
Determinants of Community Involvement in Community Based Health Insurance Enrollment Program among Residents at Debre Markos Town, 2024
*Corresponding Author(s):
Baye Tsegaye AmlakDepartment Of Nursing, College Of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
Email:baye_tsegaye@dmu.edu.et
Abstract
Introduction
Community-Based Health Insurance (CBHI) is designed to improve access to healthcare for low-income and rural populations and supports progress toward universal health coverage. However, factors influencing enrollment in CBHI in Debre Markos town have not been adequately explored.
Objective
To identify key determinants affecting community enrollment in CBHI programs in Debre Markos city, 2024.
Methods
A community-based cross-sectional study was conducted among 342 systematically selected household heads. Data were collected using a semi-structured questionnaire and analyzed using SPSS version 25. Binary logistic regression was used to identify factors associated with CBHI enrollment. Variables with a p-value < 0.25 in bivariable analysis were entered into multivariable logistic regression. Statistical significance was set at p < 0.05.
Results
Of the 342 sampled, 321 responded (93.85% response rate). Among them, 207 (64.6%) were enrolled in CBHI. Significant predictors included family size of 4-6 members (AOR=1.95), frequent health facility visits (AOR=2.71), awareness of CBHI (AOR=3.24), and non-participation in local meetings (AOR=2.11).
Conclusion
Despite CBHI's potential, a substantial proportion of the community remains unenrolled. Family size, healthcare utilization, awareness, and engagement in local meetings are key factors influencing CBHI participation in Debre Markos.
Keywords
CBHI; Debre Markos town; Determinants; Enrollment; Ethiopia; Residents
Highlights
- Community based cross sectional study design was conducted among households heads at Debre Markos town.
- Binary logistic regression model was used to identify factors associated with community based health insurance enrolment.
- Among the study participants 207 (64.6%), [95% CI: (59.7-69.8%)] were enrolled in CBHI programs.
- Family size, frequency of health institution visits, awareness about CBHI, and participation in local meeting were identified as the key factors of community enrollment in community based health insurance.
Introduction
Health insurance has been positioned as the main source of funding for expanding access to healthcare and mitigating financial risk. The four primary types of health insurance schemes are Community-Based Health Insurance (CBHI), Private Health Insurance (PHI), Social Health Insurance (SHI), and National Health Insurance (NHI) [1]. Access to health insurance is expected to have positive effect in improving access to healthcare and offer financial risk protection to households. It ensure equitable access to basic healthcare for all residents [2].
Community-Based Health Insurance (CBHI) is a type of health insurance that is especially well- suited for low-income and rural populations, as well as the informal sector in low- and middle- income nations [3]. It is one promising way to offer financial protection for all, especially to the unemployed and rural population. It provides a financial buffer against medical expenses, serving as a tool for complete health facility protection. It could have a significant impact on enrolled populations' financial security and use [4,5].
A useful instrument for achieving universal health coverage is the CBHI, which increases access to high-quality medical treatment [6]. In Low- and Middle-Income Countries (LMICs), Community-Based Health Insurance (CBHI) has emerged as a substitute for out-of-pocket medical expenses, especially in regions with low levels of government or employer-sponsored health insurance [7].
Since the mid-1990s, several LMICs have been implementing various types of health insurance programs as a response to the global effort to move away from the reliance on Out-of-Pocket Payment (OPP) for health towards risk-pooling [8,9].
Lack of access to healthcare negatively affects a person's capacity for risk management, human capital development, and sense of dignity. Policymakers and experts have recently become interested in a growing movement of CBHI programs since it appears that these programs more effectively target the impoverished [10].
An important aspect that sets the CBHI scheme apart from other health insurance plans is that enrollment is voluntary. This is consistent with the theory that people's decision to join and/or remain a member of the program may be influenced by their level of trust in healthcare institutions [11]. This thesis was examining the impact of community enrollment in community- based health insurance on the utilization of healthcare services in Debre Markos city.
Worldwide, there is a chronic shortage of funding for health care, especially in emerging nations like Africa where the expense of healthcare is always rising [12]. The World Health Organization (WHO) states that actual data suggests that paying for medical care out of pocket is the least effective and equitable way to pay for healthcare. It also discourages individuals from getting care and may make poverty worse [13].
