Diabetics-Related Foot Deformity: Prevalence, Risk Factors, Knowledge and Practice
*Corresponding Author(s):
Amenu Tolera WirtuDepartment Of Anatomy, College Of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Email:amannut2002@gmail.com
Abstract
Neuromusculoskeletal functions interplay in maintaining normal gait patterns. Changes in foot posture and architecture are results of diseases. For Instance, diabetes impacts human biomechanics of running and weight bearing of the foot. We conducted a prospective cross sectional study to assess the risk factors of anatomical foot changes in patients with Type-2 diabetes mellitus. It was carried out in normal 196 subjects at Mizan-Tepi University teaching hospital, Bench-Sheko zone, South-West, Ethiopia. Data were collected using a well-structured questionnaires and diabetic foot assessment checklists. Data analysis was done using SPSS, version 24. Whereas, randomly selected associated risk factors were assessed using multivariate linear regression model. Our results revealed an incidence of diabetics-related foot deformities that varied between 7-12%. These deformities include 7% pes cavus, 8.5% hallux valgus, 9% callus, and 12% Claw/Hammer toe. We also demonstrated diabetic related chronic complications: 44.9% foot ulcer, 20.4% peripheral neuropathy, and 18.4% peripheral arterial disease. Duration of diabetes (r= 0.026, p≤0.032) and drinking alcohol (r=0.143, p≤0.007) were significantly and directly associated with diabetic foot deformity. Occupation (r= -0.157, p≤0.003), types of diabetes (r= -0.172, p≤0.002), and presence of neurological symptoms (r= -0.120, p≤0.020) was inversely associated with diabetic foot deformity. We concluded that Hammer/Claw toe was found to be the most prevalent foot deformities among Ethiopians participating in this study and the majority of the study participants did not understand the effect of diabetes on foot health. We found only 18.4% patients were aware of the effects of diabetes on foot health, where 15.8% subjects were identified with appropriate foot care practice mobility among the study population.
Keywords
Deformity; Diabetes mellitus; Foot mechanics; Prevalence; Risk factors
INTRODUCTION
Foot is a very complex anatomical-biomechanical structure. There are numerous bones, joints, ligaments, tendons and muscles in each foot [1]. The foot acts to transmit force between the lower limb and the ground, allowing stable ambulation and stance [2]. Also, foot acts as the foundation of the erect human body posture - its intrinsic structure and positioning can either directly or indirectly influence joints of the lower extremities, pelvis and spine [3]. Effective gait relies on the ability of joints, muscles, tendons and ligaments to react to changes in extrinsic moments during mobility [3]. During normal gait, the foot functions should be as a flexible shock-absorber, deforming to uneven surfaces before undergoing a series of biomechanical changes which allow it to act as a rigid lever to exert force [2].
Diabetes is well documented to have a detrimental effect on multiple morphofunctional systems of the body, and has also been known to be a potentially lethal disease for more than a thousand years [4-7]. Foot problems in patients with diabetes are one of the most serious complications of Diabetes Mellitus (DM), a major public health issue in Sub-Saharan Africa and the commonest reason for hospitalization of patients with diabetes with prevalence as high as 25% [8-10]. Diabetes induced changes in foot posture and architecture will impact the normal biomechanics of walking and weight bearings of the foot [11]. The biomechanics of the diabetic foot are different from that of the non-diabetic foot, where changes occur in the overall gait with specific maladaptive processes occurring in the diabetic foot [12]. Diabetic complications in the lower extremity are common and diverse. Some of the biomechanical alterations common to the diabetic foot are: Diabetic Peripheral Neuropathy (DPN), Peripheral Arterial Disease (PAD), Diabetic Foot Ulceration (DFU), Deformities (Claw/Hammer toe, callus, hallux valgus and pes cavus), Wet gangrene, Abscesses and Necrotizing fasciitis [13-15]. These complications result from complex interactions between diabetic vasculopathy, neuropathy, structural deformity and decreased immunity [8]. Not all of these foot complications can be prevented, though, those underlying cause biomechanical alterations and maladaptive to diabetic foot [12].
In summary, managing the diabetic foot is a complex clinical problem requiring a multidisciplinary collaboration of health care workers to achieve limb salvage [8,9,12]. Misdiagnosis may increase the risk of serious complications including permanent disability and amputations [8,12]. Therefore; an appropriate biomechanical measures should be taken into consideration as an important component in the overall care of the diabetic foot patients.
