
Depression and Its Relation with HIV Risk and Social Well-Being among the Brothel-Based Female Sex Workers in Kolkata, India
*Corresponding Author(s):
Smarajit JanaDurbar Mahila Samanwaya Committee, Sonagachi Research & Training Institute, Kolkata, West Bengal, India
Tel:+91 8336071001,
Email:smarajitjana@gmail.com
Abstract
The overall objective of the research study, called DRISHTI, is to assess the effectiveness of the use of community based caregivers to address mental health related problems among the sex workers. As designed the first phase of the study looked into the prevalence of depression among the FSWs, and to find out any association between socio demographic and sex related factors with depression. The other objective of the study is to find out the relative contribution of depression in inducing unsafe sex practices among the FSWs. The research findings has shown high rate of depression (38.3%) in varying degrees (mild, moderate and severe) among the participants (total 400). No socio-demographic factors were found to be associated with depression. Whereas sex workers who are depressed are less likely to use condoms, having high prevalence of STIs and poor treatment seeking behaviour in comparison to those are not depressed. Study findings also suggest that depressed FSWs are not putting importance to good financial planning for future and more likely to engage in conflicts with other community members.
Keywords
INTRODUCTION
Mental health is increasingly being recognized as a major global contributor to poor health and well-being. The burden of illness resulting from psychiatric and behavioral disorders is enormous in nature. Yet it remains grossly under-presented in public health discourse. It is estimated that sufferings from psychiatric disorders accounted for 5 of the10 leading causes of disability as measured by years lived with disability [1].
The overall DALYs (Disability Adjusted Life years) burden for neuropsychiatric disorders are projected to increase by 15% more by the year 2020 [2,3]. In the recent past the significance of mental health and its social impact has drawn greater attention at UN Policy making bodies. The agenda for Sustainable Development Goal [SDG] has included mental health and substance use as an important development issue for which specific indicators has been identified under health and well-being Goal 3 of SDG [4]. In India, the respective ministry has developed national policy of mental health, and is committed to implement a national level program to integrate mental health with the primary health care services, the largest such effort in a developing country [5]. It is estimated that 1% to 2% (around 10 to 20 million) of the Indian population is suffering from major mental disorders, and around 5% (50 million) of Indian citizen suffer from minor mental health disorders [6].
Poor mental health plays a significant role in influencing high-risk behavior among individuals [7]. Studies suggest that depressed individuals can be more prone to engage in unprotected sex, substance abuse and other unsafe behavior [8]. Being in the sex work women do suffer from occupational hazards which includes varied kinds of stress and injuries including sexually transmitted infections. It is more so important as FSWs are considered as an important high-risk group in HIV transmission dynamics [9,10].
FSWs have been found to be at higher risk for mental health disorders, including depression. Consequently, FSWs suffering from mental health disorders might be at an increased risk of engaging in unsafe behavior such as unprotected sex [11] or substance use. They show little interest and less aspiration in planning future-oriented activities such as financial planning [12]. Importantly, FSWs may thus be at higher risk in accusing HIV infection as well as would face higher degree of challenges in accessing care or support services due to their stigmatized and marginalized status. Moreover, FSWs are the commonest victim of violence, abuse and social discriminatory practices. All these underlying factors act as barrier in accessing treatment and other support services [13]. Therefore depression may have a far-fetched implication in sex workers life and could adversely affect the well-being of FSWs [14]. Studies in the USA have identified high level of mental illnesses such as depression among sex workers [15]. Scholars have noted that depression is significantly associated with the high risk of becoming HIV infected [16,17].
