
Diagnostic and Therapeutic Features of Full-Term Abdominal Pregnancy with Live Fetuses: Two Cases Study at the Nabil Choucair Health Center (Dakar - Senegal) With Literature Review
*Corresponding Author(s):
Mor CisseGynecologic And Obstetrical Clinic At The Teaching Hospitals Aristide Le Dantec, BP 3001, Pasteur Avenue, Dakar, Senegal
Email:morbaye66@gmail.com
Abstract
Abdominal pregnancy is a relatively common pathology in developing countries, including Senegal, due to insufficient technical support and poor quality prenatal consultations. Its diagnosis is often late in developing countries. Treatment is always surgical through laparotomy and fetal prognosis is poor. We report two cases of full term secondary abdominal pregnancy with a living fetus at the Nabil Choucair Health Center. The first case was an abdominal pregnancy in a nulliparous with abortion as health history. The diagnosis is established during an ultrasound at 23 Weeks of Amenorrhea indicated by symptoms suggestive of abdominal pregnancy. The second case was an abdominal pregnancy in a 44 years old multiparous woman with poor prenatal follow-up, whose diagnosis was made by chance intraoperatively (cesarean section for placenta praevia covering associated with an oligoamnios). In both cases, the treatment was surgical and the fetal prognosis was good. However, the functional maternal prognosis was poor in the second case where hysterectomy with unilateral adnexectomy was performed.
Keywords
Abdominal pregnancy; Laparotomy; Living fetus; Nabil Choucair Health Center
OBSERVATIONS
Nabil Choucair is a health center in Dakar Senegal, which has annually 5000 deliveries and deliveries are more than important in September and October.
First observation
It was a 26-year old nulliparous on her second pregnancy married for 5 years with the notion of spontaneous abortion a year ago at 3 months of pregnancy. She had no particular medical history. The patient had been consulted at the emergency ward at the gynecology department for diffuse pelvic and abdominal pain with no particular characteristics, associated with incoercible vomiting in a context of secondary amenorrhea of 3 months without metrorrhagia. The clinical examination had shown a patient in good general condition, apyretic and her conjunctiva were normally colored. The abdomen was enlarged and deformed with perception of the fetal cephalic pole at the right hypochondrium and its caudal pole at the left iliac fossa. Fetal heart beats could be perceived at the peri umbilical level and were estimated at 144 beats per minute. The obstetrical examination found a subnormal uterus, a clean vulva and a firm cervix to the vaginal touch. The abdominal-pelvic ultrasound examination, performed by 3.5 and 7.5 MHz probes, confirmed the diagnosis of an active abdominal pregnancy of 23 Weeks of amenorrhea. The uterus size was slightly enlarged with an empty, thin, median cavity line (Figure 1). The fetal head was in contact with the underside of the liver, while its seat was located in the left iliac fossa in contact with the left colon. The placenta was outside the uterine cavity, adhering to the posterior surface of the uterine fundus and the intestinal handles. The pregnancy was estimated at 23 weeks of amenorrhea plus 4 days without any deformities.
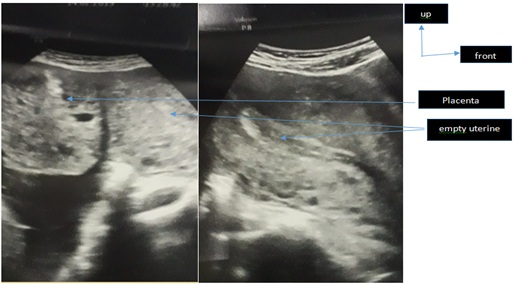
Figure 1: Obstetrical ultrasound in longitudinal section showing a slightly increased uterus size with a vacuity of the median line, placenta adhering to the uterine fundus.
Despite the maternal and fetal risks, the patient would like to carry the pregnancy to its term. A laparotomy for fetal extraction had been scheduled at 37 SA. Given the risks, the patient was followed regularly, with repetitive obstetrical examinations and ultrasound, and she was hospitalized for several days before surgery. Laparotomy with xypho-pubic incision had revealed a living fetus in the abdominal cavity contained in its amniocortical membranes (Figure 2). After opening the membranes, a female live foetus without any diformities was extracted, weighing 2100 grams with an Apgar score of 7/10 at the fifth minute.
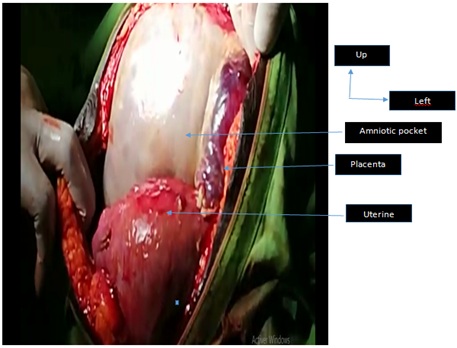
Figure 2: laparotomy Exploration.