METHODS AND SUBJECTS
A prospective observational study was conducted at the Mizan-Tepi Teaching Hospital, Mizan-Tepi University, on 196 Type-2 diabetic (126 male and 70 female) patients. The data were collected using well-structured questionnaires and diabetic foot assessment checklists, and the study tool was designed based on the instruments used in other studies. Then, the collected data were coded, entered and analyzed using SPSS, version 24. Selected associated factors were assessed using multivariate linear regression model. The target population was composed of all diabetic patients who already have follow-up in Mizan-Tepi University Teaching Hospital. They were sampled individuals who are already diagnosed as diabetic and came to Mizan-Tepi University Teaching Hospital chronic out-patient department during the study period.
All diabetic patients who have already been diagnosed as type-2 and aged above 18 years were included in the study. However, patients aged below 18 years and patients, whose legs are legally acceptable representative but are not willing to provide voluntary written consent for participation in this study were excluded. The data were collected using a pre-tested self-administered questionnaire and diabetic foot assessment checklists. The study tool was designed based on the instruments used in previous studies, with some modification to fit with the our context, study tool includes four parts, the first contains information about socio-demographic profile, second contains clinical profile, third contains inspection and assessment and fourth contains participants’ knowledge about diabetic foot complication, their attitude and practice regarding diabetic foot care. To ensure the Validity and reliability of the study tool and its use in the study setting, a pilot study was conducted. Minor modifications were made based on the feedback obtained from the participants in the pilot testing to improve clarity of some questions. The pilot study data were excluded from the study results.
Socio-demographic characteristics (sex, age, marital status, level of education, and occupation), medical history (type of diabetes, duration of diabetes, diabetes medications, blood glucose level, history of numbness and tingling, and previous history of foot problems), lifestyle variables (smoking, alcohol intake and physical activity), and physical characteristics (foot ulcers, foot deformities, Body Mass Index (BMI), blood pressure, presence of neuropathy symptoms of tingling, numbness, and burning sensation with a ‘stocking and glove’ distribution, and presence of vascular symptoms of cramps and/or claudication’s were documented.
Fasting blood samples that were taken to assess blood glucose levels were classified into the following groups: before meal 4-7mmol/L or after meal under 8.5mmol/L is normal, <3.8 mmol/L Hypoglycemic, and >11.1 mmol/L Hyperglycemic [16]. Height was measured without shoes by using Stadiometer. Body weight was measured while wearing light clothes by an adjusted scale. Body mass index was calculated by the formula: weight in kilograms divided by height in meters squared (weight in Kg, divided by the square of the height in m2). BMI defined <18.5kg/ m2 underweight, 18.5-24.9 kg/m2 normal, 25-29.9 kg/m2 overweight and >30 kg/ m2 obesity [17,18]. Blood Pressure (BP) was measured by using a sphygmomanometer in sitting position for both arms (right and left) and in lying position for either of the foot at dorsalis pedis and posterior tibial artery. Ankle-Brachial Index (ABI) was calculated by the formula: The highest systolic blood pressure of the leg (Ankle) divided by the higher of the two brachium measurements (ABI= PsL/PsB). ABI classifies as if the ratio is between 0.90-1.30 Normal, between 0.70-0.90 mild, between 0.40-0.69 moderate, and <0.40 severe [19].
Peripheral Neuropathy was assessed by vibratory, muscle strength and tendon reflex testing. Pressure, pain, vibration and joint position sensitivities were evaluated bilaterally. For pressure perception, the neurotips were used on 4 sites on the foot. These sites were without callus, notably the pulps of the Hallux and metatarsal heads off first, third and fifth toes. The site was considered sensate if the patient responded, "Yes" upon contact with the neurotips in all of the four sites of the foot and insensate if there was “No” response in one of the four sites of the foot. For vibration perception, a 128 Hz tuning fork was applied at 3 sites on the foot, the pulp of the Hallux, the lateral and the medial malleoli. The patient was asked to describe what he/she felt. If he/she described a feeling of vibrations in the pulp of the hallux, the site concerned was considered normal. If he/she described anything other than vibrations, the site concerned was considered abnormal [20]. In addition, pinprick perception (using standard neurotips) on the dorsal surface of the great toe and the index finger was evaluated. Neuropathy was further assessed by examining the tendon reflexes bilaterally and testing for muscle strength by examining for extension of the knee and dorsiflexion of the foot [21]. Lower limb ischemia was ascertained by the examining physician through palpation of the dorsalis pedis and the tibialis posterior pulses when one or more foot pulses were judged absent with or without symptoms of lower-limb claudication and/or amputation or gangrene were present. The data were analyzed using IBM SPSS version 24. The result was summarized in the form of proportion, percentage table and graphs for categorical variables.
