Effect of Acupuncture on Oxidative Stress and Inflammation: From Mechanisms to Therapeutic Applications
*Corresponding Author(s):
Tzu-Hsuan WeiDepartment Of Chinese Medicine, China Medical University Hospital, Taichung, Taiwan
Email:krultepes463@gmail.com
Abstract
Inflammation is a common feature of disorders affecting various systems in the body, and oxidative stress can lead to an imbalance in the cellular metabolism and impaired regeneration of injured tissue. The therapeutic effect of manual acupuncture and electroacupuncture has long been studied. In this study, we conducted a literature review focusing on oxidative stress and inflammation and the therapeutic effect of acupuncture on pathological pathways. Our results reveal that through a novel light therapy technique, manual acupuncture and electroacupuncture can be combined to provide an alternative method for optimizing their therapeutic effects.
Keywords
Acupuncture; Anti-inflammatory; Antioxidative; Immunomodulation; Laser; Oxidative stress; Photobiomodulation; Re-generation
Abbreviations
Akt: protein kinase B
AP-1: Activator Protein 1
ATP: Adenosine Triphosphate
CREB: cAMP-Response Element–Binding
CRT: Chemo-Radiotherapy
CcO: Cytochrome c Oxidase
COX: Cyclooxygenase
ERK: Extracellular Signal-Regulated Kinases
EP2/4: prostaglandin E2 receptor 2/4
Grxs/GSH-GSSG: glutathione/glutaredoxin systems
IL: Interleukin
IR: Infrared
JNK: Jun Amino-Terminal Kinases
LLLT: Low-Level Laser Therapy
MAPK: Mitogen-Activated Protein Kinase
mETC: mitochondrial Electron Transport Chain
MAO: Monoamine Oxidase
NADPH: Nicotinamide Adenine Dinucleotide Phosphate
NF-κB: Nuclear Factor Kappa B
NIR: Near Infrared
NO: Nitric Oxide
NOX: Nicotinamide Adenine Dinucleotide Phosphate Oxidases
PBM: Photobiomodulation
PI3K: Phosphoinositide 3-kinases; also called phosphatidylinositol 3-kinases
Prx: Peroxiredoxin
PKC: Protein Kinase C
RCT: Randomized Control Trial
ROS: Reactive Oxygen Species
RT: Radio Therapy
SOD: Superoxide Dismutase
TENS: Transcutaneous Electrical Nerve Stimulation
TGF: Transforming Growth Factor
TNF-α: Tumor Necrosis Factor-Alpha
TRPV1: Transient Receptor Potential Vanilloid 1
TRX: Thioredoxin
Introduction
Acupuncture is a form of clinical management that has been gaining recognition for its therapeutic effects, which include pain control [1], immunomodulation [1-3], homeo-static regulation [1,4,5] and antidegeneration [1,6]. Meridian theory, which was first described in The Yellow Emperor’s Classic of Internal Medicine, is a key theory guiding the medical practice of acupuncture. The “meridians,” also called “channels,” are networks spreading throughout the body, allowing organs and tissues to communicate with each other and producing a dynamic balance in the body as a biosystem. Studies have revealed the neuroanatomical basis of the therapeutic effects of acupuncture, demonstrating that most acupoints are located on or adjacent to peripheral nerve trunks or branches, capillary vessels, blood vessels, lymphatic vessels, nerve receptors, nerve endings, or mast cells. The meridians correspond to the trajectories of relevant deep peripheral nerves, including blood vessels, and stimulation at the acupoints creates the synaptic afferent input to a particular spinal or thalamic neuron, known as the receptive field [4]. Moreover, molecular evidence of electroacupuncture’s influence on the vagal–adrenal axis has been used to explain the anti-inflammatory effect of acupuncture [4]. Low-intensity laser acupuncture has been used for asthma management, revealing acupuncture’s immuno-modulatory effect and its ability to adjust the ratio between the oxidant and antioxidant systems and normalize respiratory function parameters [7].
In this study, we focused on oxidative stress and inflammation, which play a key role in the development of diseases, and the therapeutic effect of acupuncture on pathological pathways. A combination of the classical theory of acupuncture and new acupoint stimulation techniques provides numerous possibilities for the application of acupuncture in clinical management.
Materials and Methods
The authors electronically searched for articles reporting the Results of randomized Controlled Trials (RCTs), systematic reviews, and meta-analyses on the PubMed database by using the following keywords alone or in various combinations: “oxidative stress,” “acupuncture,” “mechanism,” “intravenous laser irradiation,” and “photobiomodultion.” English articles published between 2013 and November 2021 with available full texts were included in the study.