Ethiopia's health care system is among the worst in Sub-Saharan Africa and the entire world. Due to a limited budget for healthcare and a lack of sophisticated methods for raising money for it, Ethiopia's health care financing system heavily relies on high out-of-pocket costs [14]. In low-resource settings, CBHI programs have been viewed as a step toward achieving Universal Health Coverage (UHC). In this strategy, community is important because governments often face two challenges: (1) they cannot fund enough insurance for all the people in resource- constrained settings; and (2) it is difficult to collect premiums and taxes, particularly in rural areas where many residents do not have regular sources of earned income [15,16].
LMICs have struggled to provide their populations with fair healthcare. It was difficult for them to raise enough money to pay for medical services. As a result, they are currently endorsing the CBHI as a way to pay for medical care. However, due of the low rate of member enrolment, it had not had a significant impact on healthcare accessible [17-19].
A large number of individuals living in LMICs frequently face unaffordable medical expenses [3]. The Ethiopian government has been devoted to finding a way to shift from catastrophic OOP expenditure to ensure accessibility targeting quality and equity to achieve UHC [14].
Low enrolment in voluntary health insurance schemes in LMICs is common and has been attributed to several factors including the lack of adequate consumer information, lack of understanding of the insurance concept and the benefit package among the target population, lack of trust in insurers, perceived poor quality of available healthcare services, poverty, unaffordable premiums, unfavorable timing of the premium payment, institutional rigidities, large informal sector and low levels of education [2,20,21].
A systematic review and meta-analysis conducted in low and middle income countries showed that low levels of income, lack of financial resources, and poor healthcare quality were the major factors affecting enrolment in CBHI [22].
In 2011, a study result revealed that community-based health insurance enrollment in Ethiopia was 45.5%, which is very low [23]. On the other hand, the determinant factors of CBHI enrollment in the study area was not addressed. There are variables (substance use related and social support) which were not addressed in previous studies will be included in this study. Therefore, this study aims to identify major determinant factors that influence community enrollment in CBHI in Debre Markos town. Therefore, this study aimed to determine the effectiveness of targeted community engagement strategies in increasing enrollment and reducing dropout rates in Community-Based Health Insurance (CBHI) programs in Debre Markos city.
Materials And Methods
Study Design
A Community based cross sectional study was employed.
Study Area and Period
This study was conducted in Debre Markos town, East Gojjam Zone. It is situated at about 26km North East of Bahir Dar (capital of Amhara regional state) and 299km far from the capital city of Ethiopia, Addis Ababa. The town has 12 kebeles with an estimated population of over 140 thousand. Also the town has 1 comprehensive specialized hospital and 4 health centers. The town has been seen in implementing CBHI program. The study period was carried out from Nov 25- December 25, 2024.
Target Population
The target population for this includes all households’ heads of Debre Markos city.
Study Population
Randomly selected households’ heads from a sampled household were the study population.
Inclusion Criteria
All house hold heads who are living more than 6 months in the town.
Exclusion Criteria
Household heads who are not permanent resident in the town, government employees, Retire, and living less than 6 months were excluded.
Sample Size Determination
The sample size for the quantitative part of the study was determined using Cochran's formula for sample size calculation in large populations. The formula is given by: 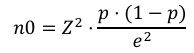
Where:
n Sample size
=Z-value (the number of standard deviations from the mean corresponding to the desired confidence level, typically 1.96 for a 95% confidence level)
pp=Estimated proportion of the population with participation in CBHI which equals 0.281.
e2=Margin of error (desired precision, typically 0.05 for a 5% margin of error)
Sample Size
Assuming a 95% confidence level and a 5% margin of error, and using an estimated proportion of 0.281:
 By adding 10% non-response rate: 311+31=342. Thus, the final sample size was approximately 342 participants.
By adding 10% non-response rate: 311+31=342. Thus, the final sample size was approximately 342 participants.
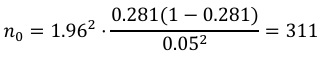
Sampling Technique and Procedure
The study was employ a two-stage sampling technique to ensure representativeness and manageability of the sample. In the first stage, the proportion of samples from each kebele were identified based on the number of residents in each kebele. In the second stage, households were chosen using a systematic random sampling technique. A random starting point was selected, and then every nth household was included in the sample (Figure 1).