RESULTS
196 patients participated in this study, out of which 126 (64.3%) were male and 70 (35.7%) were female. The participants` age ranged from 18 to 79, with a mean of (+45.4) 43 (±14. 5) years. The mean age of male was 42.2, while for female was (Table 1). Our findings show that 118 (60.2%) participants were illiterate, followed by 39 (19.9%), 27 (13.8%), 12 (6.1%) of primary, secondary, and university graduates, respectively (Figure 1). We also found 66 (33.6%) of participants were physically active, 48 (24.5%) were alcoholics, and 46 (23.5%) were smokers (Figure 2).
|
Sex |
Age in years |
||
|
Minimum |
Mean |
Maximum |
|
|
Male |
18 |
42.2 |
79 |
|
Female |
18 |
45.4 |
79 |
|
Both |
18 |
43.4 |
79 |
Table 1: Age distribution of study subjects (N=196).
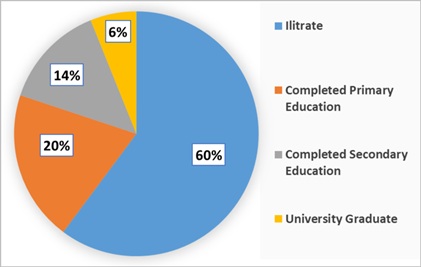 Figure 1: Level of education of study subjects (N=196).
Figure 1: Level of education of study subjects (N=196).
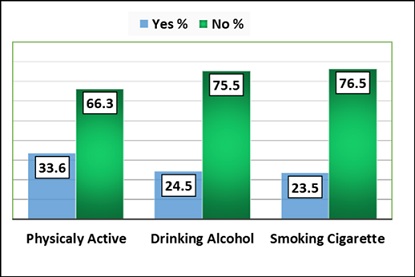 Figure 2: Lifestyle of the study subjects (N=196).
Figure 2: Lifestyle of the study subjects (N=196).
From all participants, 122 (62.2 %) were normal weighted, 68 (34.7%) were obese or overweight and 6 (3.1%) were under weighted. Eighty (40.8%) participant had been diagnosed DM in the past 1-5 years, sixty-three (32.1%) in the past 6-10 years, thirty-five (17.9%) in the past 11-20 years and eighteen (9.2%) in the past more than 21 years (Table 2).
|
Variable
|
Frequency |
Percentage |
|
|
Duration of diabetes |
1-5 years |
80 |
40.8% |
|
6-10 years |
63 |
32.1% |
|
|
11-20 years |
35 |
17.9% |
|
|
>20 years |
18 |
9.2% |
|
|
Body mass index BMI
|
Underweight (<18.5) |
6 |
3.1% |
|
Healthy weight (18.5-24.9) |
122 |
62.2% |
|
|
Overweight and obese (>25) |
68 |
34.7% |
|
|
Blood glucose level
|
< 140mg/dL (<7.7mmol/L) |
137 |
69.9% |
|
> 140mg/dL (>7.7mmol/L) |
59 |
30.1% |
|
Table 2: Clinical characteristic of patients who participated in the study (N=196).
Table 3 depicts the overall prevalence rate of foot deformities of the studied population. The overall prevalence of foot deformities in the studied population was 36.5%. That is, 35(12%) claw/Hammer toe, 26(9%) callus, 25(8.5%) hallux valgus and 20 (7%) pes cavus. We also found that diabetic foot ulcer was 133(44.9%), peripheral neuropathy was 60(20.4%), and peripheral arterial disease was 54(18.4%) (Figure 3).
|
Foot deformity |
Frequency |
Percentage |
|
Claw/Hammer toe |
35 |
12% |
|
Hallux valgus |
25 |
8.50% |
|
Callus |
26 |
9% |
|
Pes cavus (High medial arch) |
20 |
7% |
Table 3: Prevalence of foot deformities (N=196).
