
Cutaneous Pseudolymphoma of B and T Cells: A Case Report
*Corresponding Author(s):
Thaís Andrade De OliveiraDepartment Of Dermatology, Faculdade De Medicina De Jundiaí, Brazil
Tel:+55 11 993734159,
Email:thaisandrade8@gmail.com
Abstract
Cutaneous pseudolymphomasre present a benign reactive polyclonall ymphoproliferative process that simulates clinically and histologically cutaneous lymphomas. The objective of this study was to report the case of cutaneous pseudolymphoma to present its differential diagnosis with cutaneously mphomas, and other adnexal tumors. A 14-year-old male patientsought medical care for a historyof a nodule in the supralabial region for 3 months. Physical examination showed an erythematous nodule of 15 mm betweenthe supralabial region and the right nasal vestibule, without associated lymph node enlargement. The anatomo pathological showed a dense lymphohistiocytic in filtrate and intense vascular proliferation, with suppurative foci. The immunohistochemistry favored the diagnosis of cutaneous pseudolymphoma. The differential diagnosis of lymphomas and pseudolymphomasis difficult, both of which manifest as solitary nodules, papules or plaques resulting from lymphocytic infiltration and for this are indicated an atomopathological and immunohistochemical evaluation. The treatmentencompassessurgicalexcision, topical corticosteroid and intralesional cryo therapy, and in many cases there is spontaneous regression.
INTRODUCTION
CASE REPORT
At dermatological examination, the patient had an erythematous nodule off ifteen millimeters in diameter between the supralabial region and the right nasal vestibule, with a small central crust (Figure 1). In addition, it had multiple open and closed comedones, papules and pustules, characterizing a grade II acne. He did not present lymph node enlargement.

In this initial evaluation, the main clinical suspicion of a pyogenic granuloma was raised, and local cryotherapy followed by cortico idinfiltration were instituted as treatment. After seven days, there was no significant improvement, and being pseudo lymphoma and cutaneous lymphomas likely to be differential diagnoses, it was decided to perform biopsy of the lesion.
After local anesthesia, enucleation of the lesion was performed through a central spindle preserving the borders, with posterior suture for approach andthe material sent for analysis (Figure 2). He also started treatment for acne with soap and sunscreen, as well as adapalene and topical benzoyl peroxide.

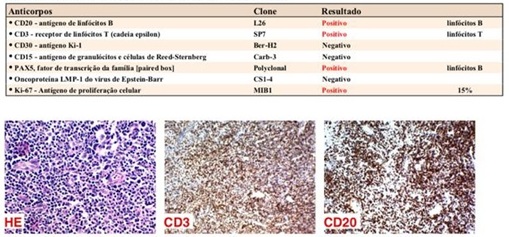
The pathological anatomy showed a lesion with dense lymphohistiocytic infiltrate and intense vascular proliferation with suppurative foci. Immunohistochemistry was positive for CD20, CD3, PAX-5 and ki-67 (Figure 3), thus containing mixed T and B lymphoid infiltrate, favoring the diagnosis of cutaneousps eudolymphoma.
After the surgical procedure performed for biopsy, the patient returned for evaluation with totally regression of the initial lesion (Figure 4), in addition to the improvement of the acne, without presenting signs of recurrence of the lesion during follow-up.
 Figure 4: Totally regression of the initial lesion after procedures.
Figure 4: Totally regression of the initial lesion after procedures.DISCUSSION
The pathogenesis of CPL is still studied and it is believed that there is participation of the Skin Associated Lymphoid Tissue (SALT) and its proliferation by antigenic stimulation. This theory corroborates the progression of CPL to lymphoma due to permanent antigenic exposure, as occurs with gastric lymphomas [5,6].
Clinically, it may present as a single nodule, as observed in the case described, ormultiple, papules, infiltrated plaques, persistent erythema or exfoliative erythroderma, and it is impossible to define the diagnosis only by clinical examination of the lesions. In view of the CPL hypothesis, the lesion should be biopsied [4].
Histological analysisis of paramount importance in the definition of the diagnosis. There is a lymphocytic-follicular proliferation of T cells, B or the mixture of the two with macrophages and dendritic cells [6]. The pattern of infiltration maybe nodular or epidermo tropic, and cell size is variable. Immunohistochemistry is imperative in distinguishing the infiltrate and its classification [4].
Therefore, the diagnosis of CPL is based on clinical history, physicalexamination, and adequate an atomopathological and immunohistochemical study. The search for causal agents, serological and contact tests are auxiliary [3].
As for the clinical course, it is usually variable. Some lesions regress after the biopsy, while others may persist for months to years. There may be recurrence in cases of new contact with the causative agente. Rareprogressionof CPL to cutaneous lymphoma can occur, butthe cause is not well understood. Clinical signs of alertness involve the presence of multiple lesions and lymphadenopathy [3].
Treatment should be considered conservative, sincemany cases regress spontaneously. Single lesions can be treated with surgical excision, topical cortico steroid and intralesional, cryotherapy. Disseminated cases can be treated with systemic cortico steroids, Interferon alfa, Hydroxychloroquine and even radiotherapy [2,4]. Removal of the causative agent, if identified, should be performed. In the case reported, the lesion regressed after partial surgical excision (biopsy) and acne treatment was instituted, aiming to control the possible triggering factor.
REFERENCES
- Mitteldorf C, Kempf W (2017) Cutaneous Pseudolymphoma. Surgical Pathology Clinics 10l: 455-476.
- Romero-Pérez D, Martínez M, Encabo-Durán B (2016) Pseudolinfomas cutáneos. Actas Dermo Sifil 107: 640-651.
- Miguel D, Peckruhn M, Elsner P (2018) Treatment of Cutaneous Pseudolymphoma: A Systematic Review. Acta Derm Venereol 98: 310-317.
- Zhou LL, Mistry N (2018) Cutaneous lymphoid hyperplasia (pseudolymphoma). CMAJ 190: 398.
- Bergman R (2010) Pseudolymphoma and cutaneous lymphoma: Facts and controversies. Clin Dermatol 28: 568-574.
- Terada T (2013) Cutaneous pseudolymphoma: A case report with an immunohistochemical study. Int J Clin Exp Pathol 6: 966-972.
Citation: de Oliveira TA, de Oliveira CH, Flora TB, Pinto CAL, Cunha PR, et al. (2019) Cutaneous Pseudolymphoma of B And T Cells: A Case Report. J Clin Dermatol Ther 5: 038.
Copyright: © 2019 Paulo Rowilson Cunha, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