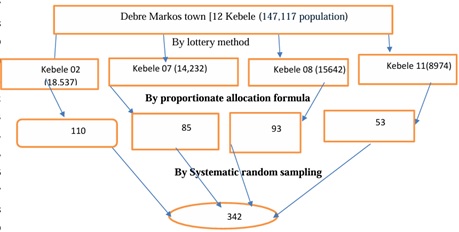 Figure 1: Schematic presentation of sampling technique and procedures community enrollment on community based health insurance among residents at Debre Markos town, 2024.
Figure 1: Schematic presentation of sampling technique and procedures community enrollment on community based health insurance among residents at Debre Markos town, 2024.
Variables
Dependent Variables
Enrollment in Community-Based Enrollment in CBHI (enroll): A binary variable representing whether a household is enrolled (1) or unenrolled (0) in the Community-Based Health Insurance (CBHI) scheme.
Independent Variables
- Sociodemographic Variables: Like age, sex, ethnicity, family size, educational status, religion, household Income, marital status, household income, time to arrive the health institution, presence chronic illness among family members, and participating in local meetings.
- CBHI Service Related Variables: Availability of health service, CBHI awareness, Frequency of visiting health facility.
- Perception of Households Towards CBHI Scheme Variables: CBHI trustworthy, Health service quality, Adequacy of CBHI, providers’ decision on diagnosis.
- Substance Use Related Factors: like using Khat, alcohol, smoking.
- Health Services Availability (available): A categorical variable that shows the accessibility and availability of healthcare services to the household (1=available, 0=Not available).
- Awareness of CBHI (aware): A categorical variable that show the level of knowledge and understanding household members have about the CBHI scheme (1=Aware, 0=Not aware).
Operational Definitions
- Availability of Health Facility: in this study implies that existence of governmental health facility within a 30 minute walking distance.
- Chronic Illness Experience: it is households or member of households who get an illness lasting more than six months preceding the data collection period [24].
- Low Social Support: Participants having <3 score in social support scoring scale,
- Moderate Social Support: Participants having 3-5 score in social support scoring scale, and
- Strong Social Support: Participants having >5 score in social support scoring scale [25].
Data Source and Data Type
Structured questionnaire to gather data from selected representative households in the town. Data were collected via interviewer-administered questionnaire. Data were collected from village residents interview administered questionnaires and semi-structured interviews.
The questionnaire for all respondents was translated into Amharic, which is the mother tongue in the study area. Three CBHI experts from the town Health office were selected and trained by the researcher for the purpose of using them as data collectors from the respondent community’s heads.
Data Collection Tools and Procedures
At the beginning, the questionnaire was prepared based on the reviewed literature and basic Questions of the study. The response gathered from respondents were tabulated, analyzed and interpreted carefully and thoroughly. At the end questionnaires and semi-structured interview questions were attached.
A structured questionnaire was considered as a major data collection tool and it is administering the determinants on communities’ decision CBHI enrolment. To validate the study, structured and a semi-structured type of predetermined questions were prepared and conducted with participants and non-participants of CBHI in the town.
Method of Data Analysis
Data collected through interview-administered questionnaires from community head respondents were entered into SPSS version 25 for initial data entry and management. The data were then be exported to SPSS version 25 software for detailed statistical analysis.
Descriptive statistics such as means, medians, modes, standard deviations, and frequencies were used to summarize the data. These statistics provide a clear picture of the general characteristics and trends within the data. Graphs, tables, and charts were used to visually present the data, making it easier to interpret the results.
Logistic regression analysis was employed to examine the relationship between the dependent variable (community involvement in CBHI enrollment) and various independent variables (e.g., socioeconomic factors, awareness levels, and perceived benefits). The logistic regression model helps in understanding the likelihood of community involvement based on different predictor variables.
The association between the dependent variable and independent variables was assessed using p-values and 95% confidence intervals (CI). The Adjusted Odds Ratio (AOR) was used to determine the strength of the association, adjusting for potential confounding variables. A p-value of less than 0.05 was considered statistically significant, indicating a less than 5% probability that the observed association is due to chance.
Data Quality Control
Training and orientation for the supervisors and data collectors was given. In order to evaluate the clarity of the questions in the questionnaire and to ensure that the reaction of the respondents to the questions, pretest was done on 5% of study subjects before one week of the actual data collection period. Also appropriate modification on the questionnaire was done. The collected data were reviewed and checked for its completeness before data entry and incomplete data were discarded. SPSS was used for data entry.
