of the disease, but it has had significant effects on the lives of the people especially the poor, who have lost their livelihoods and are struggling for basic needs of lives like food and shelter. The constant fear of the infection is likely to affect the mental health of people. Apart from Govt. and private offices, shops and other establishments, colleges, schools, Anganwadi Centers are also closed. Midday meals in schools as well as distribution of take-home ration, hot meal/egg distribution in Anganwadi Centers to children, pregnant and lactating mothers and other beneficiaries are on halt. As Lockdown has also prohibited the gathering of people and commercial activities, this has also thrown challenge on health systems to sustain the essential health services particularly ANC services due to shift of resources towards COVID 19 response.
Essential services were prioritized in their efforts to maintain continuity of service delivery during an outbreak of COVID-19 which include services related to reproductive health, including care during pregnancy and childbirth as highly recommended by World Health Organization [13]. It is important health care providers should be aware that pregnant women with COVID-19 and their newborn babies may be more likely to need specialist care and those women and their babies have access to this care. This is particularly true for pregnant women with COVID-19 alongside other commodities [14]. One of the major challenges during this lockdown period was uninterrupted provision of Maternal and Child health services vaccines at the state, regional and district level due to restricted movement within state and within districts also. It also affected the supply chain at all levels. Another risk is the public exposure and non-adherence to social distancing by people working in MCH service delivery. The scarcity of basic protection measures in adequate quantity aggravates the problem. Another critical challenge was that common public could start believing that that essential health services like ANC are also closed, as lockdown has ensured closure of majorly all type of services and institutions. This was further strengthened by closure of Anganwadi Centre at many places. Mobilizing beneficiaries to VHND / ANC Site was a challenge. Travel of ANM to the remote areas during the time of lockdown was key challenge. Lack of awareness made the adherence to physical distancing difficult during VHND and ANC. Moreover, tribal communities are quite social and believe in close interactions. Another challenge was the limited availability of masks and gloves for frontline health workers like ANMs and Mitanins.
Aim of the Study
This paper aimed to describe pregnant women’s general concerns as well as their attitudes and preferences in relation to the COVID 19 pandemic as well as to assess the Antenatal care services and knowledge and practices among pregnant women during the pandemic of Covid-19 in Chhattisgarh. It was also an attempt to ascertain continuity of ANC services during COVID 19 pandemic.
Methodology
Study design and setting
A Community based cross-sectional design was conducted during June -July 2020 in 8 districts of Chhattisgarh. The selected districts were Jashpur, Koriya, Surguja, Surajpur, Kanker, Janjgir Champa, Gaurella Pendra Marwahi and Bilaspur. Districts were selected on convenience basis as mobility was limited and State Health Resource Center (SHRC) is having field staff based in these districts for Maternal and Child Health project. These all selected districts located in a different geographical zone in Chhattisgarh. 20 blocks were selected from these 7 districts and a simple random sample was used to select 3 Sub health centers from each block. The target population was all pregnant women registered with all 3 Sub health centers from each block and residing in same area. The study covered pregnant women who give informed consent to participate in the study during the data collection. Ethical clearance was obtained from the Institutional Ethics Committee of State Health Resource Center, Raipur, and Chhattisgarh.
Sample size
The calculated sample size was of 425 pregnant women to be collected in duration of 1st June to 31st July 2020. This was calculated using proportion formula and assuming the proportion of knowledge and practice of preventive measures against COVID-19 is 50% since there was no study in Chhattisgarh. The sample size was calculated based on an expected Confidence Interval (CI) 95%, margin of error (d) 5%, and considering a non-response rate of 10%. However, the final sample collected was 1483 from 8 districts in the above mentioned duration.
Data Collection and Data Analysis
The Data were collected via face-to-face interview technique, using a structured and pretested questionnaire through Kobo Collect Mobile Application. Data were collected by trained field staff and applying all the possible strict preventive measures during the data collection. After the data collection data were analyzed using STATA.
