Journal of Nuclear Medicine Radiology & Radiation Therapy Category: Medical
Type: Case Report
Dual Parathyroid Pathology; A Common Failure of Technetium-99 Sestamibi Scan for Preoperative Parathyroid Adenoma Localization
*Corresponding Author(s):
Ahmed FathalaDepartment Of Radiology, Nuclear Medicine And Cardiothoracic Imaging, King Faisal Specialist Hospital & Research Center, MBC#28, P.O Box 3354, Riyadh, Saudi Arabia
Tel:+966552532402,
Email:ahm35799@hotmail.com
Received Date: Dec 28, 2016
Accepted Date: Mar 03, 2017
Published Date: Mar 20, 2017
Abstract
Accurate minimally invasive parathyroidectomy for hyperparathyroidism relies on accurate parathyroid adenoma localization. Currently technetium-99m sestamibi parathyroid scan (Tc-99m MIBI) is a technique of choice for preoperative localization. The Tc-99m MIBI is sensitive to detect a single parathyroid adenoma but less useful in double parathyroid adenomas or hyperplasia. In this case we report a patient with primary hyperparathyroidism and coexistence thyroid cancer. Preoperative TC-99m MIBI successfully localized a parathyroid adenoma; subsequently patient underwent surgical removal of left parathyroid adenoma with normalization of parathyroid hormone. Further, the magnetic resonance imaging of the neck and repeated Tc- 99m MIBI parathyroid scan revealed that the second focal parathyroid tissue was removed surgically and through pathology parathyroid hyperplasia was revealed.
Keywords
Parathyroid Pathology
INTRODUCTION
Accurate minimally invasive parathyroidectomy for hyperparathyroidism relies on accurate parathyroid adenoma localization,Technetium-99m sestamibi scintigraphy (TC-99m MIBI scan) both planar and Single-Photon Emission Computed Tomography (SPECT) is useful in the diagnosis of parathyroid gland adenoma, with sensitivity rates of about 90% in Primary Hyperparathyroidism (PHPT) but significantly lower rates in secondary hyperparathyroidism, Currently Tc-99m MIBI scan is the imaging technique of choice for parathyroid adenoma localization [1]. Ultrasound is very useful tool in this setting with or without TC-99m MIBI scan. Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are less commonly used for preoperative localization, and reserved for cases of failed parathyroidectomy, for detection of suspected ectopic gland, or recurrent hyperparathyroidism. The spectrum of parathyroid disease demonstrated with Tc-99m MIBI scintigraphy includes eutopic disease, ectopic disease, solitary adenoma, double or multiple adenomas and other rare parathyroid pathology. However in some clinical cases parathyroid scan is negative and failed to visualise parathyroid adenoma, which is relatively rare in solitary parathyroid adenoma but common in dual parathyroid pathology or polyglandular disorders [2]. We report a case with primary hyperparathyroidism in which the preoperative parathyroid adenoma localization with TC-99m MIBI parathyroid scan was successful and the patient underwent parathyroid adenoma excision with immediate normalization of parathyroid hormone. After two months the patient was diagnosed with recurrent hyperparathyroidism; further imaging with MRI revealed a well-defined oval shaped soft tissue mass within the right paratracheal region of right parathyroid gland, parathyroid scan demonstrated a new parathyroid uptake suggesting a second parathyroid adenoma. Patient underwent exploration with the removal of second parathyroid adenoma and subsequently patient improved the clinical symptoms along with normal calcium levels.