Ethical Considerations
Ethical clearance was obtained from Debre Markos University College of business and economics Ethical Review Committee. Description of the thesis purpose, and an offer to answer all inquiries were made to the respondents. Oral consent was used. Also affirmation that they are free to withdraw consent and to discontinue participation was made. Privacy and confidentiality of collected information were ensured throughout the process as no name is written. This study was conducted in accordance with the declaration of Helsinki.
Results
Out of 342 participants, 321 were really participated in the study giving a response rate of 93.85%. Nearly one-three, 110 (34.3%), of the participants were in the age group of 41-50, with another 28.1% (90) in the 31-40 group, reflecting a predominance of younger participants. In terms of education, the majority had completed primary school (120, 37.4%). Regarding household income, majority of participants, 59.5% (191), reported earning between 1,000-5,000 ETB, while 37.4% (120) had a chronic illness in the household, which could potentially influence their health insurance decisions (Table 1).
|
Variables |
Category |
Frequency( n) |
Percent (%) |
|
Sex |
Male |
160 |
49.84 |
|
Female |
161 |
50.16 |
|
|
Age group of the participants |
18-30 |
40 |
12.45 |
|
31-40 |
90 |
28.1 |
|
|
41-50 |
110 |
34.3 |
|
|
51+ |
81 |
25.2 |
|
|
Religion |
Christian |
280 |
87.2 |
|
Muslim |
35 |
10.9 |
|
|
Protestant |
6 |
1.9 |
|
|
Ethnicity of the respondent |
Amhara |
267 |
83.2 |
|
Oromo |
9 |
2.8 |
|
|
Tigre |
45 |
14.0 |
|
|
Marital status |
Married |
220 |
68.5 |
|
Single |
85 |
26.5 |
|
|
Divorced/Widowed |
16 |
5.0 |
|
|
Family size |
1-3 members |
120 |
37.4 |
|
4-6 members |
160 |
49.8 |
|
|
7+ members |
41 |
12.8 |
|
|
Educational status |
Can’t read and write |
40 |
12.5 |
|
|
Can read and write |
110 |
34.3 |
|
|
Primary |
120 |
37.4 |
|
|
Secondary and above |
51 |
15.9 |
|
Occupational status |
Merchant |
88 |
27.44 |
|
|
Daily laborer |
57 |
17.76 |
|
|
No Job |
99 |
30.8 |
|
|
Others |
77 |
24.00 |
|
Household monthly income |
<1,000 |
68 |
21.18 |
|
1,000-5,000 |
191 |
59.5 |
|
|
>5,000 |
62 |
19.32 |
|
|
Chronic Illness in Household |
Yes |
120 |
37.4 |
|
No |
201 |
62.6 |
|
|
Participates in local meeting |
Yes |
190 |
59.2 |
|
No |
131 |
40.8 |
Table 1: Presents the distribution of participants by sociodemographic characteristics (N=321).
Perception toward Community Based Health Insurance
Out of 321 participants, 218 (67.9%) had a poor perception while the remaining 103 (32.1%) had a good perception. This suggests that the majority of the participants may have concerns or negative views towards the CBHI program, with fewer showing positive support.
Community Based Health Insurance Related Factors
Among the total participants nearly two third, 201 (62.7%) had awareness towards CBHI and only 31.8% confirmed that health services were readily available, signaling a need for improvement in health infrastructure or service delivery to meet the population's needs (Table 2).
|
Variables |
Category |
Frequency (n) |
Percent (%) |
|
CBHI Awareness |
Aware |
201 |
62.7 |
|
Not Aware |
120 |
37.3 |
|
|
Frequency of Health Institution Visits |
Frequently Visit |
134 |
41.7 |
|
Not Frequently Visit |
187 |
58.3 |
|
|
Availability of Health Services |
No |
219 |
68.2 |
|
Yes |
102 |
31.8 |
Table 2: CBHI service-related factors among residents in Debre Markos Town (N=321).
Social Support of the Participants
Social support-It computes from the means of 12 items of multi-dimensional social support questions. Nearly half of the participants, 155 (48%) had low social support. Mean of overall social support become 4.4 (Figure 2).
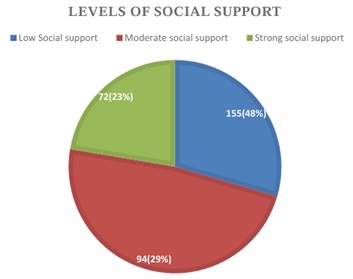 Figure 2: Showing social support level among residents Debre Markos Town, North West, Ethiopia, 2024 (N=321).