Results
In total, 415 full-text articles reporting RCTs, systemic reviews, and meta-analyses were identified; 354 articles were excluded on the basis of the title and abstract, because of the RCT protocols employed, or because they were identified as identical or similar to other articles upon a reading of the full text. Two additional articles were included after searching the reference lists of the identified articles. Of the 63 articles included, 5 included a systematic review and meta-analysis in the same article and were thus excluded as duplications. Consequently, 58 articles were included in our literature review.
Oxidative Stress and Inflammation in the Development of Pathological Changes
Reactive oxygen species (ROS) serve as cell signaling molecules for normal biologic processes. However, ROS generation can also damage multiple cellular organelles and hamper processes, which can disrupt normal physiology. Knowledge of the pathophysiology underlying several nervous system diseases, such as dementia, epilepsy, and Parkinson disease, is increasing, clarifying its relationship with chronic inflammation and the impairment of cell regeneration [1]. A common feature of system disorders, such as cancer, asthma, hypertension, obesity, depression, and schizophrenia, is the central role of inflammation and oxidative stress [8]. An imbalance between the production of ROS and the antioxidant defenses that protect cells has been identified in the pathological changes of various tissues and organ systems (Figure 1). The nature of the injury ultimately depends on specific molecular interactions, cellular locations, and the timing of the injury.
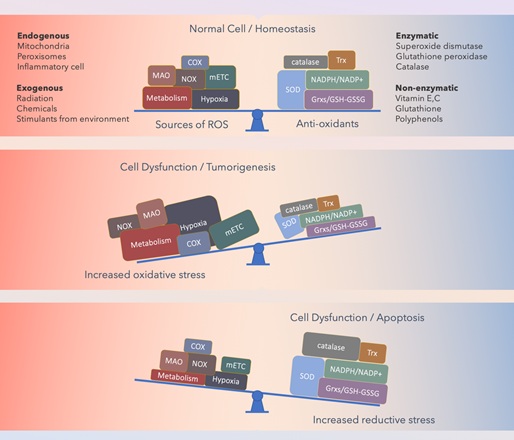 Figure 1: Schematic of the dynamic redox balance of cells.
Figure 1: Schematic of the dynamic redox balance of cells.
Typically, a dynamic redox balance exists between oxidative stress and reductive systems in cells to maintain cellular viability. An altered redox balance and deregulated redox signaling is involved in the progression of malignancies and resistance to treatment (e.g., chemotherapy for cancer). A high Reactive Oxygen Species (ROS) level often indicates genetic-, metabolic-, and microenvironment-associated alterations. The consequences of increased oxidative stress are determined by the antioxidant ability of the affected cell. Abbreviations: cyclooxygenase, COX; glutathione/glutaredoxin systems, Grxs/GSH-GSSG; mitochondrial electron transport chain, mETC; monoamine oxidase, MAO; nicotinamide adenine dinucleotide phosphate, NADPH; nicotinamide adenine dinucleotide phosphate oxidases, NOX; peroxiredoxin, Prx; superoxide dismutase, SOD; thioredoxin, TRX.
Low concentrations of ROS affect many cellular metabolism processes, including the activation of key transcription factors, such as nuclear factor kappa B (NF-κB). This results in the expression of stimulatory and protective genes, which generate growth factors belonging to the fibroblast growth factor family, proinflammatory cytokines, and chemokines involved in tissue repair [3]. In hypoxic or otherwise stressed cells, mitochondria produce Nitric Oxide (NO), which binds to Cytochrome c Oxidase (CcO) and displaces oxygen [3], inhibiting cellular respiration and reducing Adenosine Triphosphate (ATP) production. ATP is the universal energy source in living cells; it is essential for all biologic reactions, and even a small increase in ATP levels can enhance bioavailability to power the functions of cellular metabolism [3]. By contrast, a decrease in ATP contributes to the accumulation of oxidative stress, a state that develops when the levels of ROS exceed the defense mechanisms. Oxidative stress then activates the intracellular signaling pathway, involving several intranuclear transcription factors: redox factor-1, activator protein-1, NF-κB, p53, the activating transcription factor and cAMP-Response Element–Binding (CREB) protein, hypoxia-inducible factor-1, and the HIF-like factor [1,3]. These transcription factors induce the downstream production of both inflammatory mediators, such as tumor necrosis factor-alpha (TNF-α), interleukin (IL)-1 and IL-6, COX-2, and prostaglandin E2, and anti-inflammatory mediators, such as transforming growth factor (TGF)-β and IL-10 [1,3].
Moreover, noxious stimulation can rapidly stimulate protein kinase C, resulting in the translocation of this molecule from the intracellular compartments to the plasma membrane. The p38α mitogen-activated protein kinase (MAPK) was first recognized for its role in inflammation, regulating the biosynthesis of the proinflammatory cytokines IL-1 and TNFα [1]. Inflammation is induced through the activation of these cytokines, after which they interact with cognate receptors through the small GTPases [1]. Consequently, chronic pain develops when activated p38 continues to increase in the spinal cord and dorsal root ganglion neurons, where it phosphorylates transcription factors and proinflammatory cytokines and propagates pain signals [1]. Another clinical factor in cancer management is the chronic sequelae of Radiotherapy (RT) and Chemoradiotherapy (CRT). An excessive fibroblastic response has been hypothesized to be related to acute oxidative injury, contributing to extensive cell damage, ischemia, and an ongoing inflammatory response resulting in fibrosis [2,3].