Operational Definition
Antenatal care coverage (at least one visit) is the percentage of women age 15 to 49 with a live birth in a given period that received antenatal care provided by skilled health personnel (doctor, nurse, or midwife) at least once during pregnancy. Antenatal care coverage (at least four visits) is the percentage of women aged 15 to 49 with a live birth in a given period that received antenatal care four or more times.
Results
Sample profile-Social-Demographic Profile
The study included 1483 pregnant women from 8 districts. 47.1% (698) of the pregnant women belonged to 20-24 year age group and majority of pregnant women 31% (464) have completed high school followed by Middle school 21.3% (316) while 11.1% (165) did not receive any formal education. 1477 women were married while 6 were separated/ divorced (Table 1).
|
Characteristics |
Social-Demographic Profile (n=1483) |
||
|
|
Frequency |
Percentage |
|
|
Age of Pregnant women |
15-19 Years |
115 |
7.8 |
|
20-24 Years |
698 |
47.1 |
|
|
25-29 Years |
501 |
33.8 |
|
|
30-34 Years |
141 |
9.5 |
|
|
above 34 years |
28 |
1.8 |
|
|
Education |
No education |
165 |
11.1 |
|
Primary |
201 |
13.5 |
|
|
Middle school |
316 |
21.3 |
|
|
High School |
464 |
31.2 |
|
|
Higher Secondary |
262 |
17.6 |
|
|
Graduation and above |
75 |
5.3 |
|
|
Place of Residence |
Rural |
1440 |
97.1 |
|
Urban |
43 |
2.9 |
|
|
Occupation |
Housewife |
958 |
64.6 |
|
Farmer |
379 |
25.6 |
|
|
Job |
14 |
0.9 |
|
|
Self employed |
15 |
1.0 |
|
|
Unemployed |
96 |
6.4 |
|
|
Others (Unorganized Sector) |
21 |
1.4 |
|
|
Religion |
Hindu |
1405 |
94.7 |
|
Christian |
62 |
4.1 |
|
|
Muslim |
16 |
1.2 |
|
Table 1: Social-Demographic Profile
Antenatal Services
Majority of the women (89.3%) are from 2nd and 3rd trimester. 365 (24.6%) are from 8th and 9th month of pregnancy. It highlights the need of ANC services especially during COVID. As per the MCP card, Hb data was available for 1232 beneficiaries. Majority of them (>75%) are suffering from mild, moderate or severe anemia (Figure 1 & 2)
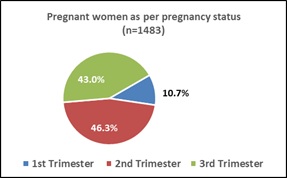
Figure 1: Pregnant women as per pregnancy status
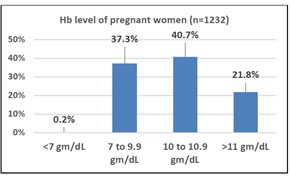 Figure 2: Hb level of pregnant women
Figure 2: Hb level of pregnant women
1434 pregnant women have done ANC visits to nearest heath facility. Out of those, 19% pregnant women have done 4 or more ANC visits at the time of survey. 49 pregnant women have not done any ANC visits till now. To analyze the timely ANC visits, we followed the guidelines from Ministry of Health and Family Welfare, Govt. of India which says that 1st ANC is recommended as soon as the period is missed or within first three months of missing the period, 2nd ANC Checkup In 4th - 6th month of pregnancy. 3rd ANC Checkup in 7th - 8th month of pregnancy. 4th ANC Checkup In 9th month of pregnancy [15] (Figure 3 & 4).