CASE PRESENTATION
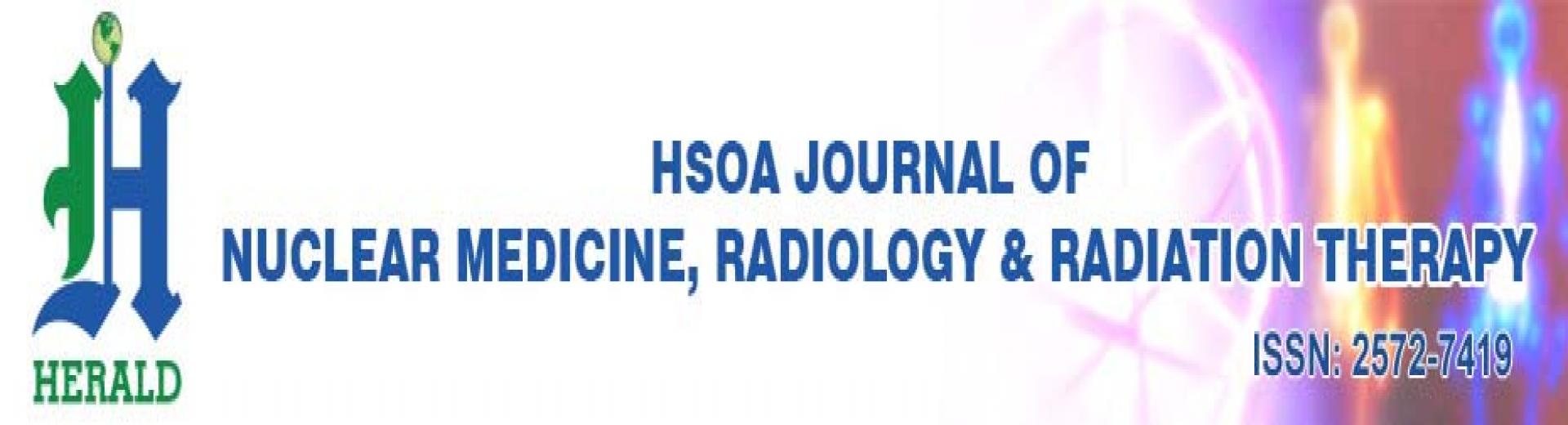
We report a case of 76-year old female who is known to have hypertension and paroxysmal atrial fibrillation well controlled on medications, was diagnosed as a case of primary PHPT based on the following laboratory findings: serum calcium (Ca++) 2.6 mmol/L (2.1-2.5 mmol/L), Phosphorus 1.0 mmol/L (0.9-1.5 mmol/L), PTH 355 ng/L (RR:15-65 ng/L) and vitamin D 80 nmol/L ( 62-199 nmol/L). Technitum-99 sestamibi scintigraphy showed a localized avid uptake in left lower neck that was thought to represent left inferior parathyroid adenoma (Figure 1A-C). In addition, clinical examination showed multi nodular goitre with euthyroid hormones. Thyroid ultrasound showed multiple bilateral thyroid nodules (Figure 1D), Fine Needle Aspiration (FNA) taken from the right thyroid lobe and was suspicious of papillary thyroid cancer. Patient underwent total thyroidectomy in addition to resection of 2 left parathyroid glands. Histopathology proved a moderate risk of papillary thyroid cancer with tall-cell variant and 0.9 cm in size, positive lymph vascular invasion with positive extra thyroid extension with positive extension to margin. The patient tolerated the surgery well, parathyroid hormone was checked and it was coming down. After two months the patient showed hypercalcaemic crisis with calcium of 4.2, phosphorus was 0.61. Neck MRI showed well defined oval shape soft tissue mass with the right paratracheal region and the expected location of right parathyroid gland (Figure 2A). Tc-99m sestamibi scan showed focal tracer retention in the area that corresponds to abnormality noted in the MRI (Figure 2B-D). Patient underwent neck dissection for right parathyroidectomy, PTH level prior to the excision was 595.7ng/L and post excision it was 38.7ng/L. The pathology report showed hyper cellular parathyroid gland suggesting parathyroid hyperplasia. The patient was discharged in a good condition.

Figure 1A: Early anterior planar image of Technium-99m sestamibi scan demonstrates intense tracer uptake in the region of the left thyroid lobe consistent with parathyroid adenoma (arrow).

Figure 1B: Delayed anterior planar image of Technium-99m sestamibi scan demonstrates intense tracer uptake in the region of the left thyroid lobe consistent with parathyroid adenoma (arrow).
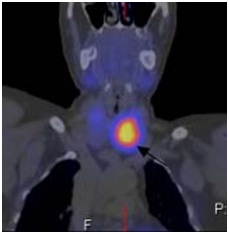
Figure 1C: Coronal sagittal image of SPECT of the neck and upper thorax image show focal intense radiotracer uptake in the lower pole of left thyroid lobe consistent with parathyroid adenoma (arrow).