Figure 2: Showing social support level among residents Debre Markos Town, North West, Ethiopia, 2024 (N=321).
Community Based Health Insurance Enrollment
Among the study participants 207 (64.6%), [95% CI: (59.7-69.8%)] were enrolled in CBHI programs (Figure 3).
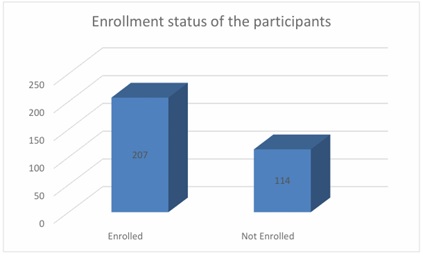 Figure 3: Showing level of community Enrollment in Community based health insurance among residents in Debre Markos town.
Figure 3: Showing level of community Enrollment in Community based health insurance among residents in Debre Markos town.
Factors Associated with CBHI Enrollment
In variable logistic regression analysis the predictor variables: sex, family size, frequency of health institution visits, awareness on CBHI, participate in local meeting, house hold monthly income, and social support were eligible to entered in multivariable logistic regression.
In multivariable logistic regression analysis, the predictor variables: family size, frequency of health institution visits, awareness on CBHI, participate in local meeting were statistically significant predictors of CBHI enrollment among residents of Debre Markos town.
Family size 4-6 members was about 2 times [AOR=1.95; 95%CI (1.24-3.06)] more likely Enrolled in CBHI programs than family size of 1-3 members. Residents who were frequently visit health institution were 2.7 times [AOR=2.71; 95%CI (1.88-4.29)] more likely Enrolled in CBHI programs as compared to their counter parts. On the other hand participants who had awareness on CBHI were about 3.2 times [AOR=3.24; 95% CI (4.06-5.54) more likely enrolled in CBHI programs than their counter parts. Those participants who participated in local meetings were 2 times [AOR=2.11; 95%CI (1.74-2.98)] more likely to enrolled in CBHI programs as compared to those who participate in local meetings (Table 3).
|
Variable |
Enrollment |
COR (95%CI) |
P value |
AOR (95%CI) |
P value |
||
|
Enrolled |
Not Enrolled |
||||||
|
Sex |
Female |
111 |
50 |
1.48(0.742-2.061) |
0.092 |
1.95(0.33-3.12) |
0.81 |
|
Male |
96 |
64 |
1 |
|
1 |
|
|
|
Family size |
1-3 members |
80 |
40 |
1 |
|
1 |
|
|
4-6 members |
105 |
55 |
1.05(0.946-2.081) |
0.092 |
1.95(1.24-3.06) |
0.03 |
|
|
7+ members |
22 |
19 |
1.73(.983-2.119) |
0.061 |
0.86(0.36-4.42) |
0.74 |
|
|
Frequency of health institution visit |
Frequent |
105 |
29 |
3.02(1.15-4.72) |
0.015 |
2.71(1.88-4.29) |
0.12 |
|
Not frequent |
102 |
85 |
1 |
|
1 |
|
|
|
Awareness on CBHI |
Aware |
151 |
50 |
3.45(4.162-5.515) |
0.006 |
3.24(4.06-5.54) |
0.03 |
|
Not Aware |
56 |
64 |
1 |
|
1 |
|
|
|
Participate in local meeting |
Yes |
142 |
48 |
2.21(1.52-3.45) |
0.00 |
2.11(1.74-2.98) |
0.01 |
|
No |
75 |
56 |
1 |
|
1 |
|
|
|
Household monthly income |
<1,000 |
42 |
26 |
1.2(2.03-6.61) |
0.000 |
1.27(0.39-4.16) |
0.69 |
|
1,000-5,000 |
128 |
63 |
1.53(2.03-6.61) |
0.000 |
1.61(0.29-4.05) |
0.71 |
|
|
>5,000 |
35 |
27 |
1 |
|
1 |
|
|
|
Social support |
Low |
106 |
49 |
3.02(1.69-6.86) |
0.001 |
1.40(0.32-6.14) |
0.65 |
|
Moderate |
71 |
23 |
4.32(0.98-2.43) |
0.061 |
1.36(0.52-3.54) |
0.53 |
|
|
Strong |
30 |
42 |
1 |
|
|
|
|
Table 3: Bivariable and Multivariable Logistic regression analysis of determinants of CBHI among residents of Debre Markos town, North West, Ethiopia, 2024 (N=321).