Reduction of oxidative stress and inflammation through acupuncture
During acupuncture, a physician inserts a thin and sterilized metal needle into the skin at specific acupoints and manipulates the needle to achieve “de qi” status (a status of which accounts that acupuncture has achieve therapeutic dose of stimulation). In addition to conventional manual acupuncture, novel methods for stimulating acupoints have emerged, enabling a growing range of therapeutic applications. For example, electro-acupuncture and Transcutaneous Electrical Nerve Stimulation (TENS) applied to acupoints are used to manage neuralgia [1,4,5], migraine [6], soft tissue injuries [2], osteoarthritis [1], poststroke rehabilitation [1,7,9] and functional dyspepsia [10].
Studies have revealed that most acupoints are located on or adjacent to peripheral nerve trunks or branches, capillary vessels, blood vessels, lymphatic vessels, nerve receptors, nerve ending, or mast cells [11]. One of the mechanisms of acupuncture involves enabling multireceptive neurons to receive convergent signals from the skin, muscles, and visceral synapses, thus influencing individual spinal neurons. Therefore, manipulating needles at specific acupoints can trigger a cascade of signal transduction, especially spinal neuron receptive fields, and also affect the neuroendocrine system through ascending neural pathways [11,12].
At a molecular level, acupuncture can regulate multiple signal pathways, including the p38 MAPK, Raf/MAPK/extracellular signal-regulated kinases (ERK) 1 and 2, toll-like receptor 4/ERK, phosphatidylinositol-4,5-bisphosphate 3-kinase/protein kinase B, adenyl cyclase/cyclic-adenosine mono-phosphate (cAMP)/protein kinase A (PKA), apoptosis signal-regulating kinase 1 (ASK1)-c-Jun amino-terminal kinases (JNK)/p38, and down-stream CREB, JNK, mammalian target of rapamycin (mTOR), NF-κB, and B-cell lymphoma 2/ Bcl-2-associated X Bax balance pathways [1]. For example, reversing the detrimental effect of cerebral ischemic or hemorrhagic injury involves modulating the ERK/JNK/p38 signal pathway, which has an antiapoptosis effect on the brain area. Improvements in Alzheimer disease, vascular dementia, and Parkinson disease also involve the regulation of the p38 MAPK pathway [1]. The inactivation of IL-1β/p38 in the frontal lobe and hippocampus has a positive effect on cognition and memory. Moreover, acupuncture has an analgesic effect through the stimulation of both ascending and descending pain signaling pathways [1].
Notably, an RCT study demonstrated that different neurobiological mechanisms are triggered during the application of TENS management only and “acupuncture-like” TENS (applying electrical nerve stimulation to acupoints with the guidance of meridian theory), resulting in distinct analgesic effects [4]. The analgesic effect of TENS was maximal when nociceptive stimuli were delivered unilaterally (i.e., to the same hand that received the TENS); by contrast, acupuncture-like TENS produced a spatially diffuse analgesic effect, coupled with long-lasting changes both in the state of the primary sensorimotor cortex (S1/M1) and the functional connectivity between S1/M1 and the medial prefrontal cortex, a core region in the descending pain inhibitory system [4].
Combining photobiomodulation and acupuncture to reduce oxidative stress and inflammation
The discovery of the biomodulation effect allows physicians to use various wavelengths of a low-level laser to achieve beneficial effects, such as promoting cell regeneration, wound healing, anti-inflammation, and blood circulation and improving edema in patients with cancer following RT and CRT [2,13]. Optostimulation, using blue-light pulses on acupoint ST36 (“Zusanli” in Chinese; an acupoint located below the knee on the tibialis anterior muscle, along the stomach meridian), has also been reported to reduce TNF and IL-6 production by 50% and increase noradrenaline, adrenaline, and dopamine serum levels in animal models compared with a control group [5,12,14-16].
A large body of evidence exists that supports the efficacy of low-level laser therapy, more recently termed photobiomodulation (PBM), for both the combined and postradiation management of several cancers, including head and neck cancer [2,3,17,18] and breast cancer [19]. Studies have reported that acupuncture is beneficial for symptom management in patients with cancer; these symptoms include pain, nausea, hot flushes, fatigue, radiation-induced xerostomia, prolonged postoperative ileus, anxiety and mood disorders, and sleep disturbance [20-22]. The aforementioned studies have highlighted promising clinical applications of the use of PBM combined with meridian theory for selecting the site for laser stimulation.
