
Delays in the Placement of Nasogastric Tube: Where are they?
*Corresponding Author(s):
David G SmithardConsultant In Elderly And Stroke Medicine, Queen Elizabeth Hospital, Lewisham And Greenwich NHS Trust, London, United Kingdom
Tel:+44 02088366000,
Email:david.smithard@nhs.net; dgsstroke@hotmail.co.uk
Abstract
Dysphagia following stroke is common and not too infrequently requires a nasogastric tube to be placed. Often there are delays in the pathway between the timing of a decision to place a NGT and it being available and safe to use. This study has examined the time taken between each phase of the pathway and the time taken over all.150 stroke patients were recruited from 5 English Hospitals. Majority were severe strokes (NIHSS > 15, mRS > 4). From the time of decision making to NGT readiness was 467.15 minutes. There was no significant difference in timings between hospitals. Stroke severity was not a marker for the length of time taken to pass the NGT. It is likely that the need for radiology played a significant role, but would not count for all the differences.The study has demonstrated that some patients wait a long time for a NGT to be ready for use after the clinical decision has been made regarding its placement.
INTRODUCTION
METHODOLOGY
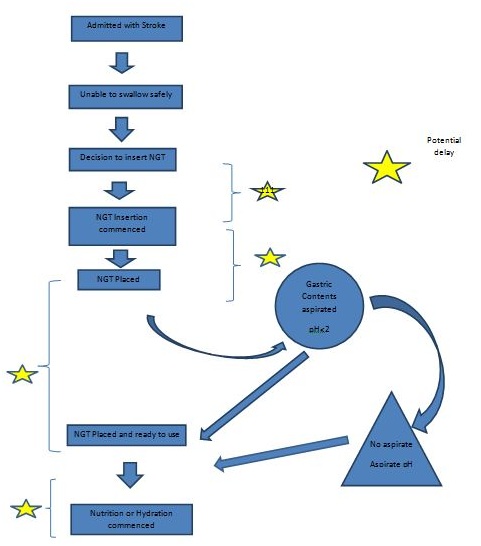 Figure 1: Steps to placement of NGT and places of potential delay.
Figure 1: Steps to placement of NGT and places of potential delay.RESULTS
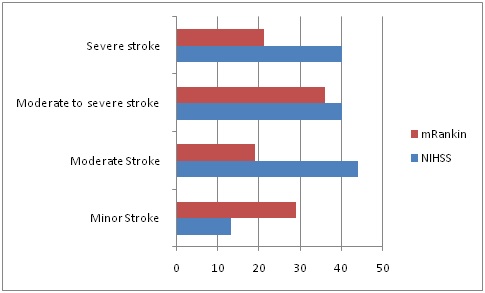 Figure 2: Stroke severity (National Institute of Health Stroke Score (NIHSS) and modified Rankin Scale (mRS)).
Figure 2: Stroke severity (National Institute of Health Stroke Score (NIHSS) and modified Rankin Scale (mRS)).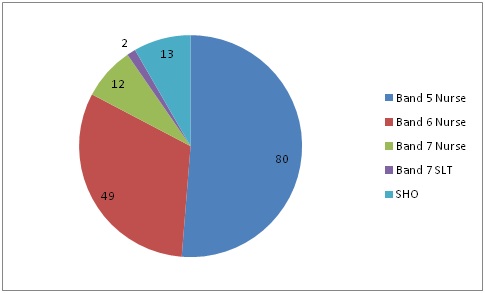 Figure 3: Staff and Seniority of staff placing NGT.
Figure 3: Staff and Seniority of staff placing NGT.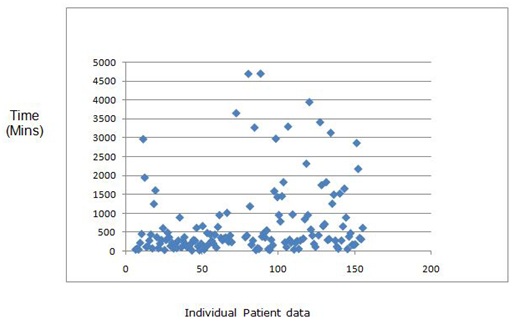 Figure 4: Time from decision taken as to the requirement for NGT to time ready to use (Individual patient data).
Figure 4: Time from decision taken as to the requirement for NGT to time ready to use (Individual patient data).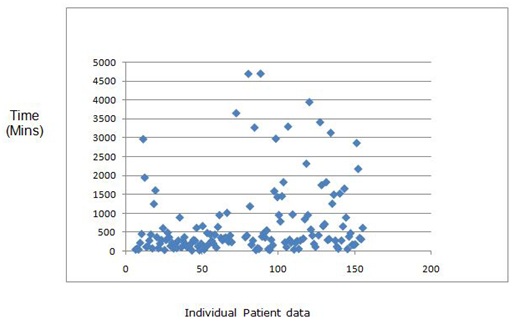 Figure 5: Time from NGT being ready for use to feeding commencing (Individual patient data).
