
Determinants of Oral Health Problems among Community-Living Elderly Persons in Greece - The Role of Diet and Chronic Diseases in Oral Health
*Corresponding Author(s):
Konstantopoulou SDepartment Of Public Health Policy, University Of West Attica, 196 Alexandras Avenue, Athens, 11521, Greece
Tel:+30 6973302839,
Email:skonstantopoulou@uniwa.gr
Abstract
Several studies have examined the relationship between oral health, diet and chronic diseases. The aim of the present study was to investigate the determinants of oral health problems, and more particularly to examine the association of diet and chronic diseases with oral health among community living elderly persons in Greece. This cross-sectional study was conducted at 5 Open Protection Centers for the Elderly (O.P.C.E.) of the Municipality of Iraklion, Attica. 156 people participated in the study. They completed a questionnaire and underwent a clinical dental examination that was performed with frontal lightning in a specially designed space provided by the O.P.C.E. The statistical analysis of the data was undertaken by the SPSS program. Study data revealed that 31,4% of participants were significantly affected by the financial crisis concerning their food choices. Men were 68% less likely to go to the dentist once a year. As the age increased, the participants’ chances of going to the dentist once a year decreased. Hypertensive participants were 61% less likely to develop periodontitis than non-hypertensive participants. The more often the participants used to eat fatty food and red meat, the less likely they were to develop periodontitis. Those who consumed more carbohydrates were 51,9% more likely to develop periodontitis than those who consumed smaller amounts of them (34%). According to these findings, the financial situation, the existence of hypertension and the macronutrients content of foods (carbohydrates, fats), were associated with oral health in the elderly.
Keywords
Chronic diseases; Elderly; Diet; Nutrition; Oral health
Introduction
The elderly are the fastest growing population group worldwide [1]. In Greece those who have reached the age of 65 are classified as elderly [2]. According to the Hellenic Statistical Authority the elderly in Greece have reached the number of 2.407.856 people (23% of the Greek population) [3]. Better access to health services and better healthcare are associated with increased average life expectancy [4], but at the same time the prevalence of chronic diseases, such as cardiovascular diseases, chronic lung diseases, cancer, dementia and diabetes mellitus is also increasing [5]. These diseases, also known as “non communicable diseases, NCDs”, have an increased prevalence among the elderly and are the main causes of disability and death [5]. The increase in the elderly population is an issue of increasing interest in the context of Public Health and it has a strong impact on the design of Public Health Policies. Prevention and health promotion strategies are known to improve the quality of life of the elderly [6].
The mouth is often characterized as the mirror of general health, which indicates that oral health is an integral part of health in our body [7]. In the elderly, poor oral health appears to be a risk factor for general health problems [8]. On the other hand, the elderly are more vulnerable to the occurrence of dental diseases, due to the increase in the incidence of chronic diseases on one hand and the impairment of physical and mental function on the other [9]. For these reasons, the elderly from a Public Health perspective are a distinct group as regards planning of dental care and prevention strategies. A healthy diet is one of the most important factors in maintaining health, functional independence and quality of life in the elderly [10]. The protective role of diet against tooth decay and periodontal disease, as well as other chronic diseases, is well established [11]. It has been estimated that oral diseases affect nearly 3.5 billion people. Tooth decay is the most common oral health problem, affecting 2 billion people. On the other hand, periodontal disease affects 14% of the global adult population [12].
Oral disease occurs more often in old age, with common findings being the total lack of natural teeth or partial dentition, molar and root caries, periodontal disease, various pathological damage to the oral cavity and dry mouth [2]. The percentages of total and partial dentition in many foreign countries vary, while in Greece the percentages are 31.5% for the total lack of natural teeth and 23.1% for partial dentition [2]. Root caries is particular common in the elderly. The reason for its development is the subsidence of gums and the exposure of teeth roots to unhealthy oral environment, something that often happens to the elderly [2]. In Greece, root decay was estimated to be approximately 42.7%. As regards periodontitis, severe periodontitis affects 15% of the population in foreign countries, while average periodontitis affects 50% of the population [2]. As regards Greece, 44.5% of the population has mild periodontitis (periodontal pockets of 4-5mm depth), while 15.4% of the population had average periodontitis (periodontal pockets≥6mm) [2].
Malnutrition is a common problem in old age and the risk of malnutrition increases with age. The age-related decrease in food intake combined with the presence of many diseases, use of medications, social isolation, financial constraints, health disorders and multiple hospital admissions complicate the nutritional balance in the elderly [13]. The assessment of the malnutrition risk is very important, in order to design and implement early interventions, as regards the nutrition of the elderly [14]. Taking the above into account, the aim of the study was to investigate the relationship between dietary habits, nutritional status, chronic diseases and the occurrence of oral health problems in the elderly. Furthermore, the study aimed to examine economic situation in our country, which was the effect of the economic crisis during the period 2007-2015 on the food choices and oral health. At the best of our knowledge no other similar studies have been carried out in Greece at the time of the present research.
Methods
Participants and procedures
The present cross-sectional study was carried out in 5 O.P.C.E.s (Open Protection Centers for the Elderly) of the Municipality of Heraklion, Attica. A total number of 161 elderly, active members of O.P.C.E., self-cared, non bedridden and able to communicate and to give informed consent participated in the study. 4 participants did not complete the questionnaire and were excluded from the sample used in the statistical analysis, which ultimately consists of 156 people aged > 65 years old. The study has been carried out in accordance with The Declaration of Helsinki. Written informed consent was obtained by all the study participants prior to their enrollment in the study.