Sex workers in India are especially at higher risk of suffering from depression due to the constellation of cultural challenges that they face [18]. The situation is exacerbated by the stigma attached to mental health including social isolation which is often confronted by individuals suffering from depression [19-21]. However, there is very little scholarship on depression with specific focus to sex workers in India, and its association with the elevated levels of HIV risk. Moreover, there is no specific strategy and intent to initiate mental health interventions targeting sex workers to address depression including its association with HIV risk taking behavior. Given the high prevalence of HIV-related risk behavior among those with depression, and the fact that sex work is one of the primary engine driving the spread of HIV in India, the dearth of mental health interventions for sex workers can severely undermine outcome of HIV initiative in the country. The present research seeks to address these gaps by designing and testing DRISHTI; ‘Depression reduction Implemented by Sex workers to stop HIV Transmission Intervention’ (DRISHTI, or “vision” in Bengali) aimed at managing depression to improve attitude, motivation and self efficacy with major focus to sexual practices. DRISTI has evolved a strategy to engage trained community members who could be playing an important role as mental health counselor to handle cases of depression. The community counselor would be inducted in the subsequent phases of the ongoing study.
Scholars have noted that individuals with mental illness are at greater risk of HIV infection [22]. Studies have observed high rates of infection among those newly admitted to inpatient psychiatric facilities [23]. Psychiatric patients tend to be less well informed about STIs [24], poorly motivated to adopt risk reduction strategies [25,26], and lacking the interpersonal and social skill needed to negotiate safer sex [27]. Kalichman and Weinhardt [28] noted that the negative impact of depression on HIV risk behavior has largely been ignored. A meta-analysis on the modifying effects of depression on HIV interventions found that individuals are less likely to engage in HIV risk taking behavior if they are not depressed [29]. Few studies have examined the influence of depression on HIV risk in India. HIV prevalence is observed to range between 2% to 3% among people with depression, compared to 0.7% prevalence in the general population in India [30]. Sahay et al., [31] found that Indians who are engaged in high-risk behavior are almost 3 times more likely to be depressed and anxious. Similarly, scholars have found that stigma, violence, conflict with clients and poverty significantly compromise mental health among sex workers in Hong Kong [32], Great Britain [33], China [34] and Canada [35]. A recent study in India observed that almost 35% of a sample of sex workers reported suicidal ideation, and 19% of them attempted suicide at least in one occasion in the past [36].
This formative research has been undertaken in the first phase of this study to find out the relative contribution of depression behind unsafe sex practices among sex workers. The research is duly implemented by Durbar Mahila Samanwaya Committee (DMSC) with the support of the ICMR (Indian Council of Medical Research) and the National Institute of Health (NIH), based on an objective to make an assessment of depression among FSWs and its potential impact in the Sonagachi red light district in Kolkata, India as a part of Indo-USA collaboration. Unfortunately, mental health care is often inaccessible for approximately one third of the population living below the poverty line as well as those who are otherwise socially marginalized [36]. The overall objective of the study (DRISHTI) is to test a strategy to deal with mental health related issues through involving community members as the caregivers. For the ongoing study field workers who have been selected from among the community members would be retained and trained further to play their role as caregivers. As planned the second phase of the study would throw light on how to develop a viable model to handle mental illnesses in resource poor settings, with special focus to sex workers’ community.
MATERIALS AND METHODS
Setting
DMSC is directly involved in improving the quality of life of around three hundred thousand sex workers including their family members across the state of West Bengal who are otherwise socially, economically and politically marginalized and ostracized. The said sex workers collective deliver a comprehensive package of services which includes health, education, financial security in addition to steering Anti trafficking program of their own. Under health interventions; services delivered by DMSC includes primarily health care, sexual health in addition to reproductive health care services. The said sex workers collective also support career building opportunities as well as creating space for cultural expression for sex workers and their children [37]. Side by side the sex workers collective has undertaken operation and intervention research to comprehend issues and challenges with an objective to improve quality of health and other development program. However DMSC is yet to initiate any intervention program centering Mental Health among the sex workers. Before initiating such intervention it was a felt necessity to assess quantum of burden and to assess the state of mental health among the sex workers community. In line with the objective, the largest red light district namely Sonagachi having more than 10,000 sex workers, based in city Kolkata, the capital of the state of West-Bengal was chosen to conduct this study.