PBM is the therapeutic use of light to transduce energy into the tissue and cells. Near Infrared (NIR) and Infrared (IR) are visible light that can be absorbed by endogenous chromophores, triggering nonthermal and noncytotoxic biological reactions through photochemical or photophysical events. Current evidence suggests that PBM acts pre-dominantly on CcO in the mitochondrial respiratory chain by facilitating electron transport, resulting in an increased transmembrane proton gradient that drives ATP production [3,23]. The absorption of IR or NIR light triggers a transient burst of ROS, followed by an adaptive reduction in oxidative stress; the activated TGF-β1 also participates in mitigating the inflammation, thereby effectively reducing pain and leading to tissue regeneration [3,24-28]. PBM has also been referred to as a “low-level laser” because the light is of relatively low intensity compared with other forms of medical laser treatment for ablation, cutting, and coagulation [3].
Evidence suggests that when PBM is administered with appropriate parameters to stressed cells, NO is dissociated from its competitive binding to CcO, thus reducing oxidative stress; consequently, ATP production is increased, and the balance between pro-oxidant and antioxidant mediators is restored [3,28-31]. PBM has been demonstrated to attenuate the production of ROS through human neutrophils [3] and reduce ROS in traumatic tissue injuries in an animal model, and a study of an acute lung inflammation model revealed that PBM reduces the generation of TNF-α and increases IL-10 [3,28,29]. In addition, NO is a potent vasodilator and can increase the blood supply to the light-stimulated tissue. PBM-mediated vascular regulation increases tissue oxygenation and promotes the gathering and function of immune cells, which may contribute to repair and regeneration [3,24,25,28-36]. Moreover, in vivo studies have demonstrated that PBM is neuroprotective and may benefit neurodegenerative diseases and neurotrauma [3,25,37-41].
PBM’s biological effects are closely dose-related, and an optimal parameter setting is required to achieve a therapeutic effect [3,25,41-53]. For example, irradiating soft tissue using a 632–635-nm diode laser enhances tissue repair and regeneration [49-51,53] and an 830-nm diode laser reduces pain at trigger points but without influencing the function of muscle rigidity [54]. PBM with a relatively high-power density (>300 mW/cm2), when absorbed by nociceptors, has an inhibitory effect on A and C fibers, the neural fibers that conduct pain signals. PBM at this stimulation intensity slows neural conduction velocity, reduces the amplitude of compound action potentials, and suppresses neurogenic inflammation [3,48].
Few eligible articles reporting RCTs clearly described laser acupuncture management. Nonetheless, a report on a Russian study detailed the application of laser acu-puncture in bronchial asthma management, including the wavelength used, treatment frequency, and outcomes [55]. Hyperviscosity syndrome has been reported to occur in patients with bronchial asthma, and normalizing hemodynamics, recovering microcirculation, and restoring a normal ratio between the immune cells and cytokine levels (e.g., IgA, IgG, and IgE) is crucial during remission. The aforementioned study demonstrated that the optimal time for local exposure in treating patients with allergic bronchial asthma using a pulsed IR low-intensity laser (890-nm wavelength, 5–7 W, 700–1600 Hz) is 60 s (paravertebrally) and 300 s (supraclavicular region) [55]. The following acupuncture points were used: BL10 (Tianzhu), BL11 (Dazhu), BL13 (Feishu), BL12 (Fengmen), BL15 (Xinshu), BL17 (Geshu), RN22 (Tiantu), RN21 (Xuanji), RN20 (Huagai), RN17 (Shan-chung), RN16 (Zhongting), RN15 (Jiuwei), SP6 (Sanyinjiao), ST14 (Kufang), ST15 (Wuyi), ST36 (Zusanli), LI4 (Hegu), LU (Lieque), and LU11 (Shaoshang). The auricular points were AAP55 (Shen Men point), AAP31 (Ping Chuan, asthma point), and AAP13 (adrenal control point). As a result of this treatment, general and local eosinophilia and cutaneous and local sensitivity to specific allergens were reduced. The positive clinical effect of the therapy was accompanied by immune normalization: T-lymphocyte and T-helper cell counts significantly increased, the level of IgA and IgG increased, and the percentage of degranulated mast cells decreased [55].
Moreover, laser acupuncture was reported to enhance molecular membrane rearrangements by reducing cholesterol and the fatty acid saturation factor, increasing the portion of phospholipids, and reducing microviscosity [55]. Functional modification in cells, such as increasing the phagocytic index and neutrophil count, was also reported [55]. These effects contribute to restoring the oxygen transport function of the blood as well as the balance of immune cells ratios.