Discussion
The findings of this study show that a significant portion of residents in Debre Markos town (64.6%) are enrolled in Community-Based Health Insurance (CBHI) programs, indicating a relatively high uptake of these health insurance schemes. The study identified several socio- demographic and behavioral predictors of CBHI enrollment, including family size, frequency of health institution visits, awareness about CBHI, and participation in local meetings. These predictors align with previous studies that have examined factors influencing the uptake of CBHI programs in different regions.
Family size was found to be a significant predictor of CBHI enrollment, with households having 4-6 members being about twice as likely to enroll in CBHI programs compared to smaller families (1-3 members) [AOR=1.95; 95% CI (1.24-3.06)]. This finding is consistent with study conducted Tanzania [26], which is found that larger family sizes were positively associated with CBHI enrollment, as households with more members may feel a greater need for financial protection against health-related costs. Larger families may also have more diverse health needs, making them more inclined to join health insurance schemes [27].
This result is in line with research from other areas that indicates larger families are more likely to enroll in health insurance programs because they must pay higher household medical expenses. Furthermore, participation in insurance is required for financial protection against health risks because bigger family sizes are frequently linked to higher levels of poverty and vulnerability [28].
The frequency with which individuals visit health institutions was another important predictor, with frequent visitors being 2.7 times more likely to enroll in CBHI programs [AOR=2.71; 95%CI (1.88-4.29)]. According to this research, those who often seek medical attention are more likely to be aware of and inclined to sign up for health insurance plans. Regular encounters with healthcare professionals improve exposure to health insurance information, increasing enrollment prospects, according to prior research. Additionally, people who often interact with the healthcare system might be directly affected by the costs of medical care, which may persuade them to look for insurance coverage in order to lower out-of-pocket expenses [29,30].
Awareness of CBHI programs was a strong predictor of enrollment, with those who were aware of CBHI being 3.2 times more likely to enroll than those who were unaware [AOR=3.24; 95% CI (4.06-5.54)]. According to our research, raising public awareness through focused marketing can greatly boost health insurance program participation rates. The goal of these advertisements should be to inform people about the benefits of CBHI, including the overall increase in access to healthcare services and financial protection against catastrophic medical bills [31].
Interestingly, the study found that individuals who participated in local meetings were more likely to enroll in CBHI programs [AOR=2.11; 95% CI (1.74-2.98)], Involving the community, especially through local gatherings, seems to be a crucial approach to spread knowledge and build confidence in health activities. Prior studies have demonstrated that community-based health insurance plans that involve people in dialogue and decision-making have a higher chance of success. Participants are more likely to experience a feeling of ownership and trust in CBHI projects, and these local meetings provide forums for talking about the advantages and difficulties of these initiatives. Consequently, health organizations looking to improve CBHI enrollment should prioritize raising attendance at local meetings [32].
The study's conclusions have significant ramifications for health administrators and legislators. Focusing on the identified determinants: family size, frequency of health institution visits, knowledge of CBHI services, and community engagement is essential to raising CBHI enrollment rates. To promote trust and the spread of knowledge about CBHI, health authorities should create focused outreach programs for larger households, provide people more chances to engage with healthcare professionals, and fund neighborhood gatherings. Community health professionals can be crucial in educating families and assisting with CBHI enrollment, therefore policymakers should think about include them in these programs [30].
Conclusion and Recommendation
Conclusion
The study reveals significant factors influencing enrollment in Community-Based Health Insurance (CBHI) programs among participants. About two thirds of the participants were enrolled in CBHI programs. Key determinants of enrollment include family size, frequency of health institution visits, awareness about CBHI, and participation in local meetings. Larger families (4-6 members) were found to be nearly twice as likely to enroll in CBHI programs compared to smaller families (1-3 members). Additionally, individuals who frequently visited health institutions had a much higher likelihood of enrolling in CBHI. Awareness of CBHI significantly increased the likelihood of enrollment, with those aware being over three times more likely to participate. Interestingly, participants who did not participate in local meetings were also more likely to enroll compared to those who engaged in such meetings.
Recommendation
To Debre Markos Town Health Insurance Office: Targeted awareness campaigns shall be given to improving public awareness about CBHI programs, especially targeting populations with limited knowledge. Outreach programs can utilize various media channels to educate the public on the benefits and opportunities offered by CBHI.
