
Direct Brow Lift an Update of Current Literature
*Corresponding Author(s):
Shani GolanDepartment Of Ophthalmology, New York Presbyterian Hospital - Weill Cornell Medical College, New York, United States
Tel:+1 97236973408,
Email:shanigola2@gmail.com
Abstract
Ptosis of the eyebrows is the earliest manifestation of the aging face [1]. It gives the face a tired look and accentuates upper eyelid deformities. There are numerous surgical procedures to lift the brow; the earliest were published in the early 1900s [2-4]. Since the introduction of the direct brow lift technique, there have been minor refinements to this procedure, as well as some major developments in surgical techniques.
Keywords
INTRODUCTION
ANATOMY
The muscle overlies the brow fat pad-the Retro-Orbicular is Oculi Fat pad (ROOF). The ROOF is strongly attached to the superior orbital rimperiosteum.
This ROOF should be distinguished from the pre-aponeurotic fat, which is located posterior to the septum. The supraorbital bundle (nerve and blood vessels) ride above and medial to the midpoint of the superior orbital rim to enter the forehead inside the frontalis muscle.
THE IDEAL BROW POSITION
The brow is normally located above the superior orbital rim in females and at the level of the rim in males. There is a more prominent fat pad and less curvature in men compared to women [9-11].
Westmore et al. [8] described the boundaries of the ideal brow. Medially - the ideal brow begins in the same vertical line as the nasal ala and medial can thus and laterally in ends in an oblique line from the nasal ala to the lateral limbus.
Both medial and lateral ends of the brow should lie in the same horizontal line and the brow’s apex should ideally lie above the lateral limbus.
McKinney et al. [10] measured the minimal distance between the center of the pupil and the apex of the brow and found that in the normal brow this distance should be 2.5 cm on average, if this distance is shorter than the patient has brow ptosis.
Brow ptosis
When brow ptosis occurs, the redundancy of skin in the upper eyelid increases. In particular, ptosis of the lateral brows can cause mechanical eyelid ptosis, as a result of the hooding of the upper eyelid skin. For this reason, it is important to assess the position of the brow in patients who are candidates for upper blepharoplasty, and the amount of eyelid skin to be excised should be determined only after careful consideration of the interplay between the brow position and the upper eyelid skin.
Brow lift surgical options
Pre-operatively the patients should be assessed for skin type, the position, shape and symmetry of the brows, the amount of brow ptosis, the position of the anterior hairline, and the presence of forehead rhytides [13,14].
We will briefly go over the main techniques available today and elaborate extensively on the direct brow lift technique (Table 1).
|
Technique |
Concept |
Pros |
Cons |
|
Trans-blepharoplasty browpexy |
Commonly done together with upper blepharoplasty through the same incision. |
Simple, and has the advantage of placing the wounds within the natural skin crease |
Only limited efficacy and a higher risk of recurrence. |
|
Mid-forehead lift |
Incisions in this technique are preformed in the forehead crease |
Suitable for men with deeper forehead creases and retreating hairlines. |
Visible scarring and altered forehead sensation. |
|
Coronal brow lift |
Involves a long post-trichial incision fromear to ear. |
Allows the surgeon to remove excess forehead skin, fat and tissue while lifting the brow. |
Not suitable for patients that have high hairline or hair that is thinning, as it may cause alopecia. |
|
Pretrichial brow lift |
Incision is created just anterior to the hairline |
Most appropriate for patients with a high forehead. forehead wrinkles can be treated concurrently. |
Visible scarring |
|
Endoscopic brow lift |
Utilizes small incisions to lift the brow endoscopically |
Similar success rates as the coronal brow lift, with a significantly lower rate of complications. |
A long learning curve for surgeon, additional expense of the specialized equipment |
|
Direct brow lifting |
Incisions are made in the superior border of the brow |
The greatest amount of brow lift per millimeter of tissue being excised higher predictability rate (the surgeon has more control on the final brow position and shape) |
Postoperative scar |
This approach is more appropriate for small degrees of brow ptosis that affect mainly the lateral brow. It is commonly done in conjunction with upper eyelid blepharoplasty through the same incision [15]. This procedure is simple, and has the advantage of placing the wound within the natural skin crease. However, it has only limited efficacy and a higher risk of recurrence.
The incisions in this technique are placed in a forehead crease, and thus it is suitable for men with deeper forehead creases and retreating hairlines [16,17]. The potential complications of this procedure are visible scarring and altered forehead sensation.
This approach involves a long incision behind the hairline fromear to ear. It allows the surgeon to also treat forehead and glabellar wrinkles while lifting the brow [18]. It is not suitable for patients that have high hairline or hair that is thinning, as this approach will lengthen the forehead and a potential complication of this technique is alopecia.