Sampling
In Sonagachi, most of the buildings are multi-storied in nature; by and large each building accommodates several brothels. The number of rooms in each building varies from 5 to 25. Usually one sex worker occupies one room, but exceptions are there where one room is shared by two or more sex worker. There are three categories of sex workers as per the contractual agreement with land lord or with the Madams
1. Self-employed, who pays their rent directly to the landlord or land ladies and work according to their wishes
2. Adhiya System, under these system sex workers who work under a Malkin (Madam) and share half of their income with her
3. Third category of sex workers work are those who on contractual basis where she pays a fixed sum of money to madam based on number of client served
Research ethics approval
Preparation of the field
Selection criteria
Sample Frame: 10,100 (from the Register)
Expected prevalence rate of HIV was taken as 12.5%, based on which Sample Size was calculated as 400 [taking into the Confidence level=99.99% and Confidence interval=+6.30]
Sample size was adjusted upward to allow for non-response and other factors. Incorporating 5% for possible non-participation and 5% for non-respondent the adjusted sample size turns out to be 440.
Ref.: Epi info package
Data collection tools
The second section of the tool was meant to assess depression using the Inventory of Depressive Symptomatology-Self Report (IDS-SR) [38,39]. The IDS is a validated structured self-inventory that is used by trained professionals but lay interviewers are capable of assessing mental disorder according to the definition and criteria of the Diagnostic and Statistical Manual of Mental Disorders 4th edition (DSM-IV) [40]. The IDS-SR contains 28 questions rated on a scale of 0-3, with a maximum total of 84 (28*3=84). A score less than or equal to 13 signifies no depression, score ranging in between 14-25 denotes mild depression, between 26-38 qualify moderate depression, and score in the range of 39-48 signify severe depression, and more than or equal to score 49 denotes very severe depression. We used the tool based on DSM-IV for the reason that the same tool has been tried and tested in community settings both in India and in Mexico.
Ethical issues
Data collection methods
Participants detected to have severe or very severe depression (according to the IDS-SR) were offered and provided with treatment with the help of consultant psychiatrist.
Analysis
RESULTS
Depression rates
Sample characteristics and associations with depression
Age:
Education level:
Number of children:
Years in sex profession:
Using Chi-square analysis, no significant association was found to exist between depression and age (p=0.09), with the level of education (p=0.83), number of children (p=0.99), or years practicing in the sex trade (p=0.12). Refer to tables 1-3.
Risk behaviors
Condom use and negotiation:
Through Chi-Squared analysis, significant association was established between 100% condom use (the previous day) with depression (p=<0.01). Refer to tables 6, 11 and 12. The depressed FSWs are less likely to use condoms in 100% of sexual encounters. Similarly, there is a significant association between refusal of clients and depression (p=<0.01). As seen in figure 1, depressed FSWs are more likely to accept clients without using a condom than non-depressed FSWs.
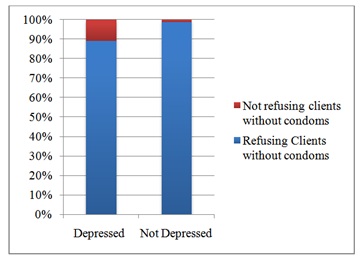 Figure 1: Percentages of refusal of clients without condoms for depressed vs non-depressed FSWs.
Figure 1: Percentages of refusal of clients without condoms for depressed vs non-depressed FSWs.Substance use:
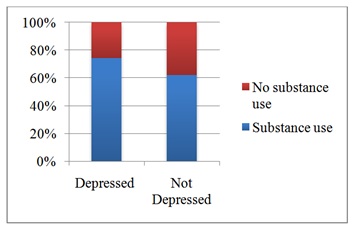 Figure 2: Percentages of substance use for depressed vs non-depressed FSWs.