The study questionnaire included three sections regarding: Socio-demographic characteristics, medical and dental history, eating habits and nutritional status. MNA questionnaire was used to investigate the nutritional status of the elderly. The miniMNA (Mini Nutritional Assessment) is a Nutritional adequacy control system. The miniMNA is a short questionnaire developed to assess nutritional status in the population and specifically to detect individuals risk for malnutrition. The main MNA target is the institutionalized elderly. It includes simple and easily extractable parameters. Depending on the answers, a score is given for each of the questionnaire parameters. The sum of the individual scores gives the mini MNA score, which categorizes patients into three categories. a. Score 12-14: normal nutritional status, b. Score 8-11: at risk for malnutrition (marginal), c. Score 0-7: malnourished participants [14-16]. MNA’s sensitivity, specificity and positive predictive value have been determined at 96%, 98% and 97% respectively, when compared with malnutrition as defined by clinicians using other methods [14-16].
In order to evaluate the participants’ body weight, Body Mass Index (BMI) was used, which is calculated by dividing the person’s weight in kilograms to the height square in meters [17]. Participants reported their own height and weight. Distribution of participants according to their BMI has been made using WHO recommendations. More specifically, obese adults are considered those whose BMI is ≥30, overweight those whose BMI is 25-29,99, normoweight those whose BMI is 18,5-24,99 and underweight when BMI is < 18,5 [18].
Furthermore, a clinical dental examination has been performed, with the participants in a sitting position and the help of frontal lightning. The use of common commercial frontal lightning was found to be adequate in practice, tested before use on control patient participants and compared with actual dental lightning in real dental office conditions. For the examination of the participants, the recommended diagnostic set of dental tools (mirror, probe, cochlear, cotton tweezers) was used, as well as a personal disposable dental towel. Based on the clinical examination, a short record was made for the presence or the absence of periodontitis in some teeth and indicators such as bleeding on probing, periodontal probing depth, clinical attachment loss. According to the European Federation of Periodontology (EFP) and the American Academy of Periodontology (AAP) in 2018 (EFP/AAP) periodontitis is the mouth disease characterized by clinical attachment loss (CAL) ≥2 adjacent teeth, buccal CAL ≥3mm, Periodontal Probing Depth (PPD) >3mm at ≥2 adjacent teeth. As regards the severity of periodontitis, attachment loss 1-2mm is characterized as mild, attachment loss 3-4 mm is characterized as moderate while attachment loss ≥5mm is characterized as severe [19]. In our research there was not a clear grading of periodontitis into mild, moderate and severe. However, the clinical examination led to useful conclusions.
Statistical analysis
Statistical analysis was performed through SPSS version 18.0. Graphs and tables are generated with Microsoft Word and Excel program. For quantitative variables, results were expressed as means ± S.D., and/or medians and interquartile ranges. For qualitative variables, results were expressed as absolute values (N) and percentages (%). Comparisons of quantitative variables between two groups were performed using Student`s “t” test or the non parametric Mann-Whitney for continuous variables. Pearson`s x2 test or Fisher’s exact test were used to compare categorical variables. Parametric Analysis of Variance (ANOVA) was used to compare quantitative variables between more than two groups. Pearson’s or Spearman’s correlation coefficient was used to test the relationship between two quantitative variables (r). Correlation is considered low when the correlation coefficient (r) ranges from to 0.1 to 0.3, moderate when the correlation coefficient ranges from 0.31 to 0.5 and high when the coefficient is greater than 0.5. In order to find the independent factors related to the frequent visit to the dentist, the existence of periodontitis, a logistic regression analysis was performed with the stepwise inclusion/removal procedure. The relative ratios (Odds ratio) were obtained with 95% confidence intervals (95%Cl). Significance levels are two-sided and statistical significance was set at 0.05.
Results
The sample consisted of 156 people with an average age of 75.9 years (±7.6 years). 51.9% of participants were male. 66.0% of the participants were married and 26.3% were widowed. Almost all participants were Greek (97.4%). Most of the participants (71.8%) have completed the elementary school, while 17.9% have completed the high school. About half of the participants (48.1%) declared to have a moderate financial situation, while 50.0% of the participants declared that they experienced high/or very high impact of the crisis on their financial situation. Finally, 31.4% of participants were quite affected by the financial crisis as regards the food choices, while 37.8% were not affected at all (Table 1).
|
|
N |
% |
|
|
Gender |
Women |
75 |
48,1 |
|
Men |
81 |
51,9 |
|
|
Age (mean value±SD) |
75,9±7,6 |
|
|
|
Family status |
Non married |
4 |
2,6 |
|
Married |
103 |
66,0 |
|
|
Divorced |
8 |
5,1 |
|
|
Widowers |
41 |
26,3 |
|
|
Educational level |
Illeterate |
1 |
0,6 |
|
Elementary School |
112 |
71,8 |
|
|
High School |
28 |
17,9 |
|
|
Technological Education |
3 |
1,9 |
|
|
University Education |
12 |
7,7 |
|
|
Economic Situation |
Bad |
58 |
37,2 |
|
Moderate |
75 |
48,1 |
|
|
Good |
23 |
14,7 |
|
|
Influence of the crisis on the financial situation |
Not at all |
18 |
11,5 |
|
A little |
16 |
10,3 |
|
|
Enough |
44 |
28,2 |
|
|
Very |
53 |
34,0 |
|
|
Very much |
25 |
16,0 |
|
|
Influence of the crisis on the food choice |
Not at all |
59 |
37,8 |
|
Little |
25 |
16,0 |
|
|
Enough |
49 |
31,4 |
|
|
Very |
12 |
7,7 |
|
|
Very much |
11 |
7,1 |
|
|
BMI ( average 28.1±3.9) |
<18,5 18,5-24,99 25-29,99 >30 |
1 32 79 44 |
0.6 20,5 50,6 28,2 |
|
Mini MNA score |
Normal In danger of undernutrition Undernutrition |
124 28
4 |
79.5 17.9
2.6 |
|
How often do you brush your teeth? |
Never Occasionally Once a day More than once a day |
14 11 56 44 |
11.2 8.8 44.8 35.2 |
|
Do you consume fruits daily? |
|
141 |
90.4 |
|
Do you consume raw vegetables daily? |
|
127 |
81.4 |
|
Between meals do you use to consume sugary drinks, beverages and soft drinks? |
|
84 |
53.8 |
Table 1: Demographic distribution, BMI. MNA score, oral care, eating habits of participants.
