
Diagnostic Challenge of Isolated Alpha-Fetoprotein Elevation: A Case Report
*Corresponding Author(s):
Ouattara Zanga DamienDepartment Of Gastroenterology, Regional University Hospital Center Of Ouahigouya, Burkina Faso
Email:damzang@gmail.com
Abstract
Mixed gastric tumors are rare. We report a clinical case in which an isolated increase in alpha-fetoprotein preceded the onset of clinical symptoms.
Clinical observation:
A 48-year-old woman was referred to gastroenterology for an isolated elevation of alpha-fetoprotein discovered during an annual health check-up. Liver function tests were normal. The ovaries and hormonal profile were also normal. Clinical manifestations appeared two years after the incidental finding of this laboratory abnormality. The patient reported nocturnal ulcer-type pain relieved by food intake and exacerbated by fasting. Upper gastrointestinal endoscopy revealed an ulcerated, exophytic tumor on the lesser curvature of the antrum. Biopsy results suggested a poorly differentiated adenocarcinoma, and surgery was indicated. After total gastrectomy, a second neuroendocrine tumor was incidentally identified in the antrum during histopathologic examination. There was no lymph node or locoregional infiltration, nor distant metastasis. The primary tumor was a poorly differentiated pT3 adenocarcinoma, and the neuroendocrine tumor was classified as mucosal pT1. Immunohistochemical staining for synaptophysin and chromogranin was positive. The mitotic index of the neuroendocrine tumor was 0/10 HPF, with a Ki-67 index below 1%. No alpha-fetoprotein staining was observed. The patient’s blood AFP level returned to normal one month after surgery, supporting the hypothesis of gastric origin of AFP secretion by the second neuroendocrine tumor.
Conclusion:
This case highlights the need for thorough investigation—particularly of the stomach—in the presence of isolated alpha-fetoprotein elevation without associated liver disease. This biological abnormality may reveal serious malignant conditions such as neuroendocrine tumors or even hepatoid adenocarcinomas.
Keywords
Alpha-Fetoprotein; Gastrectomy; Gastric Adenocarcinoma; Neuroendocrine Tumor.
Introduction
Gastric cancers rank 9th among cancers in Africa according to GLOBOCAN 2022; in Burkina Faso, they represent the 12th most common cancer, with a projected incidence of 2.7 per 100,000 inhabitants in the next five years [1]. However, mixed gastric tumors are rare and are mostly described in the literature through case reports [2–4]. Their clinical presentations are variable, and diagnosis is sometimes made postmortem during autopsy [2,5,6]. The multiplicity of histological patterns, together with scientific advances—particularly the detection of specific antibodies on biopsy specimens, molecular biology, and histo-immunochemical staining—led the WHO in 2019 to adopt a standardized classification for mixed tumors of the digestive tract [7].
Alpha-fetoprotein is a glycoprotein produced during pregnancy by the fetal liver and yolk sac, with peak production between 13 and 15 weeks of gestation [4]. AFP measurement is indicated in chronic liver diseases and, above all, in the diagnosis of hepatocellular carcinoma. Its quantification is therefore not systematic in our practice setting and is usually driven by clinical suspicion. We report here a case of well-differentiated gastric adenocarcinoma, signaled two years before the appearance of clinical symptoms by an isolated increase in alpha-fetoprotein found during an annual health check-up. This cancer was associated with a neuroendocrine tumor.
Case Report
A 48-year-old woman was referred to gastroenterology in January 2022 for an isolated increase in alpha-fetoprotein. The test had been ordered as part of her annual systematic health evaluation by her cardiologist. Her past medical history included grade 1 hypertension under treatment and sickle-cell trait (HbAS). She did not smoke and did not consume alcohol.
The patient was asymptomatic. Initial AFP level was 15 ng/mL, and 19 ng/mL five days later.
Liver function tests were normal, without cytolysis or hepatocellular insufficiency. Viral markers for hepatitis B and C were negative. The patient was immunized against hepatitis B, with an anti-HBs titer of 2356 IU/mL. Abdominal ultrasound showed a steatotic liver without dysmorphia and no signs of portal hypertension. Ovaries had a normal sonographic appearance without dystrophy. Abdominopelvic CT scan was normal. Bone scintigraphy was normal. Carcinoembryonic antigen (CEA) and CA 19-9 levels were within normal limits. Upper digestive endoscopy showed congestive mucosa of the supracardial region suggestive of grade 1 peptic esophagitis and a small sliding hiatal hernia.
