
Cutaneous Nevi in Down Syndrome Patients: Prospective study
*Corresponding Author(s):
Nadia Abdalhafid ElsherifDepartment Of Dermatology And Venereology, Benghazi University, Benghazi, Libya
Tel:+218 913760697,
Email:elsherifnadia@yahoo.com
Abstract
Background: Down Syndrome (DS) has been described in association with various dermatoses,however, there is scanty information in the literature regarding the frequency of cutaneous nevi among Down syndrome patients.
The objective of the study: To define the frequency of different cutaneousnevi in DS patients, andto precise their different phenotypes.
Patients and methods: we prospectively examined 180 Down syndrome patients. All patients underwent full body skin examination noting the type, number, size, and distribution of different nevi.
Results: Different types of nevi were noted among Down syndrome patients; café au lait macules, melanocytic nevocellular nevi, and Mongolian spot were the most frequent ones. Juvenile elastoma, Becker’s nevus, nevus spilus, labial melanocytic macule, and capillary vascular malformation were also seen.
Conclusion: Various types of cutaneous nevi not previously described in Down syndrome, was observed in our patients such as Becker’s nevus, nevus spilus and Juvenile elastoma.
Keywords
Cutaneous, Down syndrome; Elastoma; Nevi
INTRODUCTION
Down syndrome first described in 1866,is the most common genetic cause of mental retardation in human population, and is caused by the presence of an extra copy of chromosome 21.[1]. Both males and females are equally affected, with a frequency of approximately one in 600-700 live births [2].
The major features of the syndrome are mental retardation, flattening of the back of the head, ocular, auricular and skeletal anomalies as well as other associated medical problems [1]. Moreover the patients are affected more often by chronic skin conditions and skin infections than the general populations [3]. A review of the literature reveals no informationregarding the relative frequency of cutaneous nevi among Down syndrome patients. The purpose of this study is to determine the prevalence of different cutaneous nevi among Down syndrome patients.
PATIENTS AND METHODS
Down syndrome patients
The present prospective study, comprised a total of 180 Libyan patients with Down syndrome attending both Genetic Clinic at Benghazi Pediatrics Hospital, and the Mental Rehabilitation School and Center in Benghazi city-Libya. A complete patients history was taken from their parents. All patients underwent a thorough dermatological examination in a good illuminated room. The diagnosis of most cutaneous nevi were based on their clinical features, and also on the histological examination of skin biopsy when simple morphological observation was not enough to accomplish the diagnosis. All attendants with the participating patients were asked to sign informed consent documents, and manuscript is according to declaration of Helsinki.
Skin biopsy
Incisional skin biopsies were taken from the back and abdomen of two patients with white firm papules under aseptic condition with local anaesthesia, the specimens were fixed in 10% buffered formalin, and conventional paraffin sections were prepared. The specimens were examined by light microscope, using the ordinary Hematoxylin and Eosin stain (H&E), and Verhoeff van Gieson stain for histopathological diagnosis.
Statistical methods
Data were analysed using Statistical Package for Social Sciences (SPPS) version 16.0. Descriptive statistics in the form of percentages, mean and standard deviation of different parameters was used.
RESULTS
One hundred eighty patients with Down syndromewere prospectively includedin the present study, 108 (60%) were males with age ranges from 1 week- 38 year, and 72 (40%) were females with age ranges from 1 week- 30 year, with a mean of age ± SD of 10.5 ± 7.9 years, with male to female ratio of 1.5:1.
Almost 61 (33.8%) of our patients had different types of cutaneous nevi, the frequency of each type are shown in Figure 1. Café au lait macules were seen in 11.7% of the patients; all them were above one year of age, with a male to female ratio of 1.6:1. The number of macules ranges from one to three in the individual patients, with average size of 1 cm (Figure 2A), none of the patients had axillary freckles or neurofibromas. Four patients had hypothyroidism and two had congenital heart diseases.
Acquired melanocytic nevocellular nevi (moles) were seen in 10% of the patients, of more than one year of age old, with a male to female ratio of 1.6:1. Most of the lesions were epidermal type. There were no significant associated diseases noted, except in one male child who is a known case of leukemia in whom labial melancyticmacule was found. Nevus spilus was seen in a thirteen year old female patient (Figure 2B). Becker's nevus was seen in two male patients, and presented as light brown hyperpigmented patch with geographic configurations on the anterior chest in 19 year old male patient, and on the shoulder of 12 year old male patient with alopecia total is (Figure 2C).
Salmon patch (capillary vascular malformation) was noted on the back of seven year old male Down syndrome patient (Figure 2D). Mongolian spot was noted in 7.8% of the patients, most of them in the 1-5 years age group, and females represented 64% of the cases, the lesion were blue patches on the lower back and buttocks of the patients (Figure 2E). There were no associated complains.