Mechanism and effects of intravanous laser irradiation
Intravascular Laser Irradiation of Blood (ILIB) therapy involves the use of a helium–neon laser at a wavelength of 632.8 nm (red light), which is transmitted through an optical fiber using a phlebotomy cannula. This treatment has biomodulatory effects that reduce inflammation, regulate the immunologic response, improve the rheological behavior of blood, and simulate antioxidant enzymatic activities [56]. ILIB is also used as an alternative treatment for various diseases, including chronic spinal cord injury, cognitive impairment, cerebral stroke, traumatic brain injury, rheumatoid arthritis, fibromyalgia, and chronic pain. A common feature of these diseases is impaired blood circulation and hypoxia in the affected tissue or organ [56]. Similar to PBM, ILIB is a form of light therapy that enhances ATP synthesis through the spectral absorption of CcO in the mitochondrial respiratory chain [56].
Laser energy at 630–640 nm has been reported as the most effective wavelength for ILIB because photons at this wavelength are absorbed by oxygen, improving microcirculation, which changes the viscosity of the blood and affects the vascular endothelium [57]. Another study using a diabetic rat model revealed that ILIB with constant and shorter wavelengths, such as blue (λ = 450 nm), was more effective than longer wavelengths, such as red (λ = 638 nm) and IR (λ = 808 nm), at lowering the IL level [58] (Figure 2).
 Figure 2: Summary of oxidative stress and the effects of electroacupuncture and laser irradiation therapy.
Figure 2: Summary of oxidative stress and the effects of electroacupuncture and laser irradiation therapy.
Acupuncture and electroacupuncture can regulate multiple signal pathways and reduce the production and action of inflammatory mediators. Laser irradiation acts on the cytochrome c oxidase in the mitochondria and increases ATP production, this lowering oxidative stress. Abbreviations: protein kinase B, Akt; activator protein 1, AP-1; prostaglandin E2 receptor 2/4, EP2/4; phosphoinositide 3-kinases are also called phosphatidylinositol 3-kinases, PI3K; transient receptor potential vanilloid 1, TRPV1.
Discussion
Manual acupuncture and electroacupuncture are performed by inserting a needle into the skin as deep as the muscle layers, depending on the selected acupoint. Physicians perform manipulation to enhance the stimulation of the acupoint and related meridians for a therapeutic effect. Evidence suggests that acupuncture has local and systemic effects on the nervous system and also has immunomodulatory effects. At a molecular level, acupuncture’s therapeutic mechanism involves regulation of intracellular metabolism and cell proliferation. Because oxidative stress and inflammation play a key role in the development of diseases, an early prophylactic application of acupuncture may offer advantages in clinical management. The many studies and associated variables and covariables assessed in this study revealed a number of acupuncture and acupoint stimulation methods.
With regard to laser acupuncture, although the therapeutic effects are unclear when applied alone, this method can be useful as a prophylactic or as a complement to conventional treatment. Moreover, associated wavelengths and several further factors, including the site of irradiation, should be considered when identifying the optical parameters. The available evidence indicates that laser acupuncture provides therapeutic benefits by transducing the stimulation using specific lights into the soft tissues, blood, and immune cells; thus, the site selected for irradiation should be rich in these tissues and organelles. However, risks remain because soft tissues rich in vascular, lymphatic, or nerve-ending structures are susceptible to injury from overstimulation. We therefore recommend that only trained physicians use laser acupuncture to optimize the clinical effects and ensure the safety of the procedure.
Conclusion
Studies have demonstrated the considerable potential of combining the clinical application of acupuncture with PBM for optimizing acupuncture’s therapeutic effects.
Author's Contribution
Articles searching, manuscript writing, and original draft preparation, T-H W; supervising and editing C-L H.
Funding
This study was financially supported by the Chinese Medicine Research Center, China Medical University from the Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education in Taiwan (CMRC-CENTER-0).
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
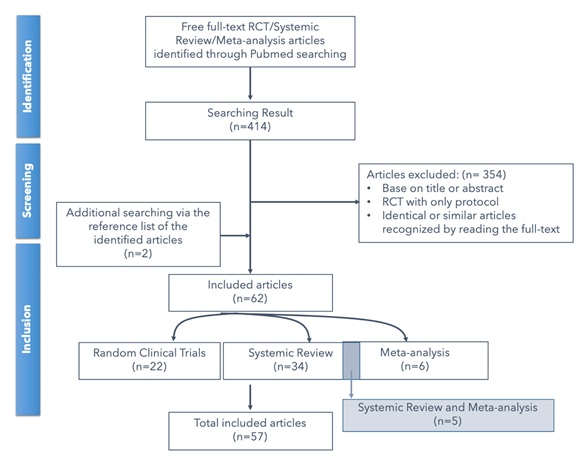
Schematic of the literature review search process
References
- Wei TH, Hsieh CL (2020) Effect of Acupuncture on the p38 Signaling Pathway in Several Nervous System Diseases: A Systematic Review. Int J Mol Sci 21:
- Cronshaw M, Parker S, Anagnostaki E, Mylona V, Lynch E, et al. (2020) Photobiomodulation and Oral Mucositis: A Systematic Review. Dent J (Basel) 8: 87.
