
Journal of Clinical Dermatology & Therapy Category: Clinical
Type: Case Report
Demodex Folliculitis of the Scalp: Case Report
*Corresponding Author(s):
Soares VCHospital De Clinicas Universidade Federal Do Parana, Brazil
Tel:+55 4133601800,
Email:vanesoares@yahoo.com.br
Received Date: May 30, 2019
Accepted Date: Jun 18, 2019
Published Date: Jun 25, 2019
Abstract
Demodex is a commensal mite found in the pilosebaceousunits. Demodicosis in scalp is uncommon and only few cases were reported on the literature. We described a young caucasian male with burning, scaling and pustules on the scalp. The scalp biopsy showed granulomatous reaction and presence of Demodex mites in follicular canals. The diagnose of demodex folliculitis of the scalp was made and a good response was achieved after topical metronidazole treatment.
Keywords
Demodex; Demodicosis; Folliculitis; Metronidazole; Rosacea; Rosacea-like; Scalp; Therapy
INTRODUCTION
Demodex is a commensal mite found in the pilosebaceous units. The three mainly demodicosis clinical forms described in facial skin are: pityriasisfolliculorumwhich presents facial erythema, burning, scales and follicular plugs; rosacea-like demodicosischaracterized by scales, erythema and papulopustules very similar with rosacea and demodicosis gravis also called granulomatous rosacea-like [1].
Demodex can also occur associate with others skin conditions such as perioral dermatitis, rosacea and seborrehoeic dermatitis, called secondary demodicosis by some authors [2]. The clinical diagnose of demodicosis can be difficult due its clinical signs are common with other skin disorders.
Demodex can also occur associate with others skin conditions such as perioral dermatitis, rosacea and seborrehoeic dermatitis, called secondary demodicosis by some authors [2]. The clinical diagnose of demodicosis can be difficult due its clinical signs are common with other skin disorders.
CASE REPORT
A 19-year-old caucasian male presented burning sensation, scaling on the center facial and scalp for the last four months. He had been treated before by another dermatologist with anti-seborrheic facial soap and corticosteroids shampoo without success. He had a medical record of atopic dermatitis, allergic rhinitis and penicillin allergy.
On clinical examination, he had some pustules on the nose and erythematous plaques with fatty scaling on glabella, nasolabial sulcus and chin. The dermoscopy on the vertex scalp revealed scaling, follicular pustules, crusts, perifollicular and interfollicular erythema (Figure1).There was no ocular symptoms. The diagnosis of facial and scalp seborrheic dermatitis was made. Doxycycline 100mg daily, ketoconazole 2% cream, ketoconazole 2% shampoo and clobetasol propionate 0.05% scalp solution was prescribed and there has been improvement on the facial and scalp lesions. After 2 weeks without treatment, the scalp lesions relapsed. Dermoscopy presented perifollicular erythema,pustules and crusts on vertex scalp. A bacterial folliculitis was suspected, It was prescribed oral sulfamethoxazole plus trimethoprim during four weeks without success.
On clinical examination, he had some pustules on the nose and erythematous plaques with fatty scaling on glabella, nasolabial sulcus and chin. The dermoscopy on the vertex scalp revealed scaling, follicular pustules, crusts, perifollicular and interfollicular erythema (Figure1).There was no ocular symptoms. The diagnosis of facial and scalp seborrheic dermatitis was made. Doxycycline 100mg daily, ketoconazole 2% cream, ketoconazole 2% shampoo and clobetasol propionate 0.05% scalp solution was prescribed and there has been improvement on the facial and scalp lesions. After 2 weeks without treatment, the scalp lesions relapsed. Dermoscopy presented perifollicular erythema,pustules and crusts on vertex scalp. A bacterial folliculitis was suspected, It was prescribed oral sulfamethoxazole plus trimethoprim during four weeks without success.

Figure 1: The dermoscopy on the vertex scalp revealed follicular pustules, crusts, perifollicular and interfollicular erythema.
In order to elucidate the diagnosis, a scalp biopsy was performed. The histopathological examination revealed superficial folicullitis, interfolicular granulomatous reaction on dermis (Figure 2) and presence of Demodex in some hair follicles (Figure 3). No bacterial colonies or fungal were found. Firstly me consider a scalp rosacea diagnose, but the absence of clinical signs for facial rosacea led us to the diagnosis of scalp demodicidosisfollicullites. Tetracycline 500mg and metronidazole solution on scalp was prescribed for four weeks. After one year of follow up, the patient remained asymptomatic.
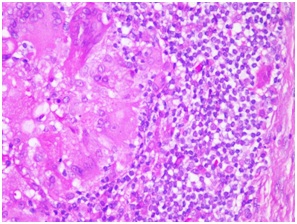 Figure 2: Histopathological scalp exam showed granulomatous reaction on dermis.
Figure 2: Histopathological scalp exam showed granulomatous reaction on dermis.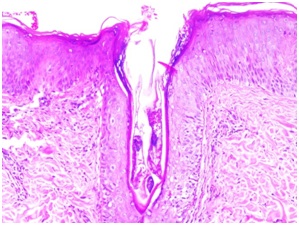 Figure 3: Presenceof Demodex inside the follicular canal.