Regarding the use of dental health services and the participants’ attitudes towards the preservation of natural teeth, 41% of the participants have never visited a dentist, while 26.3% only visit them when they feel tooth-pain. On the other hand, 96.8% of the participants believe that it is important to preserve natural teeth as much as possible (Shown in Table 2 and Figure 1).
|
|
How often do you visit a dentist? |
P Pearson's x2 test |
||||
|
Never/ In case of pain |
At least once a year |
|
||||
|
Ν |
% |
Ν |
% |
|
||
|
Gender |
Women |
40 |
53,3 |
35 |
46,7 |
<0,001 |
|
Men |
65 |
80,2 |
16 |
19,8 |
|
|
|
Age, average±SD |
|
77,2±7,7 |
|
73,2±6,8 |
|
0,002* |
Table 2: Frequency of visits to the dentist in relation to the demographic characteristics of the participants.
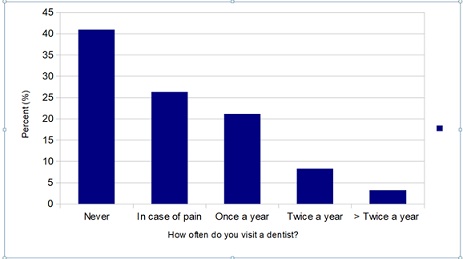
Figure 1: Frequency of visits of the participants to the dentist.
Regarding the participants’ dental hygiene habits, 11.2% never brush their teeth and 8.8% brush their teeth occasionally (Table 1). Concerning eating habits, 90.4% consume fruits and 81.4% consume raw vegetables daily. Also, 51.4% of participants consume often sugary drinks and soft drinks between meals. Regarding the participants’ nutritional status, according to the mini MNA score, 79.5% were found to have a healthy nutritional status, 17.9% were at risk for malnutrition and 2.6% suffered from malnutrition (Table 1). The average BMI of the participants was 28.1 (±3.9). In particular, 0.6% of the participants had BMI<18,5, 20,5% of the participants had BMI 18,5-24,99, 50,6% had BMI 25-29,99, while 28,25% of the participants had BMI≥30 (Table 1).
Women were significantly more likely to visit the dentist at least once a year compared to men (shown in Figure 2 and Table 2). Also, participants who used to visit the dentist at least once a year were significantly younger compared to participants who went less often (Shown in Table 2). A multivariate logistic regression was performed using as dependent variable the frequent visit to the dentist (at least once a year) and as independent variables the participants’ demographic characteristics. Using the method of sequential inclusion /removal, it was found that gender and age are related to the frequent visit at the dentist. Specifically:
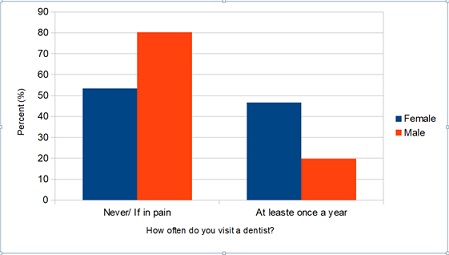 Figure 2: Distribution of frequency of visits to the dentist by gender.
Figure 2: Distribution of frequency of visits to the dentist by gender.
Men were 68% less likely than women to visit the dentist at least once a year. As age increased, participants were less likely to visit the dentist at least once a year (Table 3)
|
|
|
OR (95% CI)‡ |
P |
|
Gender |
Women |
1,00* |
|
|
|
Men |
0,32 (0,16 - 0,67) |
0,002 |
|
Age |
|
0,94 (0,9 - 0,99) |
0,016 |
Table 3: Correlation of gender and age with the frequency of visits to the dentist.
- Correlation of the presence of periodontitis with demographic, clinical and nutritional characteristics of the participants
Among the edentulous participants, periodontitis was found in 41.6% of the participants. As shown in table 3, participants who suffered from periodontitis had significantly lower BMI compared to participants without periodontitis. No differences were found in the rates of periodontitis in relation to the other parameters in the table 3. As shown in figure 3, the rate of periodontitis was significantly lower in hypertensive participants or persons who were treated for hypertension compared to participants who did not suffer from hypertension or were not treated for hypertension.
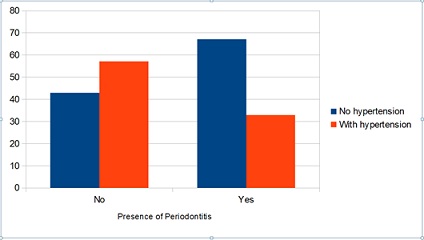 Figure 3: Rates of periodontitis according to the presence of hypertension.
Figure 3: Rates of periodontitis according to the presence of hypertension.
Periodontitis’ rates were significantly higher among the participants who consumed carbohydrates daily compared to the participants who consumed carbohydrates less often. Also, participants with periodontitis consumed less red meat and fatty foods weekly compared to participants without periodontitis (Table 4). Furthermore, a multivariate logistic regression was performed with the existence of periodontitis among the edentulous participants as dependent variable and the demographic, clinical and nutritional characteristics as independent variables; using the method of sequential inclusion/removal, the results shown in table 5 were found.