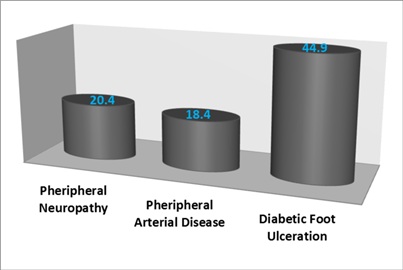 Figure 3: Prevalence of diabetic foot complication (N=196).
Figure 3: Prevalence of diabetic foot complication (N=196).
To quantify the association between risk factors and diabetic foot deformity, multivariate linear regression models were fitted (Table 4). There was statistically significant positive correlation between diabetic foot deformities with duration of diabetes (r= 0.026, p≤0.032) and drinking alcohol (r=0.143, p≤0.007).There was no statistically significant correlation between diabetic foot deformity with age (r=0.089, p≤0.064), sex (r= -0.023, p≤0.345), educational status(r= -0.03, p≤0.305), smoking (r=0.069, p≤0.119), history of previous foot problem (r=0.058, p≤0.162), and physical activity (r= -0.024, p≤0.338). Furthermore, there were a significant negative correlation between diabetic foot deformity with occupation (r= -0.157, p≤0.003), types of diabetes (r= -0.172, p≤0.002), and neurological symptoms(r= -0.120, p≤0.020).
|
|
Foot deformity |
|
|
Pearson`s |
r P-value |
|
|
Age |
0.089 |
0.064 |
|
Sex |
-0.023 |
0.345 |
|
Educational status |
-0.03 |
0.305 |
|
Smoking |
0.069 |
0.119 |
|
Drinking alcohol |
0.143* |
0.007* |
|
Duration of diabetes |
0.026 |
0.0327* |
|
History of previous foot problem |
0.058 |
0.162 |
|
Ulceration |
0.088 |
0.066 |
|
Foot wear condition |
0.028 |
0.317 |
|
Skin breakdown |
0.088 |
0.066 |
|
Nail disorder |
0.045 |
0.223 |
|
Occupation |
-0.157 |
0.003* |
|
Physical activity |
-0.024 |
0.338 |
|
Blood glucose level |
-0.064 |
0.136 |
|
Neurological symptom |
-0.12 |
0.020* |
|
Infection |
-0.089 |
0.064 |
Table 4: The multivariate linear regression analysis of factors associated with diabetic foot deformities (N=196).
We also investigated the knowledge, attitude and practice of study participants regarding effects of diabetes on foot health. From the total participant, only 36 (18.4%) patients understood the effect of diabetes on foot health and only 31(15.8%) of the participants were identified to have appropriate foot care practice. Regarding the participants getting a foot care knowledge; 15(7.7%) were getting by attending foot care class, 40(20.4%) were getting from their health care provider, and 22 (11.2%) were getting by reading handout/leaflets (Table 5).
|
Knowledge and attitudes |
YES |
NO |
||
|
Frequency |
Percentage |
Frequency |
Percentage |
|
|
Do you understand the effects of diabetes on foot health? |
36 |
18.4 |
160 |
81.6 |
|
Can you identify appropriate foot care practices? |
31 |
15.8 |
165 |
84.2 |
|
Have you ever attended a class on how to care for your feet? |
15 |
7.7 |
181 |
92.3 |
|
Have you ever received education about foot care from your healthcare provider? |
40 |
20.4 |
156 |
79.6 |
|
Have you ever read any handouts/leaflets on foot care/footwear? |
22 |
11.2 |
174 |
88.8 |
Table 5: Knowledge, attitude, practice about diabetic foot care and previous diabetic foot education (N=196).
Regarding level of foot care practice, 100 (51%) participants cannot reach their feet for self-care practice, 147 (75%) participants were not inspected their feet regularly, 134 (68.4%) participants were not examined. However, only 74 (37.9%) participants washed and dried their feet, and 66 (33.7%) participants used moisturizers for their feet (Figure 4).
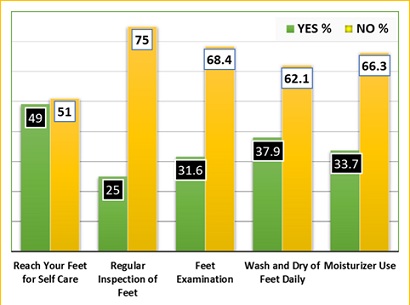 Figure 4: Level of foot care practice (N=196).
Figure 4: Level of foot care practice (N=196).