Figure 3: Presenceof Demodex inside the follicular canal.DISCUSSION
A young man has been described, whose scalp signs and symptoms and histopathological findings were compatible with demodex folliculitis of the scalp. Previous case reports has involved bald scalp, within mid age men who presented facial more severe lesions [3]. Oberholzer et al., in 2009, described two patients complaining about red scalp with itching or burning sensation, erythema, papules and pustules on hairy scalp. There was no evidence of facial rosacea and the scalp biopsy showed absence of Demodexand presence of granuloma formation on dermis consistent with rosacea. However, the diagnose of rosacea-like dermatosis was given, whereas at that moment, no case of rosacea on hairy scalp has been published [4].
Demodex is commonly found on the face but unusual on the scalp [5]. Only few case reports of demodicosis of the scalp has been described [7-9]. Histopathological exam was performed on two cases demonstrated folliculitis, perifolliculitis and intrafollicular Demodex mites [7,8]. A retrospective study reviewedscalp biopsies of 333 patients with different diseases. Demodex mites were foundin 17 cases. Four of them, showed similar clinicalfindings, among them, hair loss, erythema, scales and pustules. Histopathology showed 2 or more Demodex mites, mono-nuclear cell infiltrates and granulomas were present in 2 cases [10].
The diagnose of demodicosisis suspected when suggestive clinical signs and symptons are present, when the mites are found by Standardized Skin Surface Biopsy (SSSB) [11]. The presence of more than five mites per follicle or per cm2 is consider positive for demodicosis [12].
In our case, the diagnose was defined due yourhistopathological findings, absence of facial rosaceaand response after topical metronidazole treatment.
Demodex is commonly found on the face but unusual on the scalp [5]. Only few case reports of demodicosis of the scalp has been described [7-9]. Histopathological exam was performed on two cases demonstrated folliculitis, perifolliculitis and intrafollicular Demodex mites [7,8]. A retrospective study reviewedscalp biopsies of 333 patients with different diseases. Demodex mites were foundin 17 cases. Four of them, showed similar clinicalfindings, among them, hair loss, erythema, scales and pustules. Histopathology showed 2 or more Demodex mites, mono-nuclear cell infiltrates and granulomas were present in 2 cases [10].
The diagnose of demodicosisis suspected when suggestive clinical signs and symptons are present, when the mites are found by Standardized Skin Surface Biopsy (SSSB) [11]. The presence of more than five mites per follicle or per cm2 is consider positive for demodicosis [12].
In our case, the diagnose was defined due yourhistopathological findings, absence of facial rosaceaand response after topical metronidazole treatment.
REFERENCES
- Baima B, Sticherling M (2002) Demodicidosis revisited. Acta Dermato-Venereologica 82: 3-6.
- Chen W, Plewig G (2014) Human demodicosis: Revisit and a proposed classification. Br J Dermatol 4170: 1219-1225.
- Wong CS, Kirby B (2004) Demodicidosis in scalp rosacea.Clin Exp Dermatol 29: 318-319.
- Oberholzer PA, Nobbe S, Kolm I, Kerl K, Kamarachev J (2009) Red scalp disease-A rosacea-Like Dermatosis of the Scalp? Successful therapy with oral tetracycline. Dermatology 219: 179-181.
- Miskjian HG (1951) Demodicidosis (Demodex infestation of the scalp). AMA Arch Derm Syphilol 63: 282-283.
- Gilaberte Y, Frias MP, Rezusta A, Vera-Alvarez J (2009) Photodynamic therapywith methyl aminolevulinate for resistant scalp folliculitis secondary to Demodex infestation. J Eur Acad Dermatol Venereol 23: 718-719.
- Fernandez-Flores A, Alija A (2009) Scalp folliculitis with Demodex: innocentobserver or pathogen? Braz J Infect Dis 13: 81-82.
- Sanfilippo AM, English JC 3rd (2005) Resistant scalp folliculitis secondary to Demodex Infestation.Cutis 76: 321-324.
- García-Vargas A, Mayorga-Rodríguez JA, Sandoval-Tress C (2007) Scalp demodicidosis mimicking favus in a 6-year-old boy.J Am Acad Dermatol 57: 19-21.
- Helou W, Avitan-Hersh E, Bergman R (2016) Demodex Folliculitis of the Scalp: Clinicopathological Study of an Uncommon Entity. Am J Dermatopathol 38: 658-663.
- Forton FMN, De Maertelaer V (2019) Rosacea and Demodicosis: Little-known Diagnostic Signs and Symptoms.Acta Derm Venereol 99: 47-52.
- Hsu CK, Hsu MM, Lee JY (2009) Demodicosis: A clinicopathological study. J Am Acad Dermatol. 60: 453-462.
Citation: Soares VC, Mulinari-Brenner FA, Werner B (2019) Demodex Folliculitis of the Scalp: Case Report. J Clin Dermatol Ther 5: 032.
Copyright: © 2019 Soares VC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

Journal Highlights
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!