|
|
Presence of periodontitis |
P Pearson's x2 test |
||||
|
No |
Yes |
|||||
|
Ν |
% |
Ν |
% |
|||
|
Gender |
Women |
38 |
58,5 |
27 |
41,5 |
0,988 |
|
Men |
35 |
58,3 |
25 |
41,7 |
|
|
|
Ηλικiα, μεση τιμη±SD |
|
75,2±6,5 |
|
74,1±8,7 |
|
0,434* |
|
Married |
No |
25 |
61,0 |
16 |
39,0 |
0,683 |
|
Yes |
48 |
57,1 |
36 |
42,9 |
|
|
|
Educational level |
Up to Elementary School |
49 |
58,3 |
35 |
41,7 |
0,983 |
|
At least High School |
24 |
58,5 |
17 |
41,5 |
|
|
|
Financial situation, mean±SD median (interquartile range) |
0,7±0,6 |
1 (0 - 1) |
0,8±0,7 |
1 (0 - 1) |
0,486** |
|
|
Impact of the crisis on the food choices, mean±SD median (interquartile range) |
2,5±1 |
3 (2 - 3) |
2,2±1,2 |
2 (2 - 3) |
0,193** |
|
|
Επíδραση οικονομικης κρíσης στην επιλογη τροφíμων, μεση τιμη±SD διαμεσος (ενδ. ενρος) |
1,2±1,1 |
1 (0 - 2) |
1,2±1,3 |
1 (0 - 2) |
0,975** |
|
|
ΒΜΙ, mean value±SD |
29±3,9 |
|
27,1±4 |
|
0,009* |
|
|
Smoking |
No/Former Smoker |
65 |
60,7 |
42 |
39,3 |
0,194 |
|
Yes |
8 |
44,4 |
10 |
55,6 |
|
|
|
Frequency of alcohol consumption |
Up to 1 drink a month |
38 |
56,7 |
29 |
43,3 |
0,884 |
|
Up to 3 drinks a week |
15 |
62,5 |
9 |
37,5 |
|
|
|
>=2 drinks a day |
20 |
58,8 |
14 |
41,2 |
|
|
|
Do you believe that you have stress? |
No |
20 |
60,6 |
13 |
39,4 |
0,764 |
|
Yes |
53 |
57,6 |
39 |
42,4 |
|
|
|
Do you consume carbohydrates daily? |
No |
48 |
65.8 |
25 |
34,2 |
0,048 |
|
|
Yes |
25 |
48.1 |
27 |
51,9 |
|
|
How often do you consume red meat? mean ±SD median(interquartile range) |
|
2±0,7 |
2(2-2) |
1,7±0,8 |
2(2-2) |
0,049** |
|
How often do you consume fatty food? mean±SD median(interquartile range) |
|
0,9±1,2 |
1 (0-1) |
0,5±1 |
0 (0-1) |
0,010** |
Table 4: Correlation of periodontitis with demographic characteristics, financial situation, daily habits, stress and eating habits of the participants.
*Student’s t-test
**Mann Whitney test
|
|
|
OR (95% CI)‡
|
P
|
|
Hypertension |
No |
1,00* |
|
|
Yes |
0,39 (0,18 - 0,88) |
0,023 |
|
|
How often do you consume fatty food? |
0,63 (0,42 - 0,94) |
0,023 |
|
Table 5: Association of periodontitis with hypertension and fatty foods consumption.
± Odds Ratio (95% Confidence Interval)
*indicates reference class
Hypertension and the frequency of fatty foods consumption by the participants were found to be associated with the presence of periodontitis. More specifically:
- Hypertensive participants were 61% less likely to develop periodontitis compared to participants without hypertension
- The more often the participants consumed fatty foods, the less likely they were to develop periodontitis (Table 5)
Discussion
Recent decades have brought a significant shift in population demography worldwide and many countries record significant increases in life expectancy. The percentage of elderly people is increasing, as well as the chronic diseases that accompany them. Chronic diseases include oral health problems, such as caries and periodontitis, while caries is considered to be the most frequent chronic disease worldwide [12]. In the present study, which was conducted at the Open Protection Centers of the Elderly of Municipality of Heraklion, Attica, the determinants of oral health among community living elderly were investigated. In particular, the relationship between the dietary habits and indicators of oral health in the elderly population has been examined.
50% of the participants were affected by the crisis in terms of their financial situation, 31.4% had been affected enough by the crisis in terms of food choices, while 37.8% were not affected at all. These data quite agree with the findings from the international literature regarding the effect of the economic situation and the financial crisis on the food choices as regards the elderly. A study concluded that the elderly, who are in the stage of retirement, are not influenced by the cost when it involves food choices [20]. Also, in another research aiming to study the purchasing behaviour of the elderly, it was concluded that elderly persons are mostly interested in the transition in their lives, from the working to retirement status, as well as the technological progress, which they find difficult to follow [21]. Concerning the impact of the financial crisis to the food choices during the financial crisis in Greece, a research found that during austerity men were overweight and obese to a higher percentage and consumed red meat and fast food more often compared to women. Also, women were more influenced by the cost as regards the healthy food choices [22]. Another research conducted during the financial crisis in Greece, revealed that Greek people, because of the stress caused by the financial crisis, were not interested in their health status, while unhealthy eating habits increased [23].
The rate of malnutrition was found lower than in other studies involving a socially active elderly population in Greece, but the percentage of people at risk of malnutrition is significant [24]. More specifically, 28% of the participants were at risk of undernutrition. This comes to an agreement with the findings of an older study which examined the nutritional status of free-living elderly people in Attica, Greece. This study found that 25.8% of the population of the study was at risk of undernutrition [25]. In a study conducted later in another municipality of Attica, involving a socially active elderly population, it was found that 35,8% of the elderly were at risk of undernutrition [24]. According to the results of a study conducted in another Open Protection Center in Attica, 34% of the elderly were at risk of malnutrition [26], while, a study conducted in a health center in a semi-urban suburb of Athens, found that 30,4% of the participants aged >65 were at risk of malnutrition [27]. As regards to their dietary habits, 90.4% of the participants of our study used to consume fruits daily and 81.4% of the participants consumed raw vegetables daily, percentages that, based on national and international guidelines, might indicate partly healthy dietary habits [28]. However, 53.8% of the participants were found to consume often sugary drinks, beverages and soft drinks between meals. So, they have also unhealthy eating habits, which may lead to caries development [28]. According to the study conducted in a socially active population living in a semi-urban suburb of Athens, the adherence to the Mediterranean diet was found moderate, while the consumption of fruits and vegetables was influenced by the number of posterior teeth, as well as the posterior occlusion of the teeth [27].