Encourage Health-Seeking Behavior: Since frequent visits to health institutions were linked to a higher likelihood of enrollment, promoting regular health checkups and services could encourage more individuals to join CBHI programs. Partnerships with health institutions to provide information about CBHI at the point of service could be effective.
Support Larger Families: Recognizing the higher enrollment rates among larger families, policy interventions could focus on making CBHI more accessible and affordable for larger households, possibly through family-oriented plans or subsidies.
Evaluate the Role of Local Meetings: The inverse relationship between participation in local meetings and CBHI enrollment suggests that community engagement strategies could be re- evaluated. Exploring the reasons why non-participants in local meetings are more likely to enroll might uncover new insights into community dynamics and health program participation.
Abbreviations and Acronyms
AOR: Adjusted Odds Ratio
COR: Crude Odds ratio
CBHI: Community Based Health Insurance
LMICs: low- and middle-income countries
NGOs: Non-Governmental Organizations
UHC: Universal health coverage
WHO: World Health Organization
Declarations
Ethics Approval and Participant Consent
Before conducting the study, the proposal was presented and defended. Ethical clearance was obtained from the Institutional Review Board (IRB) of Debre Markos University. The IRB had reviewed the study protocol and approved it. Prior to data collection, informed written consent was obtained from the study participants. Confidentiality of the information was maintained throughout the study.
Consent to Publication
The study does not include images or videos relating to an individual’s recorded data, but concerning other collected and used data in the study, there is no doubt on consent of publication.
Availability of Data and Materials
The data set used and analyzed during the current study is available from the corresponding author on reasonable request.
Conflicts of Interest
The author (s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: No specific funding for this work.
Clinical Trial Number: Not applicable.
Author’s Contribution
BM, BTA: Writing the original draft, wrote the main manuscript text, analyze the work. BM, BTA, MW, and BT: All authors made a significant contribution to the work reported, whether to the conception, study design, execution, acquisition of data analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work. All authors read and approved the final draft of the manuscript.
Acknowledgment
First of all, we would like to thank Debre Markos University for giving a chance to conduct this study. Secondly, we would like to thank East Gojjam zone health insurance office for the strong support on providing data regarding the source population and help on data gathering. We would also like to give our appreciation to the data collectors and supervisors for their endeavor.
References
- Wang H, Switlick K, Ortiz C, Zurita B, Connor C (2012) Health insurance handbook: How to make it work. World Bank Publications.
- Kusi A, Enemark U, Hansen KS, Asante FA (2015) Refusal to enrol in Ghana’s National Health Insurance Scheme: Is affordability the problem? International journal for equity in health 14: 1-14.
- Adebayo EF, Ataguba JE, Uthman OA, Okwundu CI, Lamont KT, et al. (2014) Factors that affect the uptake of community-based health insurance in low-income and middle-income countries: A systematic protocol. BMJ Open 4: 004167.
- Spaan E, Mathijssen J, Tromp N, McBain F, Have A, et al. (2012) The impact of health insurance in Africa and Asia: A systematic review. Bulletin of the World Health Organization 90: 685-692.
- Chen C, Pan J (2019) The effect of the health poverty alleviation project on financial risk protection for rural residents: Evidence from Chishui City, China. International Journal for Equity in Health 18: 1-16.
- Conde KK, Camara AM, Jallal M, Khalis M, Zbiri S, et al. (2022) Factors determining membership in community-based health insurance in West Africa: A scoping review. Global Health Research and Policy 7: 46.
- Fadlallah R, El-Jardali F, Hemadi N, Morsi RZ, Samra CA, et al. (2018) Barriers and facilitators to implementation, uptake and sustainability of community-based health insurance schemes in low-and middle-income countries: A systematic review. International journal for equity in health 17: 1-18.
- Preker AS, Carrin G (2004) Health financing for poor people: Resource mobilization and risk sharing. World Bank Publications.
- Acharya A, Vellakkal S, Taylor F, Masset E, Satija A, et al. (2012) Impact of national health insurance for the poor and the informal sector in low-and middle-income countries. London The EPPI-Centre.
- Jütting J (2003) Health insurance for the poor? Determinants of participation in community-based health insurance schemes in rural Senegal.
- Akafu W, Daba T, Tesfaye E, Teshome F, Akafu T (2023) Determinants of trust in healthcare facilities among community-based health insurance members in the Manna district of Ethiopia. BMC Public Health 23: 171.