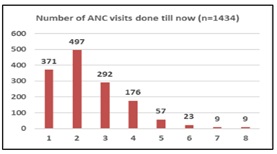 Figure 3: Number of ANC visits done
Figure 3: Number of ANC visits done
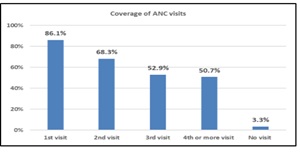 Figure 4: Coverage of ANC visits as per schedule
Figure 4: Coverage of ANC visits as per schedule
Antenatal care models suggest that a minimum of four ANC contacts are required to reduce perinatal mortality and improve women experience of care. Figure 3 shows that 50.7% of pregnant women had 4th or more ANC visits followed by 84.8% who had at least 1st ANC visit belongs to first trimester. It is evident that coverage of ANC visits decreases from 1st ANC visit to 4th ANC visit. It is also important to note that 3.3% women have not done any ANC visits.
Last visit for Antenatal Care
92.3 % pregnant women remember the date of their last ANC visit while date of last ANC visit was mentioned in MCP card for 82.7% pregnant women. It’s important to note that 68% of pregnant women remember date of their last ANC visit correctly (as per MCP card). More than 95% of last ANC visits were done in most critical times (15th March to 31st July 2020). In 93% cases, pregnant women visited routine places (VHND/SHC/PHC/CHC/DH) for ANC visit while in 7% cases, private hospitals were visited. 44.3% women availed the last ANC through walk (SHC/VHND) and 51% availed it through private vehicle while Govt. vehicle was used by 4.7% pregnant women. In all cases, pregnant women were attended by ANM/ Nurse/ Doctor. Date of Last Menstrual Period (LMP) was mentioned in MCP card of 83.7% women while EDD was mentioned for 80.1% pregnant women. Out of the 295 women (EDD not mentioned in MCP card), 42 women were in 8th and 9th month of pregnancy. In their last ANC visit, weight was taken for 90.8%, BP was measured for 96% and TT was given to 95.6% pregnant women. For 87.1 % pregnant women, Health worker / Mitanin / ANM have told about place of delivery (nearest health facility i.e. SHC / PHC / CHC / DH) for childbirth and Mahtari sewa/ Ambulance service (102/108) during their last ANC visit. 89% of pregnant women have received the IFA tablet during last ANC visit. However, only 57% pregnant women received ration from Anganwadi in last month. 76.9% pregnant women mentioned that Hb was tested while as per MCP card Hb was tested for 79.7% women in their last ANC visit. Similarly, pregnant women were asked about other critical services received in last ANC visit which were later confirmed with entries in MCP card (Table 2).
|
Characteristic |
As per pregnant women (N=1483) |
As per MCP card (N=1483) |
|
Hemoglobin test |
76.9 % |
79.7 % |
|
Urine pregnancy test |
68.5 % |
59.9 % |
|
Urine test for sugar, albumin |
47.1 % |
NA |
|
Abdominal Examination/Fetal movements |
47.4 % |
51.7 % |
|
Abdominal Examination/Fetal Heart Rate |
38.8 % |
35.5 % |
|
Blood test for sugar |
46.4 % |
46.5 % |
|
Blood Pressure |
87.7 % |
NA |
|
Sickle cell test |
23.2 % |
28.8 % |
|
Malaria test |
38.7 % |
NA |
|
Other Investigations |
5.1 % |
12.7 % |
|
USG |
NA |
72.2 % |
|
HIV Screening |
NA |
34.5 % |
NA = Data not available
Table 2: Services during last ANC visit.
92% pregnant women covered their mouth mask/cloth during last ANC visit while in 95% cases, face was also covered by person doing ANC. In 38 (2.5%) cases, none of them (pregnant women and person doing ANC) have covered the face by mask / cloth during last ANC. Other safety measures were also taken by person doing ANC such as gloves (88.4%) and hand washing (92.7%). During ANC, tips for protection from COVID was also given to 85.9% pregnant women. Overall, 78.4% pregnant women felt satisfied with services received in ANC visit during lockdown.