41% of the participants had never visited a dentist or had stopped visiting him (especially edentulous patients), while 26.3% visited a dentist only when they felt tooth pain. These percentages seem to agree with studies conducted both in developing [29] and in developed [30] countries, which shows that at least in terms of dental health, the elderly in our country have similar behaviour with elderly populations in other developed countries. Also, 11.2% never brush their teeth, while 8.8% brush their teeth occasionally and 35.2% brush their teeth more than once a day. In other words, one in five seniors does not practice daily oral hygiene. This percentage is lower than that reported in developing countries [31,32]. However, compared with developed countries, it was found that Greek elderly have worse tooth brushing behaviour. In particular, in a study conducted by Wright et al., in 2019 in an effort to study the oral health behaviour of elderly Australian men, it was found that 59.3% brushed their teeth twice or more times per day [33]. Among the participants the presence of periodontitis was found to be 41.6%. The percentage was higher than that of developed countries [1], but lower than that of developing countries [34].
Participants with periodontitis had a significantly lower BMI compared to participants without periodontitis, probably because of the difficulty in chewing several foods; this is a finding that in some cases does not agree with international literature data [35-37], while in other studies the results are contradictory [38,39]. It is worth noting that the rate of periodontitis was significantly lower in those who suffered from hypertension or were receiving medication for hypertension, perhaps because hypertensives pay more attention to their diet, but these findings do not agree with the international literature [40-42]. Hypertension and the frequency of consumption of fatty foods are both related to the presence of periodontitis. Hypertensive participants were 61% less likely to develop periodontitis compared to participants without hypertension.
Also, the more often the participants consumed fatty foods, the lower was the possibility to develop periodontitis, which is in agreement with international literature data [43,44]. This is probably explained by the replacement of carbohydrates, that negatively affect periodontal tissues, with fatty food. The negative effect of carbohydrates on periodontitis [45-47] also emerges in the present research, since it appears that those who consume more carbohydrates are 51.9% more likely to develop periodontitis than those who consume less carbohydrates (34.2%). The finding of the present study that the consumption of red meat has a positive effect on periodontitis is in line with other studies [48], while some studies support the opposite [49,50]. Men were found to be 68% less likely to visit the dentist compared to women. This finding is in agreement with the findings of other researchers [51], while some studies support that women visit dentists less often [52-54]. Also, as age increases, participants are less likely to visit a dentist at least once a year [48,50,51]. This could be explained by the increase in visits to other medical specialties, which implies the increase in the frequency of other chronic diseases and the reduction of teeth due to extractions with advancing age, but also by the earlier established dental profile of the elderly [55,56].
Limitations of the study include the cross-sectional nature of the study, which does not allow causal relationships to be identified, the relatively small sample size, which originates from only one suburb of Athens, which does not permit the generalization of the results. Also, height and weight were self-reported and not measured, which may cause a significant bias.
Proposals
According to the Ministry of Health in Greece, Public Health should have 4 main targets:
- Primary Prevention: National Programme for the promotion of physical activity and healthy nutrition, National alcohol treatment programme, National Programme for the vaccination of vulnerable population groups
- Secondary Prevention: National Screening Programme Control in the general population. National systematic antenatal and perinatal programme
- Tertiary Prevention: a. National Psychosocial Integration Programme and Rehabilitation for people with severe psychosocial problems. b. Palliative care for cancer patients
- Modernization of the Public Health System [57]
In terms of Public Health regarding the oral health, the primary preventive measures are the use of fluoride (toothpaste), toothbrushing, the use of interdental cleaning [58-61] and the fluoridation of drinking water [58,62-64]. The use of oral solutions, especially those containing chlorhexidine, may be recommended when the elderly suffer from dry mouth, but in no case this can replace toothbrushing [59].
From a nutritional point of view, the general guideline for maintaining oral hygiene is to moderate or avoid the intake of added sugars and sweeteners [59]. More specific measures are: a) the adherence to a diet rich in whole grain products, fruits and vegetables, which stimulate saliva production, along with the use of fluoride toothpaste [50,58,65], b) the consumption of protective food combinations (such as consumption of dairy products, and sugar-free chewing gum (especially that containing xylitol) [58,65], c) the consumption of refined carbohydrates and sugary drinks with meals to neutralize acids [58], d) the consumption, after the meals, of sugar-free chewing gum or cheese or even rinsing the mouth with water [58,65], e) the use of chewing sugar-free gum between meals, which increases saliva production [58,65], f) drinking rather than sipping of sweet and sour drinks (in order to reduce the exposure of the teeth [58], g) modification of the frequency of meals in order to reduce the frequency of exposure to sugars [58,65] and h) careful reading of the food labels, so that the sugar content can be noticed [66]. At the same time, the elderly must be encouraged to increase physical activity, to consume dairy products and to adapt an overall healthy lifestyle [67].
On the other hand, dentists should be trained towards the direction of nutritional counseling. During the preventive dental check-up, they should give instructions to their patients, so that they may reduce the risk of oral diseases and promote oral health. Any changes that need to be made should be analyzed in a simple and comprehensive way and realistic goals should be set, taking into account the individual, educational and cultural characteristics of the elderly [66,67], as well as their financial situation, which, to a significant extent, influence the food choices. It is obvious that elderly people with other health problems should consult specialist doctors and/or a dietitian [67]. Moreover, doctors of other specialties should contribute so as to raise the awareness of the elderly concerning oral health. In particular, primary care physicians need to be educated on the medical, functional, psychological and social implications of oral diseases and collaborate with dentists so as to provide regular screening and education about dental diseases [68-70].