Figure 2: Percentages of substance use for depressed vs non-depressed FSWs.Number of clients served per day:
Incidents of STI and health seeking behavior
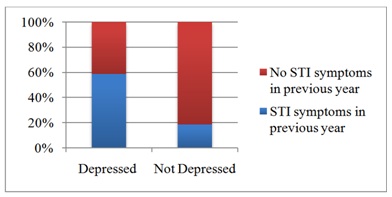 Figure 3: Percentages of STI symptoms within the past year for depressed vs non-depressed FSWs.
Figure 3: Percentages of STI symptoms within the past year for depressed vs non-depressed FSWs.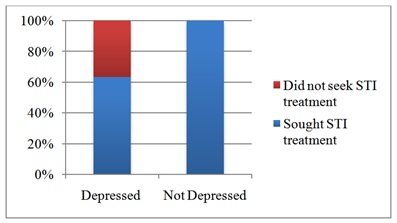 Figure 4: Percentages of seeking STI treatment for depressed vs non-depressed FSWs who suffered STI symptoms during the past year.
Figure 4: Percentages of seeking STI treatment for depressed vs non-depressed FSWs who suffered STI symptoms during the past year.Social well-being
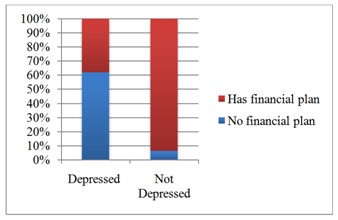 Figure 5: Percentages of FSWs having savings plans amongst depressed vs non-depressed FSWs.
Figure 5: Percentages of FSWs having savings plans amongst depressed vs non-depressed FSWs.Disputes with others:
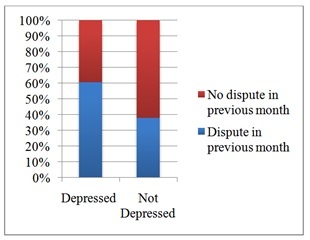 Figure 6: Percentages of FSWs involved in a dispute with other in the past month amongst depressed vs non-depressed FSWs.
Figure 6: Percentages of FSWs involved in a dispute with other in the past month amongst depressed vs non-depressed FSWs.DISCUSSION
Depression rates
Depression amongst FSWs in India and globally found to be associated with certain socio-demographic and sex trade related factors. Of note, studies have found that sex work itself may not be a casual factor behind depression. Rather, the constellation of challenging socio economic condition and marginalization of FSWs might be playing as the contributing or predisposing factor behind increase rate of depression. For instance, studies have found that FSWs’ poor mental well-being is associated with family-and partner-related burdens, stigma, discrimination, social isolation, loneliness, and violence [44].
In our study, there is no clear association between various demographic characteristics of sex workers and the rates of depression. These included age, education, number of children supported by them, and on the number of years they are in the sex work. Therefore, none of these factors contribute or predispose depression among the sex workers in Sonagachi. However there is a need to carry out further research, including the use of qualitative methods, to identify factors that may pre-dispose to depression and to verify its association with depression.
Sexual behaviors and HIV risk
Similarly, in the present study, depression is found to be associated with the decrease rates of refusal of clients who is not inclined to use condom and less use of condom with their clients. However, depression has no association with the number of clients being served by a sex worker in the previous day. Study findings shows that depression is associated with inconsistent condom use [49]. While the exact manner in which depression impacts on condom use rate is unclear, it may be due to reduced energy and motivation on the part of the individual to engage into condom negotiation or putting less value to the consequences of not using condoms. It could also be linked with her reduced sense of self-worth and hopelessness. Regardless, reduced condom use among depressed FSWs will certainly increase risks of accusing HIV infection. Consequently, identifying individuals with depression and providing counseling and other services to FSWs suffering from depression would help motivating them to use condom which will decrease HIV transmission risk [50,51].