The patient returned in January 2024 (two years after her previous consultation) with ulcer-type epigastric pain. The pain was nocturnal, worsened by fasting, and relieved by food or antacids. Upper gastrointestinal endoscopy showed a small hiatal hernia and an ulcerated, exophytic lesion on the gastric lesser curvature (Image 1).
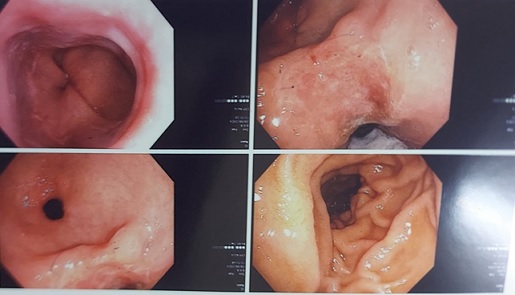
Picture 1: endoscopic images of gastroscopy
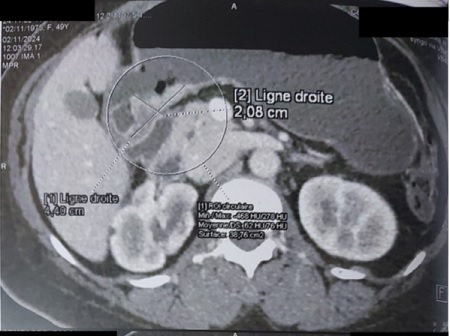
Histopathological examination of the biopsies concluded to a poorly differentiated adenocarcinoma of the lesser curvature. Thoraco-abdominopelvic CT scan revealed posterior gastric wall thickening measuring 44 mm in height and 24 mm in thickness, without metastatic lesions (Image 2).
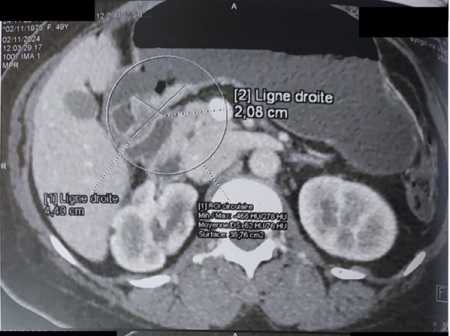 Picture 2 : Abdominal CT scan image showing a thickening of the posterior wall of the stomach measuring 44 x 24 mm
Picture 2 : Abdominal CT scan image showing a thickening of the posterior wall of the stomach measuring 44 x 24 mm
Blood tests showed a hemoglobin level of 11.4 g/dL, platelets at 358,000/mm³, and normal leukocyte count. Repeat tumor marker testing (CEA, CA 15-3, CA 19-9) was normal. AFP was now elevated at 106.6 ng/mL.
A total gastrectomy with lymph node dissection was recommended after multidisciplinary tumor board discussion, based on the diagnosis of poorly differentiated antral adenocarcinoma.
Pathology Findings
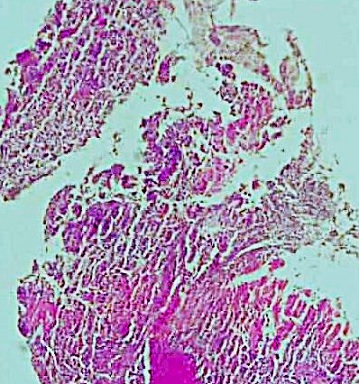
Macroscopic examination of the surgical specimen revealed an ulcerated tumor measuring 3.5 cm in length, 3.5 cm in width, and 0.7 cm in thickness. It was located on the lesser curvature, 1 cm from the distal surgical margin. The tumor infiltrated the gastric wall and was situated 0.1 cm from the serosa. The specimen also included 12 lymph nodes from the lesser curvature and 15 lymph nodes from the greater curvature (Image 3).
 Picture 3 : Ulcerated and budding lesion measuring 5×4cm with necrotic changes located in the antrum 1.5cm from the distal (duodenal) surgical section
Picture 3 : Ulcerated and budding lesion measuring 5×4cm with necrotic changes located in the antrum 1.5cm from the distal (duodenal) surgical section
A second tumor measuring 1.8 mm was incidentally discovered during the histopathologic examination of the antrum.