A symptomatic white- yellow, non follicular firm papules scattered in asymmetric clusters over the upper back and chest were seen in 1.7% of the patients, in the age group of 16- 20 years, with a male to female ratio of 2:1. None of the patients had a history of acne vulgaris, and there was no family history of a similar skin lesions. Clinically, elastoma, collagenoma and popular elastorrhexis were considered in the differential diagnosis (Figure 3). A skin biopsies were taken from a representative lesion on the back of two patients. The specimens were fixed in 10% formalin saline, sectioned and stained with Hematoxylin-eosin and Verhoeff van Gieson. H&E sections showed a focal epidermal acanthosis with thickened dermis containing normal-appearing connective tissue (Figure 4). whereas the Verhoeff van Gieson stain revealed an excess in elastic fibers throughout the reticular dermis, sparing the papillary dermis, with fairly normal collagen fibers, consistent with elastoma (Figure 5).
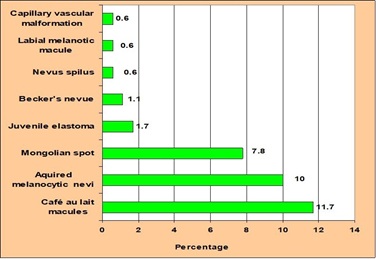 Figure 1: Prevalence of cutaneous nevi seen in Down syndrome patients.
Figure 1: Prevalence of cutaneous nevi seen in Down syndrome patients.
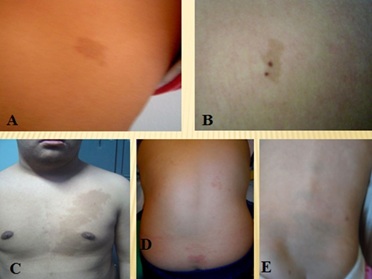 Figure 2: (A) Café au lait macules, (B) Nevus spilus, (C) Becker's nevus, (D) Capillary hemangioma, (E) Mongolian spots.
Figure 2: (A) Café au lait macules, (B) Nevus spilus, (C) Becker's nevus, (D) Capillary hemangioma, (E) Mongolian spots.
 Figure 3: Juvenile elastoma in the back of the patient.
Figure 3: Juvenile elastoma in the back of the patient.
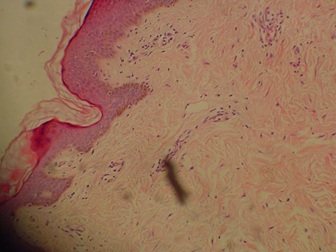 Figure 4: Section from popular lesion show thick dermis with normal-appearingconnective tissue. (H&E stain).
Figure 4: Section from popular lesion show thick dermis with normal-appearingconnective tissue. (H&E stain).
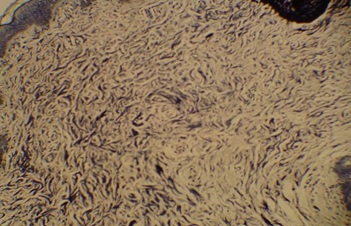 Figure 5: Dermis showing an excess in elastic fibers throughout the reticular dermis (Verhoeff van Gieson stain).
Figure 5: Dermis showing an excess in elastic fibers throughout the reticular dermis (Verhoeff van Gieson stain).
DISCUSSION
Nevi were seen frequently in our patients with Down syndrome. Café au lait macules and acquired melanocytic nevocellular nevi (moles) were the most frequent types seen in our patients.The prevalence of café au lait macules in newborns of general population is about 0.4%, and a higher prevalence is reported in older children as at least one café au lait macule larger than 0.5 cm was found in 24.2% of children, also it is more prevalent in black newborns than Caucasian ones, they are also more common in Arabic newborns [5].
Moreover, Café au lait macules have a definite association with neurofibromatosis type-1 and type-2, McCune-Albright syndrome, and Watson syndrome, while other syndromes had questionable association with the macules such as Bloom syndrome, Ataxia telangiectasia, and Tuberous sclerosis [5]. The high prevalence of café au lait macules in the general population, and its occurrence in many genetic syndromes make, therefore the association of Down syndrome with café au lait macules probably a coincidental one.
Acquired melanocytic nevocellular nevi (moles) were seen in 10% of our patients, more than one year old. One male child with leukemia had a labial melanocytic macule. The prevalence of melanocytic nevi varies with age, they are uncommon in infancy, and increases gradually during childhood and adolescence [6]. Nevus spilus was seen in a thirteen year old female patient. Nevus spilus or speckled and lentiginous nevus is a relatively rare entity [6].
Becker's nevus was noted in two male patients understudy. Becker's nevus presents in about 0.5% of young adults in the general population, with a higher incidence in males, suggesting that androgen sensitivity and stimulation may play a role in its pathogenesis [7].