Awareness and practices for COVID 19
99.5% pregnant women mentioned that they have heard about COVID 19. The common source of information being front-line health worker (ASHA/Mitanin) 76.2% (1130), followed by mobile phone 58.5% (868), ANM 56.7% (841), television 44.9% (667) followed by Doctors 29.1% (432) (Table 3).
|
Source of Information |
Frequency |
Percentage |
|
Mitanin/ASHA |
1130 |
76.2 |
|
Mobile phone (Recorded message) |
868 |
58.5 |
|
ANM |
841 |
56.7 |
|
Television |
667 |
44.9 |
|
Family member |
541 |
36.4 |
|
Doctor |
432 |
29.1 |
|
MPW |
422 |
28.4 |
|
News Channel |
382 |
25.7 |
|
Wall writing |
350 |
23.6 |
|
|
232 |
15.6 |
|
Public Announcement |
212 |
14.3 |
|
News Paper |
203 |
13.6 |
|
Radio |
162 |
10.9 |
|
Internet |
131 |
8.8 |
|
Social Media |
103 |
6.9 |
*Multiple response, Arranged in decreasing order of percentages
Table 3: Source of Information about COVID 19 *(n=1483)
Pregnant women were asked about if they are aware about symptoms of COVID 19. Majorly, they are aware about all key symptoms. However, the ley symptom (difficulty in breathing) was not known to 24% women as well as 17 (1.1%) were not aware of any symptoms of COVID 19. The study shows that knowledge about symptoms of Covid-19, 93.3% (1384) of pregnant women know about fever as one of the most common symptoms, followed by cough 96.4% (1430), running nose 82.5% (1224) and difficulty in breathing 76.5% (1135) (Table 4).
|
Characteristic |
Frequency |
Percentage |
|
Fever |
1384 |
93.3 |
|
Cough |
1430 |
96.4 |
|
Running Nose |
1224 |
82.5 |
|
Difficulty in breathing |
1135 |
76.5 |
|
Not aware |
17 |
12.7 |
*Multiple response, Arranged in decreasing order of percentages
Table 4: Awareness about symptoms of COVID 19 *(n=1483).
Women were also asked about the practices they are following which can protect them from COVID 19 infection. Almost 96.8% (1435) reported practicing hand washing, 96.1% (1425) were using mask, 86.1% (1277) avoided to visit crowded place, 80.2% (1174) followed physical distancing, 58.7% (860) avoided touching their eyes, mouth and nose and around 0.5% (8) forgot to take any precaution (Table 5).
|
Practices for prevention from COVID 19 |
Frequency |
Percentage |
|
Repeated hand washing |
1435 |
96.8 |
|
Using mask |
1425 |
96.1 |
|
Avoid crowded places |
1277 |
86.1 |
|
Physical distancing |
1174 |
79.2 |
|
Covering mouth by mask/cloth while coughing/sneezing |
997 |
67.2 |
|
Avoid touching your eye, mouth and nose |
860 |
58.0 |
|
No Precaution |
8 |
0.5 |
*Multiple response, Arranged in decreasing order of percentages
Table 5: Practices for prevention from COVID 19 *(n=1483)
Mental Health of pregnant women during COVID 19
Pregnant women were also asked about their three biggest concern during lockdown. Table no. 5 shows that about half of pregnant women i.e. 48.4% (718) reported no source of income as the biggest concern followed by anticipated shortage of food items / grocery during the lock-down period (48.2%). Every fourth woman (25.5%) feel mental stress/depression and worry regarding infection as main concern. It’s also important to note that 4.2% pregnant women have mentioned domestic violence as main concern while 5.5% have a concern of more work at home (Table 6).
