
Effectiveness of Bypass and Sleeve Bariatric Surgical Methods in Weight Reduction
*Corresponding Author(s):
Cristianne Confessor Castilho LopesUniversity Of The Region Of Joinville, Joinville, Brazil
Tel:+55 49999812333,
Email:cristiannelopes3@gmail.com
Abstract
Obesity is a chronic disease described by the large amount of body fat that leads to an increase in Body Mass Index (BMI). It is subdivided into three levels, being grade I with a BMI between 30 and 34.9 kg/m2, grade II between 35 and 39.9 kg/m2 and grade III or morbid obesity with a BMI above 40 kg/m2. Aiming at reversing the morbid condition caused by the disease, the bariatric surgical technique presents itself as the most effective option to contain grade III obesity, as well as the associated co morbidities. The objective of surgical techniques is to improve the quality of life of the obese, reducing both physical and psychosocial problems. As endocrine disease is related to several co morbidities, such as high blood pressure, sleep apnea and even some types of cancer, it is necessary to carry out an investigation into the surgical technique to be applied as well as its effectiveness during and after the surgical procedure.
Keywords
Bariatric Surgery; Bypass; Sleeve; Weight Reduction
Introduction
According to the World Health Organization (WHO), obesity is a highly prevalent disease in Brazil and in the world, which is constantly advancing. It is characterized by the accumulation of adipose tissue in the body, causing an increase in the Body Mass Index (BMI) to greater than or equal to 30 kg/m2, being considered a risk factor for more than 200 other diseases [1].
The World Health Organization (WHO) characterizes obesity according to the Body Mass Index (BMI) above 30kg/m², qualifying grade I obesity when the BMI is between 30 and 34.9 kg/m², grade II obesity between 35 and 39.9kg/m² and, finally, grade III obesity when the BMI exceeds 40kg/m² [2].
Its consequences do not only concern issues related to health, but also quality of life, as the probability of falling ill is greater when well-being indicators are reduced, characterized by difficulties in social interactions, low self-esteem, loneliness, stress , depressive signs and also in performance of work activities [3].
Therapies aimed at lifestyle changes with and without the use of medications are useful strategies for reducing body weight, however, with little efficacy in morbidly obese individuals [4,5].
Second Costa et al., [6] bariatric surgery is the most effective for grade III obesity. The purpose of surgical treatment is to improve not only the quality, but also to increase the life expectancy of the obese, solving the physical, social and psychological problems that excess weight entails. Thus, it is necessary to carry out a detailed investigation of the patient’s clinical aspects, before indicating bariatric surgery. The importance of the participation of a multidisciplinary team is also highlighted, both preoperatively and in the post-operative period.
Due to the scenario of obesity in the population and the lack of success in attempts to reduce weight, medical science was motivated to develop studies to intervene in the improvement of the population's well-being, giving rise to bariatric surgery. Also known as gastroplasty and gastric bypass surgery, bariatric surgery has become an option for morbidly obese people who are unable to lose weight by traditional methods, or who suffer from chronic health problems related to this disease [7].
The requirements for performing the surgical method must cover individuals with a BMI greater than 40kg/m², with or without co morbidities, without efficacy in longitudinal clinical treatment for a period of at least two years and who have followed clinical protocols or who demonstrate a BMI greater than 35Kg/m² with co morbidities such as high cardiovascular risk, diabetes mellitus and/or difficult-to-control systemic arterial hypertension, sleep apnea, degenerative joint diseases.
Therefore, the aim of the present study was to evaluate the effectiveness of bariatric surgery techniques Roux-en-Y Gastric Bypass (BGYR) and Vertical Gastrectomy (GV) or sleeve in weight reduction through data analysis, through a form for patients who underwent bariatric surgery.
Theoretical Foundation
Obesity has been defined as a public health problem nowadays and has gained prominence in the global epidemiological scenario. Its prevalence has increased in recent years across the world, even in developing countries such as Brazil, where in ancient times adversities related to malnutrition predominated in the population [8].
The World Health Organization (WHO) calculates that, in 2005, there were around 1.6 billion adults with obesity and at least 400 million adults were classified as obese all over the world [9].
Currently, the bariatric surgical option is recognized as the instrument more efficient in the control and treatment of morbid obesity, providing a significant reduction in co morbidities associated with obesity, improving hypertension, diabetes and dyslipidemia.
Surgery improves body satisfaction and physical well-being. However, it is necessary to remember that the surgical treatment of obesity does not focus only on the surgical procedure [10]. According to the Brazilian Society of Bariatric and Metabolic Surgery (SBCBM), regardless of the technique used, to be eligible for surgery, the patient must have a Body Mass Index (BMI) greater than 40kg/m2, with or without co morbidities, and BMI between 35kg/m2 and 40kg/m2 in the presence of health aggravating factors [11].
Brazil is a country with a high rate of performance of bariatric surgeries. The therapeutic conduct before and after the bariatric surgical procedure, with the clinical evaluation of the psychologist, is pertinent. Since, the professional will help the patient in the transition of attitude necessary for a re-education of food and life habits, after surgery [12].