After clamping the cord, we found a placenta adhering to the posterior surface of the uterine fundus, at the omentum, and to the left adnexa with moderate bleeding at its bed level and requiring its complete removal by close-to-close dissection (Figure 3). We performed Peritoneal haemostasis and cleansing and we compensated blood lost intraoperatively by the transfusion of three packed of red blood cells. The postoperative follow-ups were simple. At the last check-up, the mother and child were doing well (Figure 4).
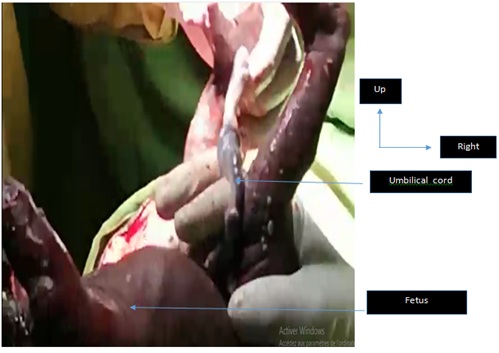
Figure 3: Fetal extraction.

Figure 4: Adhesiolysis of placenta insertion sites.
Second observation
We report an observation of a woman who was 44-year-old sixth parous on her sixth pregnancy, with as health history, 5 vaginal deliveries with 5 healthy live children. She was evacuated by a colleague from a local hospital for acute fetal pain and anamnios on a 37-week pregnancy of amenorrhea. The prenatal logbook mentioned five prenatal consultations without any ultrasound. On her admission, the general condition was still maintained with colored and anicteric conjunctival mucosa, blood pressure at 120/80 mmHg, temperature at 37°c and weight at 80 kg. The obstetrical examination found a uterine transversely spread with a height of 30 cm, regular fetal heart sounds at 146 beats per minute, vaginal touch revealed a half long, flexible and dehiscent posterior cervix with an empty excavation and a not well-appreciated presentation.
An ultrasound scan performed at the local hospital showed an active intrauterine monofetal pregnancy of 37 Weeks of Amenorrhea in transverse presentation, with the head at the left side. The ultrasound also showed a low inserted placenta totally covering with a severe oligoamnios associated with a 40/23mm anterior corporal type 3 myoma weighing 2260 grams. A C-section was indicated for a placenta previa associated with severe oligoamnios and transverse presentation. During the cesarean section, our exploration showed a slightly enlarged globular uterus and a fetus in the abdominal cavity covered by the omentum in a transverse position. We proceeded to the extraction of a newborn by podalic traction and then to the ligation of the cord section. It was a male newborn weighing 2200 grams with an Apgar score of 9/10 at the fifth minute whose examination after birth revealed no particularities.
It is safer not to remove an adherent placenta in case the latter is inserted into the posterior surface of the uterus with adhesions at the intestinal handles with a right fallopian tube that completely adhered to it. The postoperative follow-ups were simple and the patient was released 10 days after admission. One month later, the patient came back with a sub-occlusive syndrome table and abdominal pain, vomiting and discontinuation of faeces and gases. A laparotomy was performed and the exploration found a placenta caught in adhesion magma between the uterus at its posterior surface and the right adnexa with a small insertion at the rectum. It should be noted that there is an outlet of more than about 20 ml from the placenta. We performed a hysterectomy and a right adnexectomy combined with conservation of the left adnex and subsequent removal of the placenta. The postoperative follow-ups were simple and the patient was released one week after his readmission.
DISCUSSION
Epidemiological aspects
The incidence of abdominal pregnancy varies from country to country, from 1/10000 to 15000 deliveries in Europe and 1/2000 deliveries in developing countries [1]. Its frequency is influenced by the risk factors of ectopic pregnancy: genital malformations, sequelae of specific or non-specific genital infections, sequelae of tubal surgery and low socio-economic background [2]. The high frequency in developing countries is related to two factors depending on the socio-economic level of the country: the incidence of genital infection on the one hand and the inadequate pregnancy follow-up on the other [1]. Our second observation concerned a multiparous, who had not performed any ultrasound during her pregnancy follow-up. Both observations were characterized by low socio-economic level.
Diagnostic aspects
Though clinical diagnosis is often difficult, a group of signs can guide the diagnosis towards an abdominal pregnancy: digestive disorders, abdominal-pelvic pain concomitant with fetal movements, superficial fetus and cervix fixed under the pubic symphysis. In our first observation, the patient had widespread pelvic and abdominal pain and vomiting. Ultrasound is an important part of the diagnosis of abdominal pregnancy. However, the fetal ultrasound examination is often difficult due to the frequency of oligohydramnios, which hinders morphological examination [2]. The Ministry of Health and Social Action of Senegal recommends four prenatal checkups during pregnancy and three ultrasound scans. In our second case, the patient had not performed any ultrasound examinations during her pregnancy. However, ultrasound had made it possible to diagnose the disease as early as 23 AS in our first observation. The lack of ultrasound use is related to two factors: the absence of prescription due to unqualified personnel and lack of financial resources to cover the examination fees [3]. In developed countries where Magnetic Resonance Imaging (MRI) can be performed easily, diagnosis is easier. The MRI finds an empty uterus, a fetus in the abdominal cavity not circumscribed by myometrial tissue, a frequently transverse presentation and an oligoamnios [2]. In our developing countries MRI is almost inaccessible and ultrasound still has its limits as far as abdominal pregnancy diagnosis is concerned; as the result the SHIBANGU or “modified DIADHIOU” test could be a crucial tool in diagnosing abdominal pregnancy. This test consists in performing an X-ray of the small pelvis after introducing a hysterometer into the uterine cavity. Thus, the pelvic radiograph will show the hysterometer in an empty uterine cavity, meaning that does not contain any fetuses.