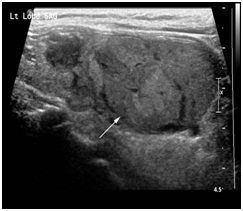
Figure 1D: Sagittal ultrasound scan shows a well-defined, heterogeneous, solid thyroid nodule in left thyroid lobe (arrow) that showed intranodular and peripheral vascularity on colour Doppler scan.
Figure 2A: Coronal T2- weighted magnetic resonance imaging demonstrates T2-high signal intensity well defined soft tissue nodule in the right lower neck (arrow).
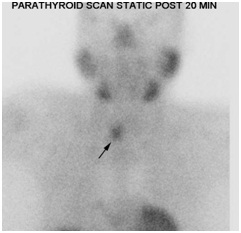
Figure 2B: Early anterior planar image of Technium-99m sestamibi scan shows a possible mild tracer uptake within the inferior region of the right thyroid lobe (arrow).
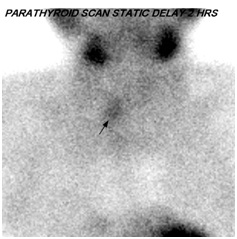
Figure 2C: Delayed anterior planar images of Technium-99m sestamibi scan shows persistent uptake within the inferior region of the right thyroid lobe suggestive of parathyroid adenoma (arrow).

Figure 2D: Coronal sagittal image of SPECT of the neck and upper thorax image shows intense focal radiotracer uptake in the lower pole of thyroid in keeping with parathyroid adenoma (arrow).
DISCUSSION
PHPT is present up to 0.1% of the general population, and it is clinically recognized in patients presenting with hypercalcemia or as a part of Multiple Endocrine Neoplasia (MEN) types I and II a. Although there have been sporadic reports of the coexistence of hyperparathyroidism and non-medullary thyroid carcinoma, concurrence of parathyroid adenoma and papillary thyroid carcinoma is rare. The cause of the association between thyroid disease and primary PHPT remains unclear [3]. The oncogenic effect of hypercalcemia on the thyroid gland has been assumed, and low-dose radiation therapy for the head and neck, especially in childhood and adolescence, is known to induce thyroid and parathyroid tumors [4]. Since the coexistence can complicate patient management via untreated hypercalcemia, unrecognized thyroid cancer and the necessity of re-operative neck surgery patients should be screened for both disease entities carefully. It is advisable to evaluate the thyroid gland prior to parathyroid gland operations. Although synchronous parathyroid and thyroid carcinomas are rare, they can coexist. It is important not only to do biochemical studies, including serum calcium and PTH concentrations but also to carefully interpret imaging studies as preoperative FNAB and ultrasound of the neck may be helpful to evaluate occult primary hyperparathyroidism, enabling surgery to be performed more aggressively and preventing a second operation that might increase morbidity and mortality.
Causes of failure of Tc-99 sestamibi to visualise parathyroid adenoma
The exact mechanism that is MIBI scan is less sensitive for dual parathyroid pathology or polyglandular pathology is uncertain, but there are certain factors that may determine MIBI uptake by parathyroid adenoma, most importantly, adenoma size, adenoma cellular function and system resolution which relies on adenoma size and MIBI uptake. Linero and co-workers showed that MIBI uptake by hyper functioning parathyroid adenoma in PHPH might be linked to a higher gland metabolism activity, probably related to cell proliferation [5]. Same author studied 46 patients with PHPT and confirmed that MIBI sensitivity is adenoma is high (91%) than parathyroid hyperplasia (67%) or double adenoma (50 %). No relation was found between biochemical or cytological parameter and scan results, weight and gland volume were significantly greater for adenoma (p.0014 and p.0004) respectively and statically significant difference between them were observed between glands with positive and negative scan [6]. Turgut B et al., suggested that MIBI scan is clearly superior to ultrasound a diagnostic tool and P-Glycoprotein (P-GP) expression, oxyphilic cell content and tumour volume may not have a main effect on MIBI scan result of parathyroid adenoma [7]. Sun and co-workers found that large parathyroid adenoma that express (P-GP) or the multi resistance related protein failed to accumulate MIBI [8]. Katz et al., found that MIBI scan failed to identify the presence of bilateral lesions in 13 patients out of 15 patients with multinodular lesions [9,10]. This fact indicates that in the era of the minimally invasive parathyroidectomy, preoperative MIBI imaging cannot be the sole basis on which the decision to perform limited cervical exploration.