Figure 5: Time from NGT being ready for use to feeding commencing (Individual patient data).|
Hospital |
N |
Number (%) CXR undertaken |
Mean time (Mins) |
Median time (Mins) |
Range (Mins) |
|
1 |
49 |
31(63) |
748 |
360 |
61 - 3948 |
|
2 |
50 |
14(28) |
431.9 |
283 |
23 - 2968 |
|
4 |
14 |
1(7.1) |
1300.4 |
975 |
50 - 3655 |
|
5 |
32 |
23 (71.9) |
962.9 |
320 |
35 - 4700 |
|
6 |
26 |
5(19.2) |
1036.4 |
451 |
210 - 3416 |
Table 1: Number Chest X-Rays (CXR) undertaken and time taken for NGT to be ready for use from time of decision per Hospital.
38/150 of people recruited only required one attempt to pass an NGT. There were 42 (28%) cases of presumed aspiration pneumonia following the passing of a NGT.
DISCUSSION
CONCLUSION
The use of NGTs in stroke units and acute general hospitals is common. This study has shown that there are, in many instances, significant delays in the NGT placement pathway. Delays occurred between each phase of the pathway (Figure 1). In many cases the delays may not have resulted in a detrimental effect to the patient, however feeding was delayed and a route for the delivery of medication was delayed. Clinicians need to investigate ways to improve the pathway rather than accepting the present status quo.
ACKNOWLEDGEMENT
Dean Waugh, Leeds Teaching Hospitals NHS Trust; East Kent Hospitals University NHS Foundation Trust, David Hargroves, Linda Cowie; Colchester Hospital NHS Trust, Alison Wright, Ramachandra Sivakumar King's College Hospital NHS Foundation Trust, James Teo, Laszlo Szithra. Southport and Ormskirk Hospitals NHS Trust, Lucy Enright.
REFERENCES
- Martino R, Foley N, Bhogal S, Diamant N, Speechley M, et al. (2005) Dysphagia After stroke. Stroke 36: 2756-2763.
- Smithard DG, O'Neill PA, England RE, Park CL, Wyatt R, Martin DF, et al. (1997) The natural history of dysphagia following stroke. Dysphagia 12: 188-193.
- Hussain A, Woolfrey S, Massey J, Geddes A, Cox J (1996) Percutaneous endoscopic gastrostomy. Postgrad Med J 72: 581-585.
- Mann G, Hankey GJ, Cameron D (1999) Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke 30: 744-748.
- Royal College of Physicians (2016) National clinical guideline for stroke (5thedn). National Clinical Guideline for Stroke, London, UK.
- National Institute for Health and Care Excellence (2010) Stroke in Adults. Quality Standard (QS2). National Institute for Health and Care Excellence, London, UK.
- Royal College of Physicians of London (2002) Nutrition and patients a doctor's responsibility/report of a working party of the Royal College of Physicians. Royal College of Physicians of London, London, UK.
- Dennis M, Lewis S, Warlow C, FOOD Trial Collaboration (2005) Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): a multicentre randomised controlled trial. Lancet 365: 764-772.
- Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, et al. (1980) Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ 58: 113-130.
- Brott T, Adams HP Jr, Olinger CP, Marler JR, Barsan WG, et al. (1989) Measurements of acute cerebral infarction: a clinical examination scale. Stroke 20: 864-870.
- Rankin J (1957) Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J 2: 200-215.
- Sparks DA, Chase DM, Coughlin LM, Perry E (2011) Pulmonary Complications of 9931 Narrow-Bore Nasoenteric Tubes During Blind Placement: A Critical Review. JPEN J Parenter Enteral Nutr 35: 625-629.
- Sorokin R, Gottlieb JE (2006) Enhancing patient safety during feeding-tube insertion: a review of more than 2000 insertions. JPEN J Parenter Enteral Nutr 30: 440-445.
- Rao M, Kallam R, Arsalani-Zadeh R, Gatt M, MacFie J (2009) Placing of feeding tubes by the bedside using an electromagnetic sensing device. Br J Intensiv Care Summer 54-59.
- Dávalos A, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, et al. (1996) Effect of malnutrition after acute stroke on clinical outcome. Stroke 27: 1028-1032.
- Taylor S, Allan K, McWilliam H, Manara A, Brown J, et al. (2014) Confirming nasogastric tube position with electromagnetic tracking versus pH or X-ray and tube radio-opacity. Br J Nurs 23: 352-358.
- Kalra L, Hodsoll J, Irshad S, Smithard D, Manawadu D, et al. (2016) Association between nasogastric tubes, pneumonia, and clinical outcomes in acute stroke patients. Neurology 87: 1352-1359.
- Dziewas R, Warnecke T, Hamacher C, Oelenberg S, Teismann I, et al. (2008) Do nasogastric tubes worsen dysphagia in patients with acute stroke? BMC Neurol 8: 28.
- National Patient Safety Agency (NPSA) (2011) Patient Safety Alert NPSA/2011/PSA002: Reducing the harm caused by misplaced nasogastric feeding tubes in adults, children and infants. National Patient Safety Agency, England, UK.
Citation: Smithard DG, Irizar H (2018) Delays in the Placement of Nasogastric Tube: Where are they? J Gastroenterol Hepatology Res 3: 015.
Copyright: © 2018 David G Smithard, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