STI rates and health seeking behavior
Substance use
In this study, approximately two-thirds of FSWs self-reported substance abuse with 60% of them reported use of alcohol and 25% of them are addicted to tobacco products. Only one participant found to use opioids. Furthermore, depression found to be associated with increased rate of substance use among FSWs. While tobacco use is a risk factor for cardiovascular, respiratory, and malignant diseases, alcohol may contribute to unsafe sex practices as it hinders condom use. Additionally, finances spent on alcohol consumption may divert resources away from establishing or maintaining financial stability. Therefore, identifying and treating both depression and substance use disorders among FSWs may positively impact on areas of physical, mental, and social well-being including cardio-pulmonary health, cancer risk, STI/HIV risk, and financial stability [58,59].
Financial and social well-being
In this study, depressed FSWs found more likely to be involved in significant number of disputes with others in the previous month, representing a disruption of social harmony and community well-being. While the current study cannot elaborate on why depressed FSWs are more likely to be engaged into varied kinds of disputes, it is possible that depression increases FSW’s levels of irritability, sense of isolation, and positive self-image, as well as motivation and energy to address potential conflicts to maintain social and community harmony. Thus depressed FSWs may be more prone to getting into conflicts but are also less likely to address those in a healthy manner. Thus addressing depression amongst FSWs may also impact social harmony and better integration with the community.
LIMITATIONS
This present study has its limitations in drawing conclusion to other sex-work contexts. DMSC has been operating in Sonagachi for last 20 years and altered the context in which brothel-based sex workers operate, including increase in condom use, decrease in STI rates, stabilization of HIV. DMSC through offering opportunities for financial savings, educational opportunities and increasing community cohesion and sex worker’s self-efficacy has helped empowering sex workers community. Thus findings from this study population may not be generalized to contexts where a similar long-term health and social interventions are not in operation. Moreover, these findings may be specific to a brothel-based sex worker only.
It is important to note that data collected on symptoms consistent with STIs, is not a full proof as it is not confirmed by laboratory tests. As a result, the study findings may not equivocally represent true STI cases among the FSWs in the study population [60].
In terms of assessing depression, the IDS-SR used in this study may not be comparable to other studies that utilize different tools to assess depression. Moreover, HIV rates are not collected from the study participants, thus HIV risk extrapolated based on previous reports and is not truly applicable to the study population.
CONCLUSION
This study contributes to the estimation of depression rate amongst brothel-based FSWs and probable association with depression and factors impacting FSW health and social well-being. Depression rate is found around 38.3% among sex workers in Sonagachi red light area. Depression is found to be associated with inconsistent condom use, increased STI rates, less interest in seeking STI treatment, increased substance use, and decreased financial planning and incidence of increased number of disputes with other family and community members. As a result, FSWs suffering from depression may be at increased risk of accusing HIV. Of note, this study did not find any association between depression and demographic factors including age, education, number of children, or years in sex work profession. Thus further research is needed to focus on plausible social and sex trade related factors and its association with depression amongst brothel-based FSWs as well as probing and identifying the relationship and manner in which depression results in increased risk of poor health and social well-being. Considering the impacts of depression on FSW’s well-being, future work could focus on designing interventions to address depression through incorporating prevention, screening, and treatment. Community-based, peer-led interventions proved to be highly effective among brothel-based FSWs, in India and in other regions, HIV prevention program needs to incorporate the findings of this study and to include mental health interventions as one of the element of HIV prevention program to enhance the outcome of HIV control program developed and implemented by the National AIDS Control Organization in India or in other countries.
Potential community based programming in the context of brothel-based sex work could include prevention initiatives, including screening program, as well as counseling and group therapy, utilizing both peers and multidisciplinary teams of health and social workers.
REFERENCES
- Scheid TL, Brown TN (2010) A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems, (2nd edn), Cambridge University Press, New York, USA.
- Friedli L, Jenkins R, McCulloch A, Parker C (2002) Developing a National Mental Health Policy. Psychology Press, Abingdon, UK.
- Patra S (2014) Perspectives on mental health and well-being in Indian context. BookStore, Haryana, India.