In addition, national policies and strategies for oral health are required. Firstly, there should be provision for the dental care for the elderly, especially those dependent on others, and secondly, the creation of similar programs for the younger persons is very important [71]. Also, there should be educational programs, in which the elderly may be informed about the importance of preserving natural teeth and would be given oral health instructions. In the same direction, proposals regarding the prevention of oral diseases in the elderly could also be the following: a) Dentists and nutritionists should be permanent staff of O.P.C.E., even on a voluntary basis; they should work closely together to achieve the best result for the maintenance of oral and general health, b) Contracts should be established for dentists with insurance funds and especially with the National Organization for the Provision of Health Services, which is the main insurance institution in Greece, so that access to dental care will be possible even for those who avoid dental treatment for financial reasons, which represent a large part of the population and c) Each Municipality should establish some free days of dental care for the poorer and financially deprived.
In Greece, the state of being edentulous is included in the 10 main causes of disability. The percentage of the greek population with unsatisfied dental care needs has increased from 5.8% in 2008 to 8.8% in 2019. As strategic priorities for the promotion of Oral Health are proposed:
- The inclusion of dental care in universal health coverage and the reduction of inequalities in oral health
- The epidemiological monitoring of the oral health of the population and the social determinants that influence it
- The promotion of oral health literacy
- The integration of the promotion of oral health in educational programs by public health practitioners
- The intervention in the commercial determinants of the sector
The promotion of the use of fluoride through informing the population, as well as the reduction of sugar consumption and use of tobacco [72]
Conclusion
Among the participants of the present cross-sectional study 50.0% have experienced high/very high impact of the economic crisis on their financial situation, while 31.4% of participants were quite affected by the financial crisis as regards the food choices, 17.9% of the participants were at risk for malnutrition and 2.6% suffered from malnutrition. The majority of the participants used to eat fruits and raw vegetables daily. More than half of the participants used to drink sugary and soft drinks between meals. The elderly participants of the study do not visit a dentist regularly for the prevention of oral health problems, nor practice systematically oral health hygiene measures. Periodontitis was present among the 41,6% of the sample. A negative association of age and male gender was found with the frequency of visits to a dentist. Furthermore, hypertension, less frequent consumption of fatty foods and red meat on a weekly basis and daily consumption of carbohydrate-rich foods are more prevalent among elderly persons with periodontitis. Participants who suffered from periodontitis had a significantly lower BMI compared to participants who did not have periodontitis. As the elderly form a constantly increasing population group, it is important to emphasise on the design and the implementation of policies aiming to prevent nutrition related diseases, including oral health problems, and to promote overall health and quality of life.
Author Contributions
All authors have contributed equally to the article. All authors read and approved the final manuscript for submission.
Acknowledgment
The authors wish to thank the President of Preschool Education and Social Care, who approved the implementation of the research, as well as the staff of the Centers of Open Protection of Heraklion, Attica, without the help of whom, the research wouldn’t have been completed.
Funding
This study did not receive any direct funding.
Disclosure of Interest
The Authors declares that there is no conflict of interest.
Availability of Data and Materials
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the President of Preschool Education and Social Care in Municipality of Heraklion, Attica.
Informed Consent Statement
Informed consent was obtained in written form from all participants in the study.
Conflict of Interest Statement
There was no conflict of interest.
References
- United Nations (2019) World Population Ageing 2019: Highlights. United Nations, New York, USA.
- Kossioni AE (2018) Gerodontology (1stedn). Athens. Greece.
- Hellenic Statistical Authority (2021) 2021 Population-Housing Census. Hellenic Statistical Authority, Athens, Greece.
- Hao L, Xu X, Dupre ME, Guo A, Zhang X, et al. (2020) Adequate access to healthcare and added life expectancy among older adults in China. BMC Geriatrics 20: 129.
- Hayat C, Stein E (2018) The Global burden of multiple chronic conditions: A narrative review. Prev Med Rep 12: 284-293.
- Fulmer T, Reuben DB, Auerbach J, Fick DM, Galambos C, et al. (2021) Actualizing Better Health And Health Care For Older Adults. Health Aff (Millwood) 40: 219-225.
- Ofili DFC, Esu EB, Ejemot-Nwadiaro RI (2020) Oral hygiene practices and utilization of oral healthcare services among in-school adolescents in Calabar, Cross River State, Nigeria. Pan Afr Med J 36: 300.
- Wong FMF, Ng YTY, Leung WK (2019) Oral Health and Its Associated Factors Among Older Institutionalized Residents-A Systematic Review. Int J Environ Res Public Health 16: 4132.
- Chan AKT, Tamrakar M, Jiang CM, Lo ECM, Leung KCM, et al. (2021) Common Medical and Dental Problems of Older Adults: A Narrative Review. Geriatrics 6: 76.
- Govindaraju T, Sahle BW, McCaffrey TA, McNeil JJ, Owen AJ (2018) Dietary Patterns and Quality of Life in Older Adults: A Systematic Review. Nutrients 10: 971.
- World Health Organization (2022) Factsheet on oral health and sugars intake. WHO, Geneva, Switzerland.
- World Health Organization (2022) Oral Health. WHO, Geneva, Switzerland.
- Kiessweter E, Colombo M, Meisinger C, Peters A, Thorand B, et al. (2018) Malnutrition and related risk factors in older adults from different health-care settings: an enable study. Public Health Nutr 23: 446-456.
- Serón-Arbeloa C, Labarta-Monzón L, Puzo-Foncillas J, Mallor-Bonet T, Lafita-López A, et al. (2022) Malnutrition Screening and Assessment. Nutrients 14: 2392.
- Soysal P, Veronese N, Arik F, Kalan U, Smith L, et al. (2019) Mini Nutritional Assessment Scale-Short Form can be useful for frailty screening in older adults. Clin Interv Aging 14: 693-699.