|
Characteristics |
Frequency |
Percentage |
|
No source of income during lockdown |
718 |
48.4 |
|
Shortage of food items/grocery |
715 |
48.2 |
|
Restrictions to meet friends, family and relatives |
699 |
47.1 |
|
Difficulty in buying medicines or other materials |
535 |
36.1 |
|
Shortage of daily use material like soap, shampoo |
390 |
26.3 |
|
Mental stress/Depression & worry regarding infection |
379 |
25.5 |
|
More work at home |
82 |
5.5 |
|
Domestic violence |
63 |
4.2 |
|
No worried at all |
210 |
14.1 |
*Multiple response, Arranged in decreasing order of percentages
Table 6: Concern of pregnant women during lockdown* (n=1483)
Women were also asked if they feel sad/depressed due to COVID 19 or they are losing confidence due to scenario because of COVID 19. Almost half (49.5%) pregnant women reported that they are feeling “more” or “much more” sad or depressed than earlier due to situation because of COVID 19. Similarly, 30.7% women feel that they are losing self-confidence “more” or “much more” than earlier due to COVID 19 (Figure 5 & 6).
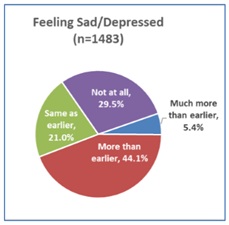 Figure 5: Women feeling sad / depressed due to COVID 19
Figure 5: Women feeling sad / depressed due to COVID 19
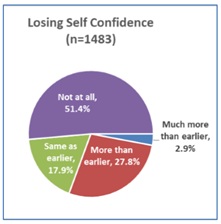 Figure 6: Women losing self-confidence due to COVID 19
Figure 6: Women losing self-confidence due to COVID 19
More than two third (69.2%) pregnant women are afraid of child delivery during uncertain times of COVID 19 followed by fear of getting infected if visit hospital for ANC (62.2%). Half of the women (50.5%) are being afraid that CVOID is not curable as well as death is sure (5.6%). Almost one fifth (19.4%) are afraid of decrease in income subsequently leading to shortage of food due to COVID 19 (Table 7).
|
Characteristics |
Frequency |
Percentage |
|
To give birth a child |
943 |
69.2 |
|
If I will go for ANC checkup in Hospital, I will be infected |
847 |
62.2 |
|
No cure available of Corona Virus |
688 |
50.5 |
|
Decrease in Income / Food |
288 |
19.4 |
|
Death is sure |
77 |
5.6 |
Table 7: Fear of pregnant women during lockdown* (n=1483)
Discussion
Pregnant women are known to be disproportionately affected by respiratory illnesses, which are associated with increased infectious morbidity and high maternal mortality rates. Pregnant women represent a vulnerable group in any infectious disease outbreak because of their altered physiology, susceptibility to infections, and compromised mechanical and immunological functions [16]. Antenatal care is the importance of providing effective communication about physiological, biomedical, behavioral, and sociocultural issues, and effective support, including social, cultural, emotional, and psychological support, to pregnant women in a respectful way. These communication and support functions of ANC are key, not only to saving lives but to improving lives, health-care utilization, and quality of care. Women positive experiences during ANC and childbirth can create the foundations for healthy motherhood [17].
The present study assesses the continuity and utilization of ANC services during the lockdown period in the Chattisgarh state due to COVID-19. As 64.6% of pregnant women are housewife and 11.1% women are with no formal education, this group may be less aware. Hence, proper efforts should be taken to reach out to this cohort so they can be more vigilant about symptoms and can take necessary steps to be taken for prevention from COVID19. Majority of the women (89.3%) are from 2nd and 3rd trimester. 365 (24.6%) are from 8th and 9th month of pregnancy. It highlights the need of ANC services especially during COVID. As per the MCP card, Hb data was available for 1232 beneficiaries. Majority of them (>75%) are suffering from mild, moderate or severe anemia. These women need utmost care, especially during COVID when routine health monitoring gets compromised.