In summary this case demonstrates coexistence of parathyroid adenoma and unrecognized thyroid cancer and the necessity to evaluate the thyroid gland prior to parathyroid gland surgery. Most importantly Tc-99m MIBI scans valuable in preoperative localization of parathyroid adenoma and less useful for detecting parathyroid hyperplasia. In recurrent or resistant hyperparathyroidism considering cross sectional imaging such as MRI with or without repeated Tc-99m MIBI scan is helpful in localizing parathyroid adenoma or hyperplasia.
In summary this case demonstrates coexistence of parathyroid adenoma and unrecognized thyroid cancer and the necessity to evaluate the thyroid gland prior to parathyroid gland surgery. Most importantly Tc-99m MIBI scans valuable in preoperative localization of parathyroid adenoma and less useful for detecting parathyroid hyperplasia. In recurrent or resistant hyperparathyroidism considering cross sectional imaging such as MRI with or without repeated Tc-99m MIBI scan is helpful in localizing parathyroid adenoma or hyperplasia.
REFERENCES
- Shah S, Win Z, Al-Nahhas A (2008) Multimodality imaging of the parathyroid glands in primary hyperparathyroidism. Minerva Endocrinol 33: 193-202.
- Ruda JM, Hollenbeak CS, Stack BC Jr (2005) A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg 132: 359-372.
- Fraser WD (2009) Hyperparathyroidism. Lancet 374: 145-158.
- Stephen AE, Chen KT, Milas M, Siperstein AE (2004) The coming of age of radiation-induced hyperparathyroidism: evolving patterns of thyroid and parathyroid disease after head and neck irradiation. Surgery 136: 1143–1153.
- Piñero A, Rodríguez JM, Martínez-Barba E, Canteras M, Stiges-Serra A, et al. (2003) Tc99m-sestamibi scintigraphy and cell proliferation in primary hyperparathyroidism: a causal or casual relationship? Surgery 134: 41-44.
- Piñero A, Rodriguez JM, Ortiz S, Soria T, Bermejo J, et al. (2000) Relation of biochemical, cytologic, and morphologic parameters to the result of gammagraphy with technetium 99m sestamibi in primary hyperparathyroidism. Otolaryngol Head Neck Surg 122: 851-855.
- Turgut B, Elagoz S, Erselcan T, Koyuncu A, Dokmetas HS, et al. (2006) Preoperative localization of parathyroid adenomas with technetium-99m methoxyisobutylisonitrile imaging: relationship with P-glycoprotein expression, oxyphilic cell content, and tumoral tissue volume. Cancer Biother Radiopharm 21: 579-590.
- Sun SS, Shiau YC, Lin CC, Kao A, Lee CC (2001) Correlation between P-glycoprotein (P-gp) expression in parathyroid and Tc-99m MIBI parathyroid image findings. Nucl Med Biol 28: 929-933.
- Katz SC, Wang GJ, Kramer EL, Roses DF (2003) Limitations of Technetium 99m Sestamibi Scintigraphic Localization for Primary Hyperparathyroidism Associated with Multiglandular Disease. Am Surg 69: 170-175.
- Witteveen JE, Kievit J, Stokkel MP, Morreau H, Romijn JA, et al. (2011) Limitations of Tc99m-MIBI-SPECT Imaging Scans in Persistent Primary Hyperparathyroidism. World J Surg 35: 128-139.
Citation: Aboualkheir MM, Fathala A (2017) Dual Parathyroid Pathology; A Common Failure of Technetium-99 Sestamibi Scan for Preoperative Parathyroid Adenoma Localization. J Nucl Med Radiol Radiat Ther 2: 006.
Copyright: © 2017 Ahmed Fathala, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Journal Highlights
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!