- Montejano Lozoya R, Martínez-Alzamora N, Clemente Marín G, Guirao-Goris SJA, Ferrer-Diego RM (2017) Predictive ability of the Mini Nutritional Assessment Short Form (MNA-SF) in a free-living elderly population: A cross-sectional study. Peer J 18: 3345.
- Fusteris E (2017) Newer data on obesity. Scientific Chronicles 22: 106-116.
- World Health Organization (2022) Body mass index (BMI). WHO, Geneva, Switzerland.
- Botelho J, Machado V, Proenca L, Mendes JJ (2020) The 2018 periodontitis case definition improves accuracy performance of full-mouth partial diagnostic protocols. Sci Rep 10: 7093.
- Conklin A, Monsivais P (2013) Economic Determinants of Diet in Older Adults. In: Raars MM, de Groot L (eds.). Food for the Aging Population (2ndedn). Woodhead Publishing, UK.
- Alhammadi K, Santos-Roldán L, Cabeza-Ramírez LJ (2021) A Theoretical Framework on the Determinants of Food Purchasing Behavior of the Elderly: A Bibliometric Review with Scientific Mapping in Web of Science. Foods 10: 688.
- Koulierakis G, Dermatis A, Vassilakou T, Pavi E, Zavras D, et al. (2021) Determinants of healthy diet choices during austerity in Greece. British Food Journal 124: 2893-2910.
- Panagiotakos DB, Pitsavos C, Athyros V, Goudevenos G, Vassilakou T, et al. (2013) Attitudes and beliefs towards cardiovascular disease prevention in relation to the financial crisis: a longitudinal study (2006-2012) in Greece. European Heart Journal 34: 469.
- Plexida A, Vasilakou T, Kampa E, Fasoi G, Kelesi M, et al. (2015) Status assessment nutrition of the elderly in Open Care Centers and correlation of the nutrition index with socioeconomic variables and
health indicators. Archives of Hellenic Medicine 32: 622-628. - Vassilakou T, Triantafyllou G, Evrenoglou L (2017) Early identification of Malnutrition Risk Among Free-Living Elderly Persons In Athens, Greece. Journal of Aging Research & Clinical Practice 6: 193-199.
- Arvanitaki E, Vasilakou T (2022) Assessment of the nutritional status of elderly people attending the Open Care Centers in the Municipality of Keratsini-Drapetsona, and correlation with socio economic
status and health indicators. Archives of Hellenic Medicine 39: 72-81. - Kartsintaki M (2022) Association between oral health status, nutrition intake and nutrition status among patients of Markopoulos Health Center. Master’s Thesis, MSc in Public Health, Dept. Of Public Health Policy, University of West Attica, Athens, Greece.
- Nicklett EJ, Kadell AR (2013) Fruit and vegetable intake among older adults: a scoping review. Maturitas 75: 305-312.
- Patro BK, Ravi Kumar B, Goswami A, Mathur VP, Nongkynrih B (2008) Prevalence of dental caries among adults and elderly in an urban resettlement colony of New Delhi. Indian J Dent Res 19: 95-98.
- Ebbens OEJ, Lawant MJ, Schuller AA (2018) [Dental visits among people over 65; a study in a general dental clinic in Drenthe, the Netherlands]. Ned Tijdschr Tandheelkd 125: 151-155.
- Aguirre Escobar GA, de Quezada RF, Escobar de González WY, Aguirre de Rodríguez KA, de Miguel ÁG, et al. (2022) Oral health profile status and treatment needs in the Salvadoran elderly population: A cross-sectional study. BMC Oral Health 22: 247.
- Oliveira MB, Lopes FF, Rodrigues VP, Alves CMC, Hugo FN (2018) Association between socioeconomic factors, behavioral, general health and oral mucosa status in elderly. Cien Saude Colet 23: 3663-3664.
- Tran J, Wright F, Takara S, Shu CC, Chu SY, et al. (2019) Oral health behaviours of older Australian men: the Concord Health and Ageing in Men Project. Aust Dent J 64: 246-255.
- Janakiram C, Mehta A, Venkitachalam R (2020) Prevalence of periodontal disease among adults in India: A systematic review and meta-analysis. J Oral Biol Craniofac Res 10: 800-806.
- Suvan J, Petrie A, Moles DR, Nibali L, Patel K, et al. (2014) Body Mass Index as a Predictive Factor of Periodontal Therapy Outcomes. J Dent Res 93: 49-54.
- Tolle SL, Newcomb TL, Conover J (2018) The Relationship Between Obesity and Periodontal Diseases. Dimensions of Dental Hygiene 16: 54-57.
- Hirschfeld J, Chapple ILC (2021) Periodontitis and Systemic Diseases. Clinical Evidence and Biological Plausibility (1stedn). Quintessence Publishing, Germany.
- Gerber FA, Sahrmann P, Schmidlin OA, Heumann C, Beer JH, et al. (2016) Influence of obesity on the outcome of non-surgical periodontal therapy - a systematic review. BMC Oral Health 16: 90.
- Tahir K, Malek AH, Vaithilingam RD, Saub R, Safii SH, et al (2020) Impact of non-surgical periodontal therapy on serum Resistin and periodontal pathogen in periodontitis patients with obesity. BMC Oral Health 20: 52.
- Zhao MJ, Qiao YX, Wu L, Huang Q, Li BH, et al. (2019) Periodontal disease is associated with increased risk of hypertension: A cross-sectional study. Front Physiol 10: 440.
- Czesnikiewicz-Guzik M, Osmenda G, Siedlinski M, Nosalski R, Pelka P, et al (2019) Causal association between periodontitis and hypertension: evidence from Mendelian randomization and a randomized controlled trial of non-surgical periodontal therapy. Eur Heart J 40: 3459-3470.
- Gordon JH, LaMonte MJ, Zhao J, Genco RJ, Cimato TR, et al. (2019) Association of Periodontal Disease and Edentulism With Hypertension Risk in Postmenopausal Women. Am J Hypertens 32: 193-201.