Histological analysis of the main tumor revealed a poorly differentiated tubular adenocarcinoma, grade III. The tumor was classified as pT3. There was no perforation, nor lymphatic, venous, or perineural invasion (Image 4). All lymph nodes were free of metastasis.
 Picture 4: Poorly differentiated, grade III tubular adenocarcinoma of the stomach
Picture 4: Poorly differentiated, grade III tubular adenocarcinoma of the stomach
 A second tumor, located at a distance from the adenocarcinoma within the antrum, was incidentally identified. It was a well-differentiated neuroendocrine tumor measuring 1.8 mm, grade 1, confined to the mucosa and classified as pT1. Immunohistochemical staining for synaptophysin and chromogranin was positive. The mitotic index was 0/10 HPF, with a Ki-67 index below 1%. No alpha-fetoprotein staining was observed in this second tumor.
A second tumor, located at a distance from the adenocarcinoma within the antrum, was incidentally identified. It was a well-differentiated neuroendocrine tumor measuring 1.8 mm, grade 1, confined to the mucosa and classified as pT1. Immunohistochemical staining for synaptophysin and chromogranin was positive. The mitotic index was 0/10 HPF, with a Ki-67 index below 1%. No alpha-fetoprotein staining was observed in this second tumor.
Postoperative course following total gastrectomy was uneventful. Reconstruction consisted of an esophagojejunostomy with a Y-shaped arrangement of the duodenopancreatic segment. Follow-up laboratory tests one month after surgery showed normalization of alpha-fetoprotein levels. The patient remained asymptomatic 12 months after surgery, with normal laboratory findings to date.
Discussion
This case is noteworthy due to the isolated elevation of alpha-fetoprotein preceding the appearance of a gastric tumor by two years. This diagnostic delay can be explained both by the limited diagnostic capabilities available in our hospital settings and by the rarity of hormonally active gastric tumors, particularly those secreting alpha-fetoprotein.
Gastric tumors are relatively rare in Africa, especially in Burkina Faso, where they rank 12th among cancers according to GLOBOCAN 2022 [1]. This low prevalence is paradoxical when considering the high prevalence of Helicobacter pylori infection reported by multiple authors [8–14].
The association of a gastric neuroendocrine tumor with a gastric adenocarcinoma is even rarer. Several types of associations and histological subtypes of neuroendocrine neoplasms have been described [7,15,16].
The epidemiology of neuroendocrine neoplasms is difficult to establish, as the literature is dominated by case reports. However, in a retrospective study of 1,538 surgically treated gastric cancers, Isawaki et al. [17] identified 25 cases (1.6%) of associated neuroendocrine tumors, including 13 cases (0.8%) of neuroendocrine carcinoma or mixed neuroendocrine–non-neuroendocrine neoplasms.
Neuroendocrine neoplasms are classified into neuroendocrine tumors, neuroendocrine carcinomas, and mixed neuroendocrine–non-neuroendocrine neoplasms, the latter requiring each component to represent at least 30% of the tumor mass [2,7,18].
Genetic mutations such as MEN1, DAXX, ATRX (associated with well-differentiated NETs) and TP53, RB1 (associated with neuroendocrine carcinomas) [7], as well as immunohistochemical testing for alpha-fetoprotein secretion, were not assessed in this case and constitute a limitation of the study.
Nonetheless, the histological findings in our patient clearly indicate an association of two distinct gastric tumors: a poorly differentiated adenocarcinoma and a neuroendocrine tumor. A diagnosis of mixed neuroendocrine–non-neuroendocrine neoplasm requires both components to coexist within the same tumor and each to represent at least 30% of the mass [7]. In our case, the neuroendocrine tumor did not account for 30% of the main lesion. The mitotic index of 0/10 HPF and low Ki-67 index likely explain the limited aggressiveness of the neuroendocrine tumor, the absence of metastasis, and the modest elevation of alpha-fetoprotein. Indeed, hepatoid adenocarcinomas described in the literature typically exhibit markedly elevated AFP levels, often exceeding 300 ng/mL [4,19–21].