- https://sustainabledevelopment.un.org
- Shah B, Parhee R, Kumar N, Khanna T, Singh R, et al. (2005) Mental Health Research in India (Technical Monograph on ICMR Mental Health Studies) Division of Noncommunicable Diseases, Indian Council of Medical Reasearch, New Delhi, India.
- Reddy VM, Chandrashekar CR (1998) Prevalence of mental and behavioural disorders in India : a meta-analysis. Indian J Psychiatry 40: 149-157.
- Alegría M, Vera M, Freeman DH, Robles R, Santos MC, et al. (1994) HIV infection, risk behaviors, and depressive symptoms among Puerto Rican sex workers. Am J Public Health 84: 2000-2002.
- Hutton HE, Lyketsos CG, Zenilman JM, Thompson RE, Erbelding EJ (2004) Depression and HIV risk behaviors among patients in a sexually transmitted disease clinic. Am J Psychiatry 161: 912-914.
- Aral S, Peterman TA (2002) STD Diagnosis and Treatment as an HIV Prevention Strategy. In: O’Leary A (ed.). Beyond Condoms: Alternative Approaches to HIV Prevention, Springer, New York, USA.
- Blanchard JF, Bhattacharjee P, Kumaran S, Ramesh BM, Kumar NS, et al. (2008) Concepts and strategies for scaling up focused prevention for sex workers in India. Sex Transm Infect 2: 19-23.
- Foss AM, Watts CH, Vickerman P, Heise L (2004) Condoms and prevention of HIV. Are essential and effective, but additional methods are also needed. BzM 329: 185-186.
- Chandra PS, Desai G, Ranjan S (2005) HIV and psychiatric disorders. Indian J Med Res 121: 451- 467.
- Popoola BI (2013) Occupational hazards and coping strategies of sex workers in southwestern Nigeria. Health Care Women Int 34: 139-149.
- Collins PY, Holman AR, Freeman MC, Patel V (2006) What is the relevance of mental health to HIV/AIDS care and treatment programs in developing countries? A systematic review. AIDS 20: 1571-1582.
- Bassel N, Schilling RF, Irwin KL, Faruque S, Gilbert L, et al. (1997) Sex trading and psychological distress among women recruited from the streets of Harlem. Am J Public Health 87: 66-70.
- Cournos F, Empfield M, Horwath E, McKinnon K, Meyer I, et al. (1991) HIV seroprevalence among patients admitted to two psychiatric hospitals. Am J Psychiatry 148: 1225-1230.
- Brawner BM, Gomes MM, Jemmott LS, Deatrick JA, Coleman CL (2012) Clinical depression and HIV risk-related sexual behaviors among African-American adolescent females: Unmasking the numbers. AIDS Care 24: 618-625.
- Pereira B, Andrew G, Pednekar S, Pai R, Pelto P, et al. (2007) The explanatory models of depression in low income countries: Listening to women in India. J Affect Disord 102: 209-218.
- Chandra PS, Deepthivarma S, Manjula V (2003) Disclosure of HIV Infection in South India: Patterns, Reasons and Reactions. AIDS Care 15: 207-215.
- Tarakeshwar N, Krishnan AK, Johnson S, Solomon S, Sikkema K, et al. (2006) Living with HIV Infection: Perceptions of Patients with Access to Care at a Non-Governmental Organization in Chennai, India. Culture, Health Sexuality 8: 407-421.
- Tarakeshwar N, Khan N, Sikkema KJ (2006) A Relationship-based Framework of Spirituality for Individuals with HIV. AIDS Behav 10: 59-70.
- Carey MP, Weinhardt LS, Carey KB (1995) Prevalence of infection with HIV among the seriously mentally ill: Review of research and implications for practice. Professional Psychology: Research and Practice 26: 262-268.