The pretrichial incision is created just anterior to the hairline, often in a saw-toothed manner to aid in scar camouflage. This technique is most appropriate for patients with a high foreheads it will lower the hairline. Forehead and glabellar wrinkles can be treated concurrently. Visible scarring is a potential complication of this surgery and it is best hidden in patients who wear their hair with bangs.
This approach utilizes small incisions and has become popular for facial rejuvenation. It has a similar success rate as the coronal brow lift, with a significantly lower rate of complications (numbness, itching, hair loss, tissue swelling) and a faster recovery time [5,6,19-21]. However, this technique has disadvantages that include: A steep learning curve, the additional expense of specialized equipment, and additional surgical time.
The direct brow approach can be used for any pattern and amount of brow ptosis. This approach gives the greatest amount of brow lift per millimeter of tissue being excised. It also has a higher predictability rate and gives the surge on more control on the final brow position and shape. The main disadvantage of this technique is the postoperative scar. The direct brow lift is often reserved for patients with pre-existing deep forehead rhytids, which can help camouflage the scar, or for patients with full and “bushy” brow hairs which can hide the scar from view.
OPERATIVE TECHNIQUE
2. Identify the position of the supraorbital bundle at the medial aspect of the brow.
3. Incision-cut the skin along the marked ellipse. Stay within the ROOF at the medial 1/3rd of the outlined ellipse to protect the supraorbital bundle and deepen the dissection to below the fat layer in the lateral end of the ellipse, to expose the frontalis muscle. Pay close attention to avoid damaging the supraorbital bundle when excising the ellipse of tissue.
4. Closing the wound-careful closure performed in two layers (deep and superficial skin sutures) is the preferred technique as it leads to the most satisfactory cosmetic result. Often, interrupted 4-0 absorbable sutures are used to close the deep layers in a buried fashion. In patients with facial palsy these sutures may also be fixated to the periosteum. Closing the skin is often carried out with 5-0 non-absorbable sutures, taking care to evert the skin edges to allow for a flat, rather than depressed scar [22]. Steri-strip dressings may also be placed along the wound. The skin sutures should be removed after 5-7 days.
EFFICACY AND COMPLICATIONS
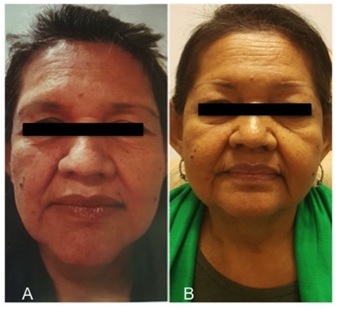
Figure 1: (A) 59 years old patient with a history of involutional bilateral brow ptosis (before) and (B) (1 year after) bilateral direct brow lift.

Figure 2: (A ) 67 years old patient with History of chronic right Bell’s palsy resulting in brow ptosis (before) and (B) (1 year after) right direct brow lift.
Many authors report low complication rates following direct brow lift, however there is no exact quantification [25-27]. Supraorbital nerve trauma and complete loss of sensation in the forehead is one of the reported side effects, however it should be avoidable when careful dissection is employed. Temporary patches of reduced forehead sensation from cutting smaller branches of the nerve can occur and will normally recover in a few months. One report [24] found that 74% of patients had altered sensation over the forehead, but only 7% of those were unhappy about it. Another report [28] found a 27.5% rate of postoperative paresthesia but did not mention if it was transient or permanent.
The postoperative scar in this approach is a major concern to both patients and surgeons. Ueda et al. [28] reported that 77% of patients were satisfied with the cosmesis of the postoperative scar and none of their patients was ‘completely dissatisfied’. Booth et al. found similar high levels of satisfaction, with 81% of their patients reporting being either happy or very happy with the surgical outcome [24]. Unsatisfactory aesthetic outcome is another common patient’s complaint [29-31]. Freund and Nolan reported that both the standard open brow lift and the end oscopic approach result in disappointing eyebrow height and contour.
DISCUSSION
The direct brow lift operation, discussed thoroughly here, remains relevant due to its simplicity. This is a quick procedure, with no need for special equipment or extensive training and it provides reliable and predictable postoperative outcome, with high rates of patient satisfaction. Postoperative complications can be minimized by careful dissection and layered closure.
REFERENCES
- Knize DM (1996) An anatomically based study of the mechanism of eyebrow ptosis. Plast Reconstr Surg 97: 1321-1333.
- Passot R (1919) La chururgie esthetique des rides du visage. Presse Med 27: 258.
- Miller CC (1908) Cosmetic Surgery (2nd edn). Chicago, Ill: Oak Printing and Publishing, Ohio, USA.