This dual tumor localization is rarely reported. Most cases in the literature describe hormonally active gastric adenocarcinomas secreting alpha-fetoprotein [4–6,15,20,22–26]. AFP-secreting gastric tumors are most commonly hepatoid adenocarcinomas [4,6,20,27,28], which are rare, frequently described as case reports, and generally associated with poor prognosis.
Li et al. [19], in a retrospective collection of cases from 1984 to 2020, reported 252 cases of hepatoid adenocarcinoma, with more than 60% occurring in patients over 60 years old. Lesions were located in the gastric antrum in 51% of cases and showed an ulcerative appearance in 51%. Tumors were poorly differentiated in 80%.
AFP secretion exceeded normal levels in 76.7% of cases and exceeded 300 ng/mL in 47%. A second histological subtype capable of secreting AFP and described in the literature is gastric adenocarcinoma with enteroblastic differentiation [15,29]. Other even rarer histological variants include gastric adenocarcinoma associated with germ cell tumors [3], ovarian clear cell carcinoma [24], or combinations of carcinosarcoma and hepatoid adenocarcinoma [6].
Conclusion
This case highlights a dual gastric localization consisting of a neuroendocrine tumor and a poorly differentiated adenocarcinoma secreting alpha-fetoprotein. The two-year diagnostic delay reflects the challenges of medical practice in our context. This case also underscores the importance of systematically investigating any elevation of alpha-fetoprotein, even when isolated, in asymptomatic patients with preserved general condition. In the absence of classic causes such as chronic liver disease or germ cell tumors, the possibility of adenocarcinomas—particularly gastric forms—should be carefully explored.
References
- Filho AM, Laversanne M, Ferlay J, Colombet M, Piñeros M, et al. (2025) The GLOBOCAN 2022 cancer estimates: Data sources, methods, and a snapshot of the cancer burden worldwide. Int J Cancer 156: 1336–1346.
- Carvalho T, Coutada A, Jácome M, Fernandes D (2024) Gastric Mixed Neuroendocrine-Non-Neuroendocrine Neoplasm: An Unusual Tumor and Its Presentation in a Young Adult. GE Port J Gastroenterol 31: 432–436.
- Han X, Wang S, He H, Sun Y, Li J (2022) Gastric adenocarcinoma with germ cell tumor components: a rare case report. J Int Med Res 50: 3000605211069202.
- Inagawa S, Shimazaki J, Hori M, Yoshimi F, Adachi S, et al. (2001) Hepatoid adenocarcinoma of the stomach. Gastric Cancer 4: 43–52.
- Hirota S, Naganuma A, Kobayashi R, Suzuki Y, Hoshino T, et al. (2023) An autopsy case of alpha-fetoprotein-producing large duodenal adenocarcinoma. Clin J Gastroenterol; 16: 829–835.
- Li Z, Zhou Q, Lu J, Zhang H, Teng L (2021) Carcinosarcoma of the stomach with alpha-fetoprotein-producing hepatoid adenocarcinoma: an unexpected combination of two rare subtypes of gastric cancer in one tumor. J Int Med Res. 49.
- Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, et al. (2020) WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology. 76: 182–188.
- Asombang AW, Kelly P (2012) Gastric cancer in Africa: what do we know about incidence and risk factors? Trans R Soc Trop Med Hyg. 106: 69-74.
- Ghoshal UC, Chaturvedi R, Correa P (2010) The enigma of Helicobacter pylori infection and gastric cancer. Indian J Gastroenterol. 29: 95-100.
- Ilic M, Ilic I (2022) Epidemiology of stomach cancer. World J Gastroenterol. 28: 1187-1203.
- Lunet N, Barros H (2003) Helicobacter pylori infection and gastric cancer: facing the enigmas. Int J Cancer. 106: 953-960.
- Segal I, Ally R, Mitchell H (2001) Gastric cancer in sub-Saharan Africa. Eur J Cancer Prev. 10: 479-482.
- Shirani M, Pakzad R, Haddadi MH, Akrami S, Asadi A ,et al. (2023) The global prevalence of gastric cancer in Helicobacter pylori-infected individuals: a systematic review and meta-analysis. BMC Infect Dis. 23: 543.
- Smith SI, Ajayi A, Jolaiya T, Onyekwere C, Setshedi M, et al. (2022) African Helicobacter and Microbiota Study Group. Helicobacter pylori Infection in Africa: Update of the Current Situation and Challenges. Dig Dis. 40: 535-544.