Overall coverage of ANC visits is great (97%). It is evident that coverage of ANC visits decreases from 1st ANC visit to 4th ANC visit as only 50% pregnant women have taken 4 or more ANC visits. The coverage of ANC visits needs to be improvised and efforts should be made to ensure that already registered pregnant women who have done 2 or 3 visits also should take 4th visit also. 68% of pregnant women remember date of their last ANC visit correctly (as per MCP card) which reflects the rapport and coordination between ANM/Mitanin and the pregnant women. It is also significant to note that more than 95% of last ANC visits were done in most critical times (15th March to 31st July 2020), when many other services were hampered due to COVID. In 93% cases, pregnant women visited routine places (VHND/SHC/PHC/CHC/DH) for ANC visit while in 7% cases, private hospitals were visited. In all cases, pregnant women were attended by ANM/ Nurse/ Doctor which is a good indicator of healthcare availability during COVID19. It was also seen that all the routine services were provided during ANC visit which reflects that quality of agency visits are not compromised. Overall satisfaction rate among pregnant women for ANC services is 78% which is quite satisfactory. Another issue observed was a mismatch between the services mentioned in the MCP card versus as told by pregnant women. There should be proper training to health care workers to communicate the pregnant woman well about the services provided to minimize ambiguity as well as they are well aware about the services given. Only 57% pregnant women received ration from Anganwadi in last month because Anganwadi centers were closed initially.
During ANC visits, COVID appropriate behavior was well adapted and practiced by pregnant women as well as healthcare workers providing ANC services. This is possible because messaging regarding adherence to COVID appropriate behavior has reached well to every pregnant woman as well as healthcare workers. As Chhattisgarh faces issue of geographical access as well as LWE extremism, community mobilization relies mainly on Mitanin (ASHA). 76% pregnant women knows about COVID through Mitanin. The study shows that 93.3% (1384) of pregnant women know about fever as one of the most common symptoms, followed by cough 96.4% (1430), running nose 82.5% (1224) and difficulty in breathing 76.5% (1135). More than 80% pregnant women follow protocols like repeated hand washing, use of mask, avoiding crowded places and physical distancing.
There is well evident continuity of ANC services and adherence to COVID appropriate behavior during ANC. It could be possible because of following reasons
- a.Much before Ministry of Health and Family Welfare, State Govt. has issued a letter to all districts on 20th March 2020 for ensuring all essential services including immunization at health facilities as well as in community.
- b.Lockdown was announced on 24th March 2020. State Government with support of SHRC and other development agencies was closely monitoring the districts to understand the ground reality of program implementation particularly MCH services. It was observed that there was lack of clarity at district level on continuation of services as well as there was poor monitoring at state level because everyone was involved in COVID response. To ensure better monitoring of these services at field level, state had issued an order (30 March) appointing three Deputy Directors to monitor the essential services including MCH services and immunization at division level. Based on State letter, letter was issued on 31 March to districts.
- c.State also developed the checklist for effective monitoring at district level on weekly basis. Based on best available resources and guidance available, state also issued guideline (02 April) to continue ANC services as a part of VHSND for all the districts.
- d.To keep the morale high of Mitanin in tough times, State Govt has issued a letter with guidance on involvement in all essential services.
- e.State, with support from development partners, created IEC material specifically for front line worker which can be easily shared on social media for wider reach.
- f.District administrations also supported frontline health workers as well as others by issuing temporary security pass for ease of movement in the district during VHSND.
Pregnant women were also asked about their three biggest concern during lockdown. Apart from concerns like income, anticipated shortage of food items / grocery during the lock-down period, the other key concern was mental stress/depression and worry regarding infection (25.2%). It needs to be addressed through proper awareness and necessary steps at community / facility level. There is significant proportion of females which expressed that they are more sad/depressed than earlier, and they are losing self-confidence. Some of them have mentioned about increased domestic violence and more work at home as their husband and other family members are at home. More than 60% women are afraid of giving birth in these uncertain COVID times as well as of getting infection during ANC visit to hospital. There is definitely a fear regarding uncertainty around COVID treatment and its mortality. All these issues which are related to mental wellbeing of pregnant women need to be addressed through proper counseling session for pregnant women as well as for their family members through online or offline method. This practice should be continued further even after COVID19 as these mental health issues are going to stay for a long.