DISCUSSION
Understanding foot biomechanics of human beings is an important component of the physical examination in hospitals. One among the four most serious complications of diabetes is foot problems. Diabetic foot is related to several commonly identifiable functional and structural foot deformities. It can exist in isolation as well as aggregates to bring predisposition to diabetes related foot complications. Complicated interactions between diabetic vasculopathy, neuropathy, structural deformity, loss of joint mobility and reduced immunity is the best assumption to date. The current investigation adds robust information for future studies [5,13]. In this study, the overall prevalence of foot deformities in the studied population was 36.5%.Claw/hammer toe was higher among them.
Our Study is the first in South Western Ethiopia investigating the prevalence and associated risk factor of foot complication or deformities. Our findings indicate an overall prevalence of foot deformities of 36.5%. The most common structural foot deformities were Claw\Hammer toe followed by (12%), Callus (9%), Hallux valgus (8.5%) and pes cavus (7%). Previous studies carried out in different settings pointed out possible variations in the prevalence foot deformities. Some of these studies showed a lower prevalence than our findings (17-34%) [22,23]. However, another study reported a higher prevalence of foot deformities 44.5%, 64% and 64.2% [24-26]. Similarly, other three studies had also estimated high prevalence of foot deformities ranged between 54.3 % - 79 %, [27-29]. This variation is due to age, presence of underlying health conditions, assessment procedure and poor glycemic control. In addition, because each type of foot deformities has its own prevalence and etiology, this can also lead to a variation in the prevalence outcomes.
Risk factors significantly associated with diabetic foot deformity were duration of diabetes and alcohol intake. In line with our findings, an Iraqi study showed the positive correlation of foot deformity and duration of diabetes [30]. Also, UAE studies found positive correlation of foot deformity and duration of diabetes [31]. Our results also clearly supportthe hypothesis that DM eventually leads to chronic complications, including PVD, PN and DFU [32]. We found DFU (44.9%) was the commonest type of diabetic related foot complication followed by PN (20.4%) and PAD (18.4%). It is in line with the study done in Black Lion Referral Hospital Addis Ababa DFU (39%) [33].
PN is the most common neuropathy syndrome seen in people with diabetes. The prevalence of PN in the literature is 5-80% of the case. Our finding indicated that 20.4% of the study participants possess Peripheral Neuropathy (Figure 3). This findings is in line with the previous study reports of 21.9% [30], but was less than that of 39% [32], 37% [4] and 43.1 % [34]. These variations are due to lack of screening tools, modern imaging modalities and the difference in the number of the sample size. Also, may be due to relative increment in the number of patients who have been diagnosed recently because complications are expected to increase as diagnosed year gap increases whether on treatment or not as different studies showed.
PAD is a condition characterized by a way of atherosclerotic occlusive disorder of the lower extremities. It’s caused by accelerating atherosclerosis, and is a vital threat component for impaired wound healing and lower extremity amputation. Our findings show PAD in 18.4% of the subjects. This is lower than the finding in Tanzania 21% [35] and 36.7% [34]. However, above the percentage found in the studies of 13% [31,32] and 12% [31]. The possible reason for this difference could be due to age, duration and severity of diabetes, poor glycemic control, lifestyle of the study subjects. This is in settlement with previous findings in other Africans [36] Diabetic foot care education and level of practice. Diabetic foot cares have to be begun once the diagnosis of diabetes is made, even if there’s no evidence of foot irregularities. The result of this examination showed an extra share of diabetic patients had a terrible know-how of diabetic foot care. In this examination, around one-third (18.4%) of the study subjects recognized the effects of diabetes strolling fitness. The lack of awareness of foot care in this examination is smaller than a look at carried out in 30.1% [37], 54.4% [38] and 50% [39].
The knowledge of suitable foot care has been suggested to be definitely influenced by means of patient education which in turn reduces the risk of foot complications in this have a look at, 84.2% participants were not identified appropriate foot care practice. This poor level of foot care practice in this look at is greater than 46% [37], 44.7% [38].