- Zecha JA, Durlacher JER, Nair RG, Epstein JB, Sonis ST, et al. (2020) Safety and efficacy of photobiomodulation therapy in oncology: A systematic review. Cancer Med 9: 8279-8300.
- Peng WW, Tang ZY, Zhang FR, Li H, Kong YZ, et al. (2019) Neurobiological mechanisms of TENS-induced analgesia. Neuroimage 195: 396-408.
- Maeda Y, Kim H, Kettner N, Kim J, Cina S, et al. (2017) Rewiring the primary somatosensory cortex in carpal tunnel syndrome with acupuncture. Brain 140: 914-927.
- Li Z, Zeng F, Yin T, Lan L, Makris N, et al. (2017) Acupuncture modulates the abnormal brainstem activity in migraine without aura patients. Neuroimage Clin 15: 367-375.
- Chavez LM, Huang SS, Donald IM, Lin JG, Lee YC, et al. (2017) Mechanisms of Acupuncture Therapy in Ischemic Stroke Rehabilitation: A Literature Review of Basic Studies. Int J Mol Sci 18: 2270.
- Guo C, Sun L, Chen X, Zhang D (2013) Oxidative stress, mitochondrial damage and neurodegenerative diseases. Neural Regen Res 8: 2003-2014.
- Du Y, Zhang L, Liu W, Rao C, Li B, et al. (2020) Effect of acupuncture treatment on post-stroke cognitive impairment: A randomized controlled trial. Medicine (Baltimore) 99: 23803.
- Guo Y, Wie W, Chen JD (2020) Effects and mechanisms of acupuncture and electroacupuncture for functional dyspepsia: A systematic review. World J Gastroenterol 26: 2440-2457.
- González SQ, Castillo ST, Gómez RET, Estrada IJ (2017) Acupuncture Points and Their Relationship with Multireceptive Fields of Neurons. J Acupunct Meridian Stud 10: 81-89.
- Liu S, Wang Z, Su Y, Qi L, Yang W, et al. (2021) A neuroanatomical basis for electroacupuncture to drive the vagal–adrenal axis. Nature 598: 641-645.
- Zein R, Selting W, Hamblin MR (2018) Review of light parameters and photobiomodulation efficacy: dive into complexity. J Biomed Opt 23: 1-17.
- Moskvin SV, Khadartsev AA (2020) Methods of effective low-level laser therapy in the treatment of patients with bronchial asthma (literature review). Biomedicine (Taipei) 10: 1-20.
- Hou S, Huh B, Kim HK, Kim KH, Abdi S (2018) Treatment of Chemotherapy-Induced Peripheral Neuropathy: Systematic Review and Recommendations. Pain Physician 21: 571-592.
- Milstein DM, Genot MT, Lansaat L, Brink R, Dominguez JA, et al. (2016) Low level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: part 1: mechanisms of action, dosimetric, and safety considerations. Support Care Cancer 24: 2781-2792.
- Bardellini E, Amadori F, Conti G, Majorana A (2019) Efficacy of the photobiomodulation therapy in the treatment of the burning mouth syndrome. Med Oral Patol Oral Cir Bucal 24: 787-791.
- Baxter GD, Liu L, Petrich S, Gisselman AS, Chapple C, et al. (2017) Low level laser therapy (Photobiomodulation therapy) for breast cancer-related lymphedema: a systematic review. BMC Cancer 17: 833.
- Garcia MK, Quade JM, Haddad R, Patel S, Lee R, et al. (2013) Systematic review of acupuncture in cancer care: a synthesis of the evidence. J Clin Oncol 31: 952-960.
- Chien TJ, Hsu CH, Liu CY, Fang CJ (2017) Effect of acupuncture on hot flush and menopause symptoms in breast cancer- A systematic review and meta-analysis. PLoS One 12: 0180918.
- Rudayni AHMA, Gopinath D, Maharajan MK, Veettil SK, Menon RK (2021) Efficacy of Photobiomodulation in the Treatment of Cancer Chemotherapy-Induced Oral Mucositis: A Meta-Analysis with Trial Sequential Analysis. Int J Environ Res Public Health 18: 7418.
- Cardoso FDS, Martins RÁBL, Silva SG (2020) Therapeutic Potential of Photobiomodulation In Alzheimer's Disease: A Systematic Review. J Lasers Med Sci 11: 16-22.
- Brochado FT, Jesus LH, Carrard VC, Freddo AL, Chaves KD, et al. (2018) Comparative effectiveness of photobiomodulation and manual therapy alone or combined in TMD patients: a randomized clinical trial. Braz Oral Res 32: 50.