- Cournos F, Empfield M, Horwath E, McKinnon K, Meyer I, et al. (1991) HIV seroprevalence among patients admitted to two psychiatric hospitals. Am J Psychiatry 148: 1225-1230.
- Kalichman SC, Kelly JA, Johnson JR, Bulto M (1994) Factors associated with risk for HIV infection among chronic mentally ill adults. Am J Psychiatry 151: 221-227.
- Blanchard JJ, Mueser KT, Bellack AS (1998) Anhedonia, positive and negative affect, and social functioning in schizophrenia. Schizophr Bull 24: 413-424.
- Carey MP, Carey KB, Weinhardt LS, Gordon CM (1997) Behavioral risk for HIV infection among adults with a severe and persistent mental illness: Patterns and psychological antecedents. Community Ment Health J 33: 133-142.
- Mueser KT, Doonan R, Penn DL, Blanchard JJ, Bellack AS, et al. (1996) Emotion recognition and social competence in chronic schizophrenia. J Abnorm Psychol 105: 271-275.
- Kalischman SC, Weinhardt L (2001) Negative affect and sexual risk behavior:Comment on Crepaz and Marks (2001). Health Psychol 20: 300-301.
- Lennon CA, Huedo-Medina TB, Gerwien DP, Johnson BT (2012) A role for depression in sexual risk reduction for women? A meta-analysis of HIV prevention trials with depression outcomes. Soc Sci Med 75: 688-698.
- Carey MP, Ravi V, Chandra PS, Desai A, Neal DJ (2007) Prevalence of HIV, Hepatitis B, Syphilis, and Chlamydia Among Adults Seeking Treatment for a Mental Disorder in Southern India. AIDS Behav 11: 289-297.
- Sahay S, Phadke M, Brahme R, Paralikar V, Joshi V, et al. (2007) Correlates of anxiety and depression among HIV test-seekers at a Voluntary Counseling and Testing facility in Pune, India. Qual Life Res 16: 41-52.
- Ling DC, Wong WC, Holroyd EA, Gray A (2007) Silent killers of the night: an exploration of psychological health and suicidality among female street sex workers. J Sex Marital Ther 33: 281-299.
- Sanders T (2004) A continuum of risk? The management of health, physical and emotional risks by female sex workers. Sociology of Health & Illness 26: 557-574.
- Wang B, Li X, Stanton B, Fang X, Yang H, et al. (2007) Sexual coercion, HIV-related risk, and mental health among female sex workers in China. Health Care Women Int 28: 745-762.
- Jackson LA, Bennett CG, Sowinski BA (2007) Stress in the sex trade and beyond: Women working in the sex trade talk about the emotional stressors in their working and home lives. Critical Public Health 17: 257-271.
- Shahmanesh M, Wayal S, Cowan F, Mabey D, Copas A, et al. (2009) Suicidal behavior among female sex workers in Goa, India: the silent epidemic. Am J Public Health 99: 1239-1246.
- Durbar, A Brief Profile, A Continuing Battle to Regain Dignity, Profiling of an inspiring journey of a sex-workers’ collective in Kolkata, Durbar, Kolkata, India.
- Rush AJ, Giles DE, Schlesser MA, Fulton CL, Weissenburger J, Burns C (1986) The Inventory for Depressive Symptomatology (IDS): preliminary findings. Psychiatry Res 18: 65-87.
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH (1996) The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychol Med 26: 477-86.
- American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders. APA, Washington, DC, USA.
- MacCallum RC, Zhang S, Preacher KJ, Rucker DD (2002) On the practice of dichotomization of quantitative variables. Psychol Methods 7: 19-40.
- NACO (2013) Annual Report 2012-13. NACO, Department of AIDS Control, Ministry of Health & Family Welfare, New Delhi, India.
- Vijayakumar G, Mabude Z, Smit J, Beksinska M, Lurie M (2006) A review of female-condom effectiveness: patterns of use and impact on protected sex acts and STI incidence. Int J STD AIDS 17: 652-659.