Mongolian spots were noted in 7.8% of our patients, most of the patients were younger than 5 years of age, and females represent 64% of the cases, this was in accordance with another study which showed a prevalence of Mongolian spots in 6.4% of Down syndrome patients and most of cases were in the age group of 1-4 years.[4]Mongolian spot fades gradually and usually disappears by the age of 4 years, and its persistence beyond the first decade of life is uncommon, although it is reported to occur among 4% of Japanese adults [8].
Mongolian spots have been reported in association with common structural anomalies such as cleft lip, and supernumerary digits, however, recognition of extensive Mongolian spots is of particular importance in early diagnosis of Hurler and Hunter syndrome [8]. The occurrence of Mongolian spots among our Down syndrome patients may either be just a coincidental observation or a true association.
Salmon patch (capillary vascular malformation) was noted in only one patient. Down syndrome has a reduced riskof vascular anomalies compared with the general population, this protective effect has been attributedto an increased gene dosage from an additional copy of chromosome 21, which causes elevated expression of antiangiogenic proteins [9].
In the present study, the diagnosis of elastoma, also known as nevus elasticus or juvenile elastoma was confirmed by histological examination of biopsy specimens from two of three patients with Down syndrome presented with asymptomatic white-yellow, non follicular firm papules scattered over the upper back and the chest. There was no family history of similar skin lesions. All the three patients were in the age group of 16- 20 years, with a male to female ratio of 2:1.
Connective tissue naevi are circumscribed hamartomatous malformations of the dermal extracellular matrix, including collagen, elastic fibres or glycosaminoglycans. Isolated (sporadic) and familial forms of elastoma have been reported. The familial form is inherited as an autosomal dominant trait, and in association with osteopoikilosis, it is known as Buschke-Ollendorff syndrome [10]. However, sporadic occurrence without any associated extracutaneous manifestations has also been reported [10]. The occurance of different types of connective tissue naevi in patients with Down syndrome have been reported [11,12]. However, to our knowledge, this is the first report of juvenile elastoma in DS patients. The pathogenesis of elastoma in Down syndrome is still unclear. Since elastosis perforans serpiginosa is a well known complication of Down syndrome, therefore, various connective tissue disorders including elastoma, collagenoma, and others may also be seen in those individuals with Down syndrome [11]. Absence of a family history of similar skin lesions among our patients may exclude the possibility of Buschke-Ollendorff syndrome, but may strongly represent a formefruste of the Buschke-Ollendorff syndrome [10].
In conclusion, we recommend very carefulexamination and regular long-term follow up for children with Down syndrome who present with cutaneous nevi.
REFERENCES
- Chisholm KM (2018) Down Syndrome. Atlas Genet CytogenetOncol Haematol 22: 182-184.
- Sherman SL, Allen EG, Bean LH, Freeman SB (2007) Epidemiology of Down syndrome. Mental retardation and developmental disabilities research reviews 3: 221-227.
- Madan V, William J, Lear JT (2006) Dermatological manifestations of Down's syndrome. Clin Exp Dermatol 31: 623-629.
- Schepis C, Barone C, Siragusa M, Pettinato R, Romano C (2002) An updated survey on skin conditions in Down syndrome. Dermatology 205: 234-238.
- Shah KN (2010) The diagnostic and clinical significance of café-au-lait macules. Pediatr Clin North Am 57: 1131-1153.
- Mackie RM (2004) Disorders of the cutaneous melanocyte. In: Burns T, Breathnach SM, Cox N, Griffiths C (eds). Rook’s Textbook of Dermatology. (7th edn) Oxford: Black Well Science, New Jersey, USA. 38: 4-38.
- Atherton DJ, Moss C (2004) Naevi and other developmental defects. In: Burns T, Breathnach SM, Cox N, Griffiths C (eds). Rook’s Textbook of Dermatology, (7th edn). Oxford: Black Well Science: 15: 17-18.
- Inamadar AC, Palit A (2007) Persistent, aberrant Mongolian spots in Sjögren-Larsson syndrome. Pediatr Dermatol 24: 98-99.
- Greene AK, Kim S, Rogers GF, Fishman SJ, Olsen BR, et al. (2008) Risk of vascular anomalies with Down syndrome. Pediatrics 121: 135-140.
- Foo CC, Kumarasinghe SPW (2005) Juvenile elastoma: A forme fruste of the Buschke-Ollendorff syndrome? Australas J Dermatol 46: 250-252.
- Togawa Y, Nohira G, Shinkai H (2003) Collagenoma in Down syndrome. Br J Dermatol 148: 596-597.
- Sais G, Jucglà A, Moreno A, Peyrí J (1995) Milia-like idiopathic calcinosis cutis and multiple connective tissue nevi in a patient with Down syndrome. J Am Acad Dermatol 32: 129-130.
Citation: Elsherif NA, Elsherif AI (2020) Cutaneous Nevi in Down Syndrome Patients: Prospective study. J Clin Dermatol Ther 6: 057.
Copyright: © 2020 Nadia Abdalhafid Elsherif, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