- Keskiner I, Lutfioglu M, Aydogdu A, Saygun NI, Serdar MA (2016) Effect of Photobiomodulation on Transforming Growth Factor-β1, Platelet-Derived Growth Factor-BB, and Interleukin-8 Release in Palatal Wounds After Free Gingival Graft Harvesting: A Randomized Clinical Study. Photomed Laser Surg 34: 263-271.
- Markowitz SN, Devenyi RG, Munk MR, Croissant CL, Tedford SE et al. (2020) A Double-masked, Randomized, Sham-controlled, Single-center Study With Photobiomodulation For The Treatment Of Dry Age-related Macular Degeneration. Retina 40: 1471-1482.
- Hanna R, Dalvi S, Bensadoun RJ, Benedicenti S (2021) Role of Photobiomodulation Therapy in Modulating Oxidative Stress in Temporomandibular Disorders. A Systematic Review and Meta-Analysis of Human Randomised Controlled Trials. Antioxidants (Basel) 10: 1028.
- Liebert A, Krause A, Goonetilleke N, Bicknell B, Kiat H (2017) A Role for Photobiomodulation in the Prevention of Myocardial Ischemic Reperfusion Injury: A Systematic Review and Potential Molecular Mechanisms. Sci Rep 77: 42386.
- Nejatifard M, Asefi S, Jamali R, Hamblin MR, Fekrazad R (2021) Probable positive effects of the photobiomodulation as an adjunctive treatment in COVID-19: A systematic review. Cytokine 137: 155312.
- Santos SAD, Serra AJ, Stancker TG, Simões MCB, Vieira DS, et al. (2017) Effects of Photobiomodulation Therapy on Oxidative Stress in Muscle Injury Animal Models: A Systematic Review. Oxid Med Cell Longev 2017: 5273403.
- Matos BTL, Buchaim DV, Pomini KT, Barbalho SM, Guiguer EL, et al. (2021) Photobiomodulation Therapy as a Possible New Approach in COVID-19: A Systematic Review. Life (Basel) 11: 580.
- Rosso MPO, Buchaim DV, Pomini KT, Coletta BBD, Reis CHB, et al. (2019) Photobiomodulation Therapy (PBMT) Applied in Bone Reconstructive Surgery Using Bovine Bone Grafts: A Systematic Review. Materials (Basel) 12: 4051.
- Suh S, Choi EH, Mesinkovska NA (2020) The expression of opsins in the human skin and its implications for photobiomodulation: A Systematic Review. Photodermatol Photoimmunol Photomed 36: 329-338.
- Jagdeo J, Austin E, Mamalis A, Wong C, Ho D, et al. (2018) Light-emitting diodes in dermatology: A systematic review of randomized controlled trials. Lasers Surg Med 50: 613-628.
- Tripodi N, Feehan J, Husaric M, Sidiroglou F, Apostolopoulos V (2021) The effect of low-level red and near-infrared photobiomodulation on pain and function in tendinopathy: a systematic review and meta-analysis of randomized control trials. BMC Sports Sci Med Rehabil 13: 91.
- Wan Z, Zhang P, Lv L, Zhou Y (2020) NIR light-assisted phototherapies for bone-related diseases and bone tissue regeneration: A systematic review. Theranostics 10: 11837-11861.
- Rosso MPO, Buchaim DV, Kawano N, Furlanette G, Pomini KT, et al. (2018) Photobiomodulation Therapy (PBMT) in Peripheral Nerve Regeneration: A Systematic Review. Bioengineering (Basel) 5: 44.
- Salehpour F, Hamblin MR (2020) Photobiomodulation for Parkinson's Disease in Animal Models: A Systematic Review. Biomolecules 10: 610.
- Firoozi P, Keyhan SO, Kim SG, Fallahi HR (2020) Effectiveness of low-level laser therapy on recovery from neurosensory disturbance after sagittal split ramus osteotomy: a systematic review and meta-analysis. Maxillofac Plast Reconstr Surg 42: 41.
- Tomazoni SS, Almeida MO, Bjordal JM, Stausholm MB, Machado CDSM, et al. (2020) Photobiomodulation therapy does not decrease pain and disability in people with non-specific low back pain: a systematic review. J Physiother 66: 155-165.
- Chan AS, Lee TL, Yeung MK, Hamblin MR (2019) Photobiomodulation improves the frontal cognitive function of older adults. Int J Geriatr Psychiatry 34: 369-377.
- Pruitt T, Wang X, Wu A, Kallioniemi E, Husain MM, et al. (2020) Transcranial Photobiomodulation (tPBM) With 1,064-nm Laser to Improve Cerebral Metabolism of the Human Brain In Vivo. Lasers Surg Med 52: 807-813.