- Graham HF (1926) Plastic Surgery of the Head, Face, and Neck. Ann Surg, 84: 911-912.
- Vasconez LO (1992) The use of the endoscope in brow lifting. Video presentation at: Annual Meeting of the American Society of Plastic and Reconstructive Surgeons; Washington, D.C.USA.
- Isse NG (1994) Endoscopic facial rejuvenation: Endoforehead, the functional lift. Case reports. Aesthetic Plast Surg 18: 21-29.
- Gunter JP, Antrobus SD (1997) Aesthetic analysis of the eyebrows. Plast Reconstr Surg 99: 1808-1816.
- Westmore MG (1975) Facial cosmetics in conjunction with surgery. Course presented at the Aesthetic Plastic Surgical Society Meeting, Britis Columbia, Vancouver, Canada.
- Ellenbogen R (1983) Transcoronal eyebrow lift with concomitant upper blepharoplasty. Plast Reconstruct Surg 71: 490-499.
- McKinney P, Mossie RD, Zukowski ML (1991) Criteria for the forehead lift. Aesthetic Plast Surg 15: 141.
- Goldstein SM, Katowitz JA (2005) The male eyebrow: A topographic anatomic analysis. Ophthal Plast Reconstr Surg 21: 285-291.
- Georgescu D, Anderson RL, McCann JD (2010) Brow ptosis correction: A comparison of five techniques. Facial Plast Surg 26: 186-192.
- Maas CS, Kim EJ (2003) Temporal brow lift using botulinum toxin A: An update. Plast Reconstr Surg 112: 109-112.
- Bidros RS, Salazar-Reyes H, Friedman JD (2010) Subcutaneous temporal browlift under local anesthesia: A useful technique for periorbital rejuvenation. Aesthet Surg J 30: 783-788.
- McCord CD, Doxanas MT (1990) Browplasty and browpexy: An adjunct to blepharoplasty. Plast Reconstruct Surg 86: 248-254.
- Rafaty FM, Goode RL, Abramson NR (1978) The brow lift operation in a man. Arch Otolaryngol 104: 69-71.
- Brennan HG (1980) Correction of the ptotic brow. Otolaryngol Clin N Am 13: 265-273.
- Fett DR, Sutcliffe RT, Baylis HI (1983) The coronal brow lift. Am J Ophthalmo l 96: 751-754.
- Steinsapir KD, Shorr N, Hoenig J, Goldberg RA, Baylis HI, et al. (1998) The endoscopic forehead lift. Ophthalmic Plast Reconstruct Surg14: 107-118.
- Holck DEE, Ng JD, Wiseman JB, Foster JA (1998) The endoscopic browlift for forehead rejuvenation. Semin Ophthalmol 13: 149-157.
- Stanek JJ, Berry MG (2014) Endoscopic-assisted brow lift: Revisions and complications in 810 consecutive cases. J Plast Reconstr Aesthet Surg 67: 998-1000.
- Pascali M, Bocchini I, Avantaggiato A, Carinci F, Cervelli V, et al. (2016) Direct brow lifting: Specific indications for a simplified approach to eyebrow ptosis. Indian J Plast Surg 49: 66-71.
- Bidros RS, Salazar-Reyes H, Friedman JD (2010) Subcutaneous temporal browlift under local anesthesia: A useful technique for periorbital rejuvenation. Aesthetic Surgery Journal 30: 783-788.
- Booth AJ, Murray A, Tyers AG (2004) The direct brow lift: Efficacy, complications, and patient satisfaction. Br J Ophthalmol 88: 688-691.
- Green JP, Goldberg RA, Shorr N (1997) Eyebrow ptosis. Int Ophthalmol Clin 37: 97-122.
- Johnson JM, Anderson JR, Katz RB (1979) The brow lift 1978. Arch Otolaryngol 105: 124-126.
- Jarchow RC (1987) Direct browplasty. South Med J 80: 597-600.
- Ueda K, Harii K, Yamada A (1994) Long term follow up study of browlift for treatment of facial paralysis. Ann Plast Surg 32: 166-170.
- Rafaty FM, Goode RL, Abramson NR (1978) The brow lift operation in a man. Arch Otolaryngol 104: 69-71.
- Paul MD (2001) The evolution of the brow lift in aesthetic plastic surgery. Plast Reconstr Surg 108: 1409-1424.
- Freund RM, Nolan WB (1996) Correlation between brow lift outcomes and aesthetic ideals for eyebrow height and shape in females. Plast Reconstruct Surg 97: 1343-1348.
Citation: Golan S, Lelli GJ, Levine B (2019) Direct Brow Lift an Update of Current Literature. J Otolaryng Head Neck Surg 5: 024.
Copyright: © 2019 Shani Golan, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