The diabetic foot program encompasses screening, examination, diagnostic tests, foot wear recommendation, referrals, follow-ups and patient education. Preventive diabetic foot care education is an essential and a mandatory part inside the overall care of diabetes patients. Unfortunately, a sizable wide variety of patients have been not offered adequate self-care foot education. In the present study 79.6% of the study participants were not received self-care foot education from their health care provider, while I examine it with different studies our result is in line with the study conducted in rural Puducherry, India 79.1% [38] and Karachi, Pakistan 81% [40]. The deficiency inside the understanding may be because of no specified programs that encompass address diabetes education, unlike TB and HIV, which have many national programs and poor communication between the health care provider and the patients; additionally loss of counseling by health care provider as result of busy clinic schedule; and unavailability of diabetic foot care programs. Thus, patient e education to create awareness at the prevention of foot complication is imperative and must be integrated into the routine care of patients with diabetes.
We also found that diabetic foot ulcers were the most prevalent diabetics-related foot complication. Also, the majority of the study participants did not understand the effect of diabetes on foot health and did not identify appropriate foot care practice mobility. To summarize, understanding foot mechanics is an important component of the examination and overall care of diabetic foot. In line with this, an early identification of biomechanical faults will determine anatomical foot change to rule out possible complications as well as to take effective preventive measures. Also, to minimize the burden of a patient, improved screening and prevention programs as well as patient education should be provided to all diabetic patients. We also recommend, a larger scale, global diabetics-related foot deformity research, education and awareness programs to be promoted.
FUNDING
This research received no external funding.
ACKNOWLEDGEMENT
Our most sincere thanks go to Mizan-Tepi University Teaching Hospital health workers for their kindly cooperation throughout the study period. We also, sincerely thank Mizan- Tepi University for assistance.
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interests.
REFERENCES
- Lincoln MJ, Nilasenal DS, Tumer CW, Warner HR, Foerster VA, et al. (1994) Development and Implementation of a Computer-Generated Reminder. Proc Annu Symp Comput Appl Med Care 1994: 831-835.
- Sumpio BE (2012) Contemporary evaluation and management of the diabetic foot. Scientifica (Cairo) 2012: 435487.
- Shavelson D (2011) The Biomechanics of the Diabetic Foot.
- Bowling F (2015) Gait Variability and Kinematic Alterations in People with Diabetes Mellitus and Peripheral Neuropathy. University of Huddersfield, 1-307.
- Elgzyri T (2014) Outcome of ischemic foot ulcer in patients with diabetes, with or without revascularization diabetes and endocrinology.
- Rao SR (2006). Foot and ankle mechanics in individuals with diabetes mellitus and neuropathy. Lowa Research Online, USA.
- Meghna M (2010) Diabetic foot: microbiology, pathogenesis and glycan studies. University of Westminster, UK.
- Barr L (2015) Diabetic foot ulceration: implications of biomechanics on prevention and treatment. Diabetic foot Canada 4: 34-39.
- van Schie CHM (2005) A review of the biomechanics of the diabetic foot. Int J Low Extrem Wounds 4: 160-170.
- Dinh T (2011) Global perspective on diabetic foot ulceration. IntechOpen Limited, UK.
- Uccioli L, Giacomozzi C (2009) Biomechanics and choosing footwear for the diabetic foot. The Diabetic Foot Journal 12: 166-176.
- Kim PJ (2011) Biomechanics of diabetic foot consideration in limb salvage. Adv Wound Care (New Rochelle) 2: 107-111.
- Naidoo P, Liu VJ, Mautone M, Bergin S (2015) Lower limb complications of diabetes mellitus: a comprehensive review with clinicopathological insights from a dedicated high-risk diabetic foot multidisciplinary team. Br J Radiol 88: 20150135.
- D’Souza DM, Al-Sajee D, Hawke TJ (2013) Diabetic myopathy: impact of diabetes mellitus on skeletal muscle progenitor cells. Front Physiol 4: 379.
- Strollol SE Caserotti P, Ward RE, Glynn NW, Goodpaster BH, et al. (2015) A review of the relationship between leg power and selected chronic disease in older adults. J Nutr Health Aging 19: 240-248.
- National Institute for Clinical Excellence (2019). Normal blood glucose level. http://www.diabetes.co.uk/diabetes-care/blood-sugar-level-ranges.html
- World Health Organization (2016) Global report on diabetes. WHO, Switzerland.
- International Diabetes Federation. The IDF consensus worldwide definition of metabolic syndrome, Belgium.
- John Hopkins (2016) Ankle brachial index, USA.
- Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM (1998) Preventive Foot Care in People with Diabetes Care 21: 2161-2177.