- Sasso LL, Souza LG, Girasol CE, Marcolino AM, Guirro RRJ, et al. (2020) Photobiomodulation in Sciatic Nerve Crush Injuries in Rodents: A Systematic Review of the Literature and Perspectives for Clinical Treatment. J Lasers Med Sci 11: 332-344.
- Sobral AP, Sobral SS, Campos TM, Horliana AC, Fernandes KP, et al. (2021) Photobiomodulation and myofascial temporomandibular disorder: Systematic review and meta-analysis followed by cost-effectiveness analysis. J Clin Exp Dent 13: 724-732.
- Salehpour F, Majdi A, Pazhuhi M, Ghasemi F, Khademi M, et al. (2019) Transcranial Photobiomodulation Improves Cognitive Performance in Young Healthy Adults: A Systematic Review and Meta-Analysis. Photobiomodul Photomed Laser Surg 37: 635-643.
- Hadis MA, Zainal SA, Holder MJ, Carroll JD, Cooper PR, et al. (2016) The dark art of light measurement: accurate radiometry for low-level light therapy. Lasers Med Sci 31: 789-809.
- Mansano BS, Rocha VP, Antonio EL, Peron DF, Lima RN, et al. (2021) Enhancing the Therapeutic Potential of Mesenchymal Stem Cells with Light-Emitting Diode: Implications and Molecular Mechanisms. Oxidative Medicine and Cellular Longevity 2021: 6663539.
- Ezzati K, Laakso EL, Salari A, Hasannejad A, Fekrazad R, et al. (2020) The Beneficial Effects of High-Intensity Laser Therapy and Co-Interventions on Musculoskeletal Pain Management: A Systematic Review. J Lasers Med Sci 11: 81-90.
- Ezzati K, Laakso EL, Saberi A, Chabok SY, Nasiri E, et al. (2020) A comparative study of the dose-dependent effects of low level and high intensity photobiomodulation (laser) therapy on pain and electrophysiological parameters in patients with carpal tunnel syndrome. Eur J Phys Rehabil Med 56: 733-740.
- Taradaj J, Rajfur K, Shay B, Rajfur J, Ptaszkowski K, et al. (2018) Photobiomodulation using high- or low-level laser irradiations in patients with lumbar disc degenerative changes: disappointing outcomes and remarks. Clin Interv Aging 13: 1445-1455.
- Matys J, Swider K, Lesniak KG, Dominiak M, Romeo U (2019) Photobiomodulation by a 635nm Diode Laser on Peri-Implant Bone: Primary and Secondary Stability and Bone Density Analysis-A Randomized Clinical Trial. Biomed Res Int 2019:2785302.
- Zomorrodi R, Loheswaran G, Pushparaj A, Lim L (2019) Pulsed Near Infrared Transcranial and Intranasal Photobiomodulation Significantly Modulates Neural Oscillations: a pilot exploratory study. Scientific Reports
- Batista MR, Estrela LA, Alves VMN, Motta AR, Furlan RMMM (2021) Immediate effects of red (660 nm) and infrared (808 nm) photobiomodulation therapy on fatigue of the orbicularis oris muscle: a randomized clinical study. Codas 34: 20200363.
- Carvalho PD, Mazzer N, Reis FA, Belchior AC, Silva IS (2006) Analysis of the influence of low-power HeNe laser on the healing of skin wounds in diabetic and non-diabetic rats. Acta cirurgica brasileira 21: 177-183.
- Costa SA, Florezi GP, Artes GE, Costa JE, Gallo RT, et al. (2017) The analgesic effect of photobiomodulation therapy (830 nm) on the masticatory muscles: a randomized, double-blind study. Brazilian oral research 31: 107.
- Moskvin SV, Khadartsev AA (2020) Methods of effective low-level laser therapy in the treatment of patients with bronchial asthma (literature review). Biomedicine (Taipei) 10: 1-20.
- Liu CC, Hsu CS, He HC, Cheng YY, Chang ST (2021) Effects of intravascular laser phototherapy on delayed neurological sequelae after carbon monoxide intoxication as evaluated by brain perfusion imaging: A case report and review of the literature. World J Clin Cases 9: 3048-3055.
- Mikhaylov VA (2015) The use of Intravenous Laser Blood Irradiation (ILBI) at 630-640 nm to prevent vascular diseases and to increase life expectancy. Laser Ther 24: 15-26.
- Amjadi A, Mirmiranpor H, Khandani S, Sobhani SO, Shafaee Y (2019) Intravenous Laser Wavelength Irradiation Effect on Interleukins: IL-1α, IL-1β, IL6 in Diabetic Rats. Laser Ther 28: 267-273.
Citation: Wei TH, Hsieh CL (2022) Effect of Acupuncture on Oxidative Stress and Inflammation: From Mechanisms to Therapeutic Applications. J Altern Complement Integr Med 8: 230.
Copyright: © 2022 Tzu-Hsuan Wei, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.