- Abe D, Akazawa Y, Yatagai N, Hayashi T, Ueyama H, et al. (2023) Clinicopathological characteristics of gastric adenocarcinoma with enteroblastic differentiation and gastric adenocarcinoma with enteroblastic marker expression. Virchows Arch. 483: 405-414.
- Panzuto F, Ramage J, Pritchard DM, van Velthuysen MF, Schrader J, et al. (2023)European Neuroendocrine Tumor Society (ENETS) 2023 guidance paper for gastroduodenal neuroendocrine tumours (NETs) G1-G3. J Neuroendocrinol. 35: e13306.
- Iwasaki K, Barroga E, Enomoto M, Tsurui K, Shimoda Y, et al. (2022) Long-term surgical outcomes of gastric neuroendocrine carcinoma and mixed neuroendocrine-non-neuroendocrine neoplasms. World J Surg Oncol. 20: 165.
- Rindi G, Petrone G, Inzani F (2014) The 2010 WHO classification of digestive neuroendocrine neoplasms: a critical appraisal four years after its introduction. Endocr Pathol. 25: 186-192.
- Li L, Yang X, Ji W, Zhu Q, Yang X, et al. (2023) Emphasis on the clinical relationship between alpha-fetoprotein and hepatoid adenocarcinoma of the stomach: a retrospective study. BMC Gastroenterol. 23: 142.
- Li M, Mei YX, Wen JH, Jiao YR, Pan QR, et al. (2023) Hepatoid adenocarcinoma-Clinicopathological features and molecular characteristics. Cancer Lett. 559: 216104.
- Zi M, Ma Y, Chen J, Pang C, Li X, et al. (2024) Clinicopathological characteristics of gastric neuroendocrine neoplasms: A comprehensive analysis. Cancer Med. 13: e7011.
- Ge DF, Wang YK, Li YY, Liao XH, Zhu CY, et al. (2024) Assessing clinical pathological characteristics and gene expression patterns associated with hepatoid adenocarcinoma of the stomach. Clin Transl Oncol. 26: 2674-2684.
- Kimura M, Matsuoka R, Nishikawa K, Imamura J, Kimura K (2024) Alpha-fetoprotein-producing gastric cancer with ruptured liver metastasis mimicking hepatocellular carcinoma. Clin J Gastroenterol. 17: 234–239.
- Kuriyama S, Yano M, Kusaba T, Zaitsu S, Nishida H, et al. (2023) Immunohistochemical and molecular analysis of an α-fetoprotein-producing cervical adenocarcinoma with clear cell morphology. Med Mol Morphol. 56: 20-27.
- Lu J, Jin M, Zhou X, Chen X, Shao Y, et al. (2022) Clinicopathological and molecular characteristics of the alpha-fetoprotein-producing gastric cancer: emphasis on two major subtypes. APMIS. 130: 169-180.
- Yang X, Wu Y, Wang A, Ma X, Zhou K, et al. (2024) Immunohistochemical characteristics and potential therapeutic regimens of hepatoid adenocarcinoma of the stomach: a study of 139 cases. J Pathol Clin Res. 10: e343.
- Qu BG, Bi WM, Qu BT, Qu T, Han XH, et al. (2016) PRISMA-Compliant Article: Clinical Characteristics and Factors Influencing Prognosis of Patients With Hepatoid Adenocarcinoma of the Stomach in China. Medicine (Baltimore). 95: e3399.
- Yang JZ, Guo XX, Xu C, Hou YY, Yuan W (2024) Clinicopathological features of gastric alpha-fetoprotein-producing adenocarcinoma with SWI/SNF complex deletion. Zhonghua Bing Li Xue Za Zhi. 53: 52-57.
- Li QZ, Zhao HB, Ban N, Wang Q, Zhang JJ, et al. (2020 ) Gastric adenocarcinoma with enteroblastic differentiation and elevated serum alpha fetoprotein. Zhonghua Bing Li Xue Za Zhi. 49: 886-890.
Citation: Damien OZ, Ibrahim S, Léonce ZS, Souleymane S, Delphine NZ, et al. (2026) Diagnostic Challenge of Isolated Alpha-Fetoprotein Elevation: A Case Report. HSOA J Gastroenterol Hepatology Res 9: 059
Copyright: © 2026 Ouattara Zanga Damien, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