In many settings, policies on social distancing may demand the restructuring of health care services to reduce face-to-face contact between doctors and patients, making diagnosis and support of mental health conditions more challenging. During this pandemic, many women are more vulnerable to intimate partner violence and associated adverse pregnancy outcomes and they are less able to seek support. Increased stress and anxiety during pregnancy up regulate inflammatory pathways and correlate strongly with neuropsychiatric disease for offspring.
Conclusion
The study showed that the majority of the pregnant women believed that they were at a high risk of infection with COVID-19, and many were concerned about possible health consequences, especially for their unborn child. Almost 90% of the pregnant women isolated at home most of the time. The majority were worried about possible consequences for antenatal care, but majorly they have attended a scheduled preventive consultation. The majority of the women preferred normal antenatal consultations in a normal clinical setting. Communication strategies must, however, strike a balance between inducing the necessary changes in daily living without inducing excessive feelings of dread. The perception of risk of infection and its consequences for their own health and the health of the unborn child was, however, also high. The COVID-19 pandemic has led to a rapid increase in the use of video consultations. This format may have important practical advantages, and, for some groups of patients, video-consultations might be advantageous. The pregnant women in our study are fine with an unchanged antenatal programme. Further research is required to assess the risks, costs, acceptability and potential benefits associated with alternative modes of delivery of antenatal care. Qualitative studies would be important in elucidating how the women value the personal face-to-face contact relative to the risk of infection. Self-isolation may have increased the women’s feeling of self-efficacy, i.e. their ability to control their health and risk. Such a mechanism can only be assessed by qualitative interview studies. Future studies should also address the effects of lockdown on the mental health of pregnant women.
The pandemic is already widening social inequalities, and the likely impending economic crisis will only exacerbate this, increasing inequality and pushing more women into poverty. Socioeconomic deprivation is a clear driver of maternal morbidity and mortality, and a positive gradient has been observed between deprivation indicators and a range of adverse maternal child health outcomes. We can expect the downstream effects of COVID-19 to be apparent for a number of years.
References
- WHO (2016) WHO recommendations on antenatal care for a positive pregnancy experience.
- Yang H, Wang C, Poon LC (2020) Novel coronavirus infection and pregnancy. Ultrasound in Obstetrics & Gynecology 55:435-437.
- UNICEF (2020) Antenatal care.
- (2019) Special Bulletin on Maternal Mortality in India 2015-17.
- (2015-2016) National Family Health Survey (NFHS-4) India Fact sheet.
- PMMVY | Ministry of Women & Child Development | GoI.
- Li Q, Guan X, Wu P, Wang X, Zhou L, et al. (2020) Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. The New England journal of medicine 382: 1199-1207.
- WHO Europe. (2020) WHO announces COVID-19 outbreak a pandemic.
- WHO (2020) WHO Director-General’s opening remarks at the media briefing on COVID-19.
- Wong SF, Kam M Chow, Tse N Leung,Sik T Lai,Wing W Yan, et al. (2004) Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. American journal of obstetrics and gynaecology 191: 292-297.
- Di Mascio D, Khalil A, Saccone G, Rizzo G, Buca D, et al. (2020) Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: a systematic review and meta-analysis. American journal of obstetrics & gynaecology MFM 2: 100107.
- Centers for Disease Control and Prevention (2021) Breastfeeding and Caring for Newborns.
- World Health Organization (2020) COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance.
- https://www.who.int/news/item/01-09-2020-new-research-helps-to-increase-understanding-of-the-impact-of-covid-19-for-pregnant-women-and-their-babies
- My safe motherhood Booklet for expecting mothers. Maternal Health Division Ministry of Health & Family Welfare, Government of India.
- Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, et al. (2020) Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ 1: 370.
- WHO (2016) WHO recommendations on antenatal care for a positive pregnancy experience.
Citation: Singh G, Gupta V, Tripathi N (2021) Continuity of Antenatal Care Services in Chhattisgarh during COVID19. J Community Med Public Health Care 8: 078.
Copyright: © 2021 Gajendra Singh, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