- Riaz M, Zaidi SI, Fd Alvi S, Fawwad A, Ahmadani MY, et al. (2014) Characteristics of a large cohort of patients with diabetes having at-risk feet and outcomes in patients with foot ulcerations referred to a tertiary care diabetes unit. Int Wound J 13: 594-599.
- Bakri FG, Allan AH, Khader YS, Younes NA, Ajlouni KM (1012) Prevalence of diabetic foot ulcer and its associated risk factors among diabetic patients in Jordan. J Med J 46:118 -25.
- Ndip EAA, Tchakounte B, Mbanya J-C (2006) A study of the prevalence and risk factors of foot problems in a population of diabetic patients in Cameroon. Int J Low Extrem Wounds 5: 83-88.
- Walters DP, Gatling W, Hill RD, Mullee MA (1993) The prevalence of foot deformity in diabetic subjects: a population study in an English community. Practical Diabetes International 10:106-108.
- Ababneh A, Bakri F, Khader Y, Lazzarini P, Ajlouni K (2020) Prevalence and Associates of Foot Deformities among Patients with Diabetes in Jordan. Curr Diabetes Rev 16: 471-482.
- Helfand AE (2004) Foot problems in older patients: a focused podogeriatric assessment study in ambulatory care. J Am Podiatr Med Assoc 94: 293-304.
- Jones NJ, Chess J, Cawley S, Phillips AO, Riley SG (2013) Prevalence of risk factors for foot ulceration in a general haemodialysis population. Int Wound J 10: 683-688.
- Dòria M, Rosado V, Pacheco LR, Hernández M, Betriu À, et al. (2016) Prevalence of diabetic foot disease in patients with diabetes mellitus under renal replacement therapy in Lleida, Spain. Biomed Res Int 2016: 7217586.
- Kaminski M, Frescos N, Tucker S (2012) Prevalence of risk factors for foot ulceration in patients with end-stage renal disease on haemodialysis. Intern Med J 42: 120-128.
- Mansour AA, Imran HJ (2006) Foot abnormalities in diabetics: prevalence & predictors in Basrah, iraq. Pak J Med Sci 22: 229-233.
- Al-Maskari F, El-Sadig M (2007) Prevalence of risk factors for diabetic foot complications. BMC Fam Pract 8: 59.
- Ramachandran A (2004) Specific problems of the diabetic foot in developing countries. Diabetes Metab Res 1: 19-22.
- Gizaw M, Harries AD, Ade S, Tayler-Smith K, Ali E, et al. (2015) Diabetes mellitus in Addis Ababa, Ethiopia: admissions, complications and outcomes in a large referral hospital. Public Health Action 5: 74-78.
- Yusof NM, Abu Rahman J, Zulkifli AH, Che-Ahmad A, Khalid KA, et al. (2015) Predictors of major lower limb amputation among type II diabetic patients admitted for diabetic foot problems. Singapore Med J 56: 626-631.
- Abbas ZG, Archibald LK (2007) Challenges for management of the diabetic foot in Africa: Doing more with less. Int Wound J 4: 305-313.
- Abbas ZG, Archibald LK (2005) Epidemiology of the diabetic foot in Africa. Med Sci Monit 11: 262-270.
- Troskot N, Duvancic T, Kolic M (2013) Diabetic foot syndrome – dermatological point of view. Acta Clin Croat 52: 99-106.
- Saurabh S, Sarkar S, Selvaraj K, Kar SS, Kumar SG, et al. (2018) Effectiveness of foot care education among people with type 2 diabetes in rural Puducherry, India. Indian J Endocrinol Metab 18: 106-110.
- Jinadasa CVM, Jeewantha M (2011) A study to determine the knowledge and practice of foot care in patients with chronic diabetic ulcers. International Journal of Collaborative Research on Internal Medicine & Public Health. 3: 115-122.
- Musarrat R, Miyan Z, Zaidi SI, Fd Alvi S, Fawwad A, et al (2014) Characteristics of a large cohort of patients with diabetes having at-risk feet and outcomes in patients with foot ulceration referred to a tertiary care diabetes unit. Int Wound J 13: 594-599.
Citation: Mekonnen BE, Wirtu AT, Kebede MA, Tilahun AG, Degaga TK (2021) Diabetics-Related Foot Deformity: Prevalence, Risk Factors, Knowledge and Practice. Trends Anat Physiol 4: 010.
Copyright: © 2021 Biruk Endalkachew Mekonnen, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.