- Ngugi EN, Wilson D, Sebstad J, Plummer FA, Moses S (1996) Focused peer-mediated educational programs among female sex workers to reduce sexually transmitted disease and human immunodeficiency virus transmission in Kenya and Zimbabwe. J Infect Dis 174: 240-247.
- Kelly JA, Murphy DA, Bahr GR, Koob JJ, Morgan MG, et al. (1993) Factors associated with severity of depression and high-risk sexual behavior among persons diagnosed with human immunodeficiency virus (HIV) infection. Health Psychol 12: 215-219.
- Kennedy P, Hopwood M, Duff J (2001) Psychological Management of Chronic Illness and Disability. In: Milgrom J, Burrows GD (eds.). Psychology and Psychiatry: Integrating Medical Practice. University of Michigan, Wiley, Chichester, UK.
- Marks G, Crepaz , Senterfitt JW, Janssen RS (2005) Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr 39: 446-453.
- McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, et al. (2006) Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Educ Prev 18: 59-73.
- Munro S, Lewin S, Swart T, Volmink J (2007) A review of health behaviour theories: how useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS? BMC Public Health 7.
- Minnis AM, Padian NS (2005) Effectiveness of female controlled barrier methods in preventing sexually transmitted infections and HIV: current evidence and future research directions. Sex Transm. Infect 81: 193-200.
- Moore JS, Rogers M (2002) Female-controlled prevention technologies. In: O’Leary A (ed.). Beyond Condoms: Alternative Approaches to HIV Prevention, Springer, New York, USA. Pg no: 47-76.
- Semaan S, Des Jarlais DC, Sogolow E, Johnson WD, Hedges LV, et al. (2002) A meta-analysis of the effect of HIV prevention interventions on the sex behaviors of drug users in the United States. J Acquir Immune Defic Syndr 30: 73-93.
- Wariki WM, Ota E, Mori R, Koyanagi A, Hori N, et al. (2012) Behavioral interventions to reduce the transmission of HIV infection among sex workers and their clients in low-and middle-income countries. Cochrane Database Syst Rev.
- Vickerman P, Foss AM, Pickles M, Deering K, Verma S, et al. (2010) To what extent is the HIV epidemic in southern India driven by commercial sex? A modelling analysis. AIDS 24: 2563-2572.
- Sagtani RA, Bhattarai S, Adhikari BR, Baral D, Yadav DK, et al. (2013) Violence, HIV risk behaviour and depression among female sex workers of eastern Nepal. BMJ Open 3.
- Steen R, Hontelez JA, Veraart A, White RG, de Vlas SJ (2014) Looking upstream to prevent HIV transmission: can interventions with sex workers alter the course of HIV epidemics in Africa as they did in Asia? AIDS 28: 891-899.
- Arora P, Nagelkerke NJ, Moineddin R, Bhattacharya M, Jha P (2013) Female sex work interventions and changes in HIV and syphilis infection risks from 2003 to 2008 in India: a repeated cross-sectional study. BMJ open 3.
- Suresh G, Furr AL, Srikrishnan AK (2009) An Assessment of the Mental Health of Street-Based Sex Workers in Chennai, India. Journal of Contemporary Criminal Justice 25.
- Beattie TSH, Bhattacharjee P, Ramesh BM, Gurnani V, Anthony J, et al. (2010) Violence against female sex workers in Karnataka state, south India: impact on health, and reductions in violence following an intervention program. BMC Public Health 10: 1-11.
- National Institute Mental Health Intervent (2001) An integrated framework for preventive and treatment interventions. National Institute Mental Health Intervent, Washington, D.C., USA.
Citation: Jana S, Ray P, Roy S, Piduttia J, Ghose T, et al. (2017) Depression and Its Relation with HIV Risk and Social Well-Being among the Brothel-Based Female Sex Workers in Kolkata, India. J Community Med Public Health Care 4: 025.
Copyright: © 2017 Smarajit Jana, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