- Santonocito S, Polizzi A, Palazzo G, Indelicato F, Isola G (2021) Dietary Factors Affecting the Prevalence and Impact of Periodontal Disease. Clin Cosmet Investig Dent 13: 283-292.
- Martinon P, Fraticelli L, Giboreau A, Dussart C, Bourgeois D, et al. (2021) Nutrition as a key Modifiable Factor for Periodontitis and Main Chronic Diseases. J Clin Med 10: 197.
- Millen AE, Dahhan R, Freudenheim JL, Hovey KM, Li L, et al. (2022) Dietary carbohydrate intake is associated with the subgingival plaque oral microbiome abundance and diversity in a cohort of postmenopausal women. Scientific Reports 12: 2643.
- Kocher T, König J, Borgnakke WS, Pink C, Meisel P (2018) Periodontal complications of hyperglycemia/diabetes mellitus: Epidemiologic complexity and clinical challenge. Periodontol 78: 59-97.
- Woelber JP, Bremer K, Vach K, König D, Hellwig E, et al. (2017) An oral health optimized diet can reduce gingival and periodontal inflammation in humans - a randomized controlled pilot study. BMC Oral Health 17: 28.
- Najeeb S, Zafar MS, Khurshid Z, Zohaib S, Almas K (2016) The Role of Nutrition in Periodontal Health: An update. Nutrients 8: 530.
- Salazar CR, Laniado N, Mossavar-Rahmani Y, Borrell LN, Qi Q, et al. (2018) Better-quality diet is associated with lower odds of severe periodontitis in US Hispanics/Latinos. J Clin Periodontol 45: 780-790.
- Martinon P, Fraticelli L, Giboreau A, Dussart C, Bourgeois D, et al. (2021) Nutrition as a key modifiable factor for periodontitis and main chronic diseases. J Clin Med 10: 197.
- Nitschke I, Stillhart A, Kunze J (2015) Utilization of dental services in old age. Swiss Dent J 125: 433-447.
- Eguchi T, Tada M, Shiratori T, Imai M, Onose Y, et al. (2018) Factors Associated with Undergoing Regular Dental Check-ups in Healthy Elderly Individuals. Bull Tokyo Dent Coll 59: 229-236.
- Spinler K, Aarabi G, Valdez R, Kofahi C, Heydecke G, et al. (2019) Prevalence and determinants of dental visits among older adults: findings of a nationally representative longitudinal study. BMC Health Serv Res 19: 590.
- Kramarow EA (2019) Dental Care Among Adults Aged 65 and over, 2017. NCHS Data Brief 337: 1-8.
- Parker ML, Thornton-Evans G, Wei L, Griffin SO (2020) Prevalence of and Changes in Tooth Loss Among Adults Aged ≥50 Years with Selected Chronic Conditions — United States, 1999–2004 and 2011–2016. Morbidity and Mortality Weekly Report (MMWR) 69: 641-646.
- Patel N, Fils-Aime R, Li C-H., Lin M, Robison V (2021) Prevalence of past-year dental visit among US adults aged 50 years or older, with selected chronic diseases, 2018. Preventing Chronic Disease 18: 200576.
- Ministry of Health (2021) National Plan for the Pubic Health. Ministry of Health, USA.
- Poklepovic T, Worthington HV, Johnson TM, Sambunjak D, Imai P, et al. (2019) Interdental brushing for the prevention and control of periodontal diseases and dental caries in adults. Cochrane Database Syst Rev: CD009857.
- Ontario Dental Association (2019) Senior’s Oral Care: Providing oral hygiene care to residents of Ontario long-term care homes. A Guide for personal support workers. Ontario Dental Association, Toronto, Canada.
- Coll PP, Lindsay A, Meng J, Gopalakrishna A, Raghavendra S, et al. (2020) The Prevention of Infections in Older Adults: Oral Health. J Am Geriatr Soc 68: 411-416.
- American Dental Association (ADA) (2019) Aging and Dental Health. ADA, New York, USA.
- American Dental Association (2015) The Benefits of Water Fluoridation for Adults. ADA, New York, USA.
- Welsh F (2018) For Older Adults: It’s Not Too Late to Get Your Fluoride Fix. Water Fluoridation for Healthy Communities, Colorado, USA.
- CDC (2021) Community Water Fluoridation. CDC, Georgia, USA.
- American Dental Association (ADA) (2016) Nutrition and Oral Health. ADA, New York, USA.
- Hayes MJ, Cheng B, Musolino R, Rogers AA (2017) Dietary analysis and nutritional counselling for caries prevention in dental practise: a pilot study. Aust Dent J 62: 485-492.
- Palacios C, Joshipura K, Willett W (2009) Nutrition and Health: Guidelines for dental practitioners. Oral Dis 15: 369-381.
- Arora G, Yeung C (2018) The role of general practitioners in recognising and managing dental disease. Clinical Focus Primary Care 12: 6-13.
- Poudel P, Griffiths R, Wong VW, Arora A, Flack JR, et al. (2020) Perceptions and practices of general practitioners on providing oral health care to people with diabetes - a qualitative study. BMC Fam Pract 21: 34.
- Barnett T, Hoang H, Stuart J, Crocombe L (2017) The relationship of primary care providers to dental practitioners in rural and remote Australia. BMC Health Serv Res 17: 515.
- Edelstein BL, Perkins J, Vargas CM (2020) The Role of Law and Policy in Increasing the Use of the Oral Health Care System and Services. ODPHP, Rockville, USA.
- Bodossaki Foundation (2022) A Roadmap for Public Health in the 21th century. Bodossaki Foundation, Athens, Greece.
Citation: Konstantopoulou S, Vassilakou T (2022) Determinants of Oral Health Problems among Community-Living Elderly Persons in Greece - The Role of Diet and Chronic Diseases in Oral Health. J Gerontol Geriatr Med 8: 145.
Copyright: © 2022 Konstantopoulou S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