- Jude A, Atanga S, Falang C, Nso E (2018) Factors associated with non enrollment into community based health insurance schemes in the Bamenda Health District, Cameroon. Int J Public Health Epidemiol Res 4: 60-70.
- World Health Organization (2000) The world health report 2000: Health systems: Improving performance. World Health Organization, Geneva, Swaziland.
- Hope RL (2003) Paying in potatoes: Community-based health insurance for the rural and informal sector. The Lancet 362: 827-829.
- Ko H, Kim H, Yoon CG, Kim CY (2018) Social capital as a key determinant of willingness to join community-based health insurance: A household survey in Nepal. Public Health 160: 52-61.
- Allegri MD, Pokhrel S, Becher H, Dong H, Mansmann U, et al. (2008) Step-wedge cluster-randomised community-based trials: An application to the study of the impact of community health insurance. Health Research Policy and Systems 6: 1-8.
- Macha J, Kuwawenaruwa A, Makawia S, Mtei G, Borghi J (2014) Determinants of community health fund membership in Tanzania: A mixed methods analysis. BMC health services research 14: 1-11.
- Noubiap JJN, Joko WYA, Obama JMN, Bigna JJR (2014) Community-based health insurance knowledge, concern, preferences, and financial planning for health care among informal sector workers in a health district of Douala, Cameroon. Pan African Medical Journal 16: 17.
- Chankova S, Atim C, Hatt L (2010) Impact of Health Insurance in low-and middle-Income Countries. Brookings Institution Press, USA.
- Criel B, Waelkens MP (2003) Declining subscriptions to the Maliando mutual health organization in Guinea-Conakry (West Africa): What is going wrong? Social science & medicine 57: 1205-1219.
- Adebayo EF, Uthman OA, Wiysonge CS, Stern EA, Lamont KT, et al. (2015) A systematic review of factors that affect uptake of community-based health insurance in low-income and middle- income countries. BMC health services research 15: 543.
- Mebratie AD, Sparrow R, Yilma Z, Alemu G, Bedi AS (2015) Enrollment in Ethiopia’s community-based health insurance scheme. World Development 74: 58-76.
- Chanie MG, Ewunetie GE (2019) Determinants of enrollment in community based health insurance among Households in Tach-Armachiho Woreda, North Gondar, Ethiopia, 2019. PloS One 15: 0236027.
- Zimet G, Dahlem N, Zimet S, Fairley G (1988) The multidimentional scale of percieved social support. Jornal of personality assessment 52: 30-41.
- Mapoy NK, Bonza ZH, Minga NM, Kemirembe DP, Kabago L (2023) The Influence of Socio- Economic Factors on the Membership Status of Health Insurance Schemes: A Case of the Informal Sector in Tanzania.
- Domapielle MK (2014) Health insurance and access to health care services in developing countries. Indonesian Journal of Government and Politics 5: 30964.
- Hossain SI (1990) Interrelations between child education, health, and family size: Evidence from a developing country. Economic Development and Cultural Change 38: 763-781.
- Degroote S, Ridde V, Allegri MD (2020) Health insurance in sub-Saharan Africa: A scoping review of the methods used to evaluate its impact. Applied Health Economics and Health Policy 18: 825-840.
- Habiyonizeye Y (2013) Implementing community-based health insurance schemes: Lessons from the case of Rwanda. Thesis submitted for the Master Degree in International Social Welfare and Health Policy Autumn term 2013.
- Yusuf H, Kanma-Okafor O, Ladi-Akinyemi T, Eze U, Egwuonwu C, et al. (2019) Health insurance knowledge, attitude and the uptake of community-based health insurance scheme among residents of a suburb in Lagos, Nigeria. West Afr J Med 36: 103-111.
- Bayked EM, Toleha HN, Kebede SZ, Workneh BD, Kahissay MH (2023) The impact of community-based health insurance on universal health coverage in Ethiopia: A systematic review and meta-analysis. Global Health Action 16: 2189764.
- Smith KV, Sulzbach S (2008) Community-based health insurance and access to maternal health services: Evidence from three West African countries. Soc Sci Med 66: 2460-2473.
Citation: Manaye B, Amlak BT, Wondim M, Alemu BT (2025) Determinants of Community Involvement in Community Based Health Insurance Enrollment Program among Residents at Debre Markos Town, 2024. HSOA J Community Med Public Health Care 12: 164.
Copyright: © 2025 Birhanu Manaye, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