Therapeutic aspects
Therapeutic management is always surgical. If the fetus dies in utero, a regulated laparotomy will be scheduled [4] so as not to expose the mother to infectious and bleeding disorders. If the fetus is alive, before 20 AS, termination of the pregnancy should be discussed. The usual approach is a laparotomy, a few rare cases of laparoscopic approach for pregnancies with less than 12 AS have been reported [2]. After 20 AS, a laparotomy will be scheduled at 34 AS [5] after fetal pulmonary maturation. Because of the risk of uncontrollable bleeding, any attempt to extirpate the placenta is strictly prohibited if the placenta is inserted on a noble organ or a vessel [6]. If delivery is possible, it is performed intraoperatively. The classic attitude is to leave the placenta in place by cutting the cord as close as possible [3]. Placental resorption is controlled by ultrasound and the determination of placental hormones (chorionic gonadotropic hormone). To accelerate placental resorption, Methotrexate may be recommended [7]. In our second observation, the diagnosis of abdominal pregnancy was made intraoperatively at 37 AS and we didn’t remove the placenta because of these intestinal adhesions.
However, in our first observation, the diagnosis was made at 23 AS and the pregnancy was continued up to 37 AS. The delivery was carried out intraoperatively.
Prognostic aspects
Fetal prognosis is often poor with a high stillbirth rate, 75% to 95% [4]. It was nil for our two observations. The causes of death are related to fetal hypotrophy and diformities. However, in our observations, no diformities were found but hypotrophy was noted with a birth weight of 2200 grams and 2100 grams at 37 AS. Maternal prognosis depends on the early diagnosis and attitude towards the placenta [1]. Maternal mortality ranges from 0% to 18%, mainly due to haemorrhages and infectious complications [2]. In our series, we did not observe any maternal deaths, but the functional prognosis is taken into account in our second observation because of hysterectomy with right adnexectomy related to infectious complications.
CONCLUSION
Abdominal pregnancy is a common pathology encountered in countries where medicalization is insufficient. The clinical examination, in front of certain signs, makes it possible to suspect it. Ultrasound should be systematic and should be carried out in a rigorous manner. Not only is it essential but it occupies a prominent place in the diagnosis of this pathology. Training medical and paramedical staff in ultrasound, and its systematic use during pregnancy could improve diagnosis and prognosis. The SHIBANGU or modified DIADHIOU test remains valid in developing countries. The fetal prognosis is poor in all cases and that of the mother can be preserved if diagnosis is done in time.
REFERENCES
- Ombelet W, Vandermerwe JV, Van Assche FA (1988) Advanced extrauterine pregnancy: Description of 38 cases with literature survey. Obstet Gynecol Surv 43: 386-387.
- Mahi M, Boumdin H, Chouir S, Salaheddine T, Attioui D, et al. (2002) Un nouveau cas de grossesse abdominale. J Radiol 83: 989-992.
- Correa P, Atayi L, Cave L, Lauroy L, Bourgon P (1965) Quelques aspects particuliers de la grossesse abdominale. A propos de 18 cas relevés en milieu africain à Dakar. Bull Fed Gynecol Obstet 17: 872-874.
- Diouf A, Diouf F, Cissé C.T, Diallo D, Gaye A, et al. (1996) La grossesse abdominale à terme avec enfant vivant : à propos de deux cas. J Gynecol Obset Biol Reprod 25: 212-215.
- Ranphal S, Moodley J (1998) Advanced extrauterine pregnancy, Curr Obset Gyneacol 8: 90-95.
- Gueye M, Cissé ML, Gueye SMK, Guèye M, Diaw H, et al. (2012) Difficultés du diagnostic et de prise en charge de la grossesse abdominale: à propos de deux cas diagnostiqués à terme au centre hospitalier de Diourbel du Sénéga Clinics in mother and childhealth 9: 1-3.
- Spanta R, Roffman LE, Grissom TJ, Newland JR, McManus BM (1987) Abdominal pregnancy: Magnetic resonance identification with ultrasonographic follow-up of placental involution. Am J Obstet Gynecol 157: 887-889.
Citation: Cisse M, Gassama O, Biaye B, Fall KBM, Gueye KA, et al. (2020) Diagnostic and Therapeutic Features of Full-Term Abdominal Pregnancy with Live Fetuses: Two Cases Study at the Nabil Choucair Health Center (Dakar - Senegal) With Literature Review. J Reprod Med Gynecol Obstet 5: 041.
Copyright: © 2020 Mor Cisse, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