Regarding the methods adopted, the bypass technique forms a small gastric reservoir that does not include the distal part of the stomach, connecting it to the Roux-en-Y jejunal loop, thus bypassing the fundus of the stomach, duodenum and proximal small intestine. In turn, the sleeve or sleeve gastrectomy method presents itself as a biliopancreatic diversion without distal gastrectomy, preserving the pylorus, and in this technique there is no exclusion of the duodenum, preserving the functions of food and vitamin absorption [13].
Therefore, the bypass method is considered the gold standard by many bariatric specialists and has been the most used technique in Brazil. The surgical procedure can be divided according to the propositions of Fobi, Brolin or distal gastrojejunoileal (Scopinaro type) for stapling the stomach, that is, three practically similar ways to perform the surgery aiming to increase satiety and lead to weight loss, in addition to controlling co morbidities such as diabetes and hypertension, mainly [14].
The Sleeve technique, also known as shirt-sleeve gastrectomy, has been increasingly used and consists of transforming the gastric cavity into a tubular lumen aiming at decreasing body mass and being effective in the control of Systemic Arterial Hypertension (SAH) , cholesterol and triglycerides, and due to its low complication rates, it can become more applied than the bypass method in a short time [15].
Methodology
The study has a cross-sectional design, with a quantitative method and supported by a literature review. The instrument used was data collection through the development of questionnaires via Google forms, intended for patients who underwent surgical procedures.
The form addressed issues such as: gender, age, surgical technique adopted and marital status, how long the patient had undergone the procedure, how many kilograms were eliminated in the first week of surgery and, in total, if the patient tried to undergo any type of diet previously, as well as performing physical activity and having any type of associated co morbidity.
In addition, regarding the operative period, they were asked about the existence of complications or not during the surgery, whether the patient would indicate the method to someone and the level of satisfaction.
The survey was carried out between February and March 2020, after a supervised collection was carried out in the pilot study. The Informed Consent Form (FICF) was signed by the patients included in the investigation, ensuring the anonymity of information; the Term of Assent was filled out by the operated patients to certify that they were aware of the research carried out.
For its development, all ethical principles of research involving human beings were met, in accordance with the Resolution of the National Health Council No. 466 of December 12, 2012, having been approved by the ethics committee of the Centro Universitário Facvest under number 4,535 .870. Participants received the free and informed consent form in duplicate, one to the participant and the other to the researcher.
The researched group consisted of 68 patients.51 females and 17 males. All adults who have undergone the bariatric procedure.
Results
Through a survey conducted through the Google forms platform applied to 69 patients who underwent the surgical procedure in the city of Caçador-SC and Florianópolis-SC, and 68 patients agreed to voluntarily participate in the study (Figure 1).
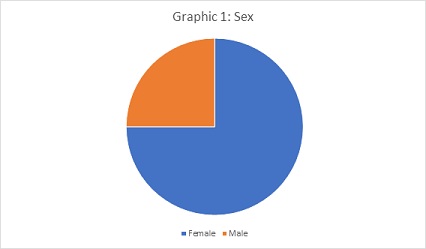 Figure 1: Sex.
Figure 1: Sex.
In the survey, it was identified that most patients underwent the Sleeve surgical technique (53%), and the remainder, 47%, by the Bypass method. In addition, 32.35% of respondents reported having undergone the surgery more than 20 months before the interview, 30.88% corresponded to the period between 12 and 24 months and the remainder up to 12 months (Figure 2).
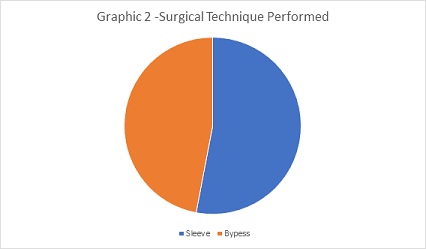 Figure 2: Surgical Technique Performed.
Figure 2: Surgical Technique Performed.
It was observed that 60.29% of respondents lost from 5kg to 10kg in the first week after the procedure, 27.9% up to 5kg and 11.7% corresponded to the range of 10kg to 15kg, in the same period of time. In turn, the total weight reduction in 80.8% of respondents corresponded to a loss of more than 30 kg, and the remainder, comprising 19.2% of patients, registered a decrease in overweight of less than 30 kg (Figure 3).
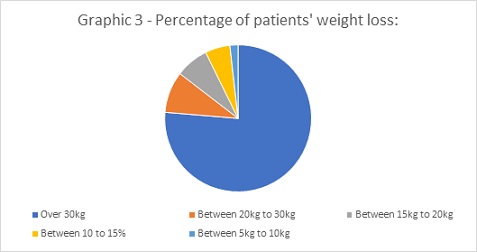 Figure 3: Percentage of patients' weight loss.
Figure 3: Percentage of patients' weight loss.
It is noteworthy that most patients (95.5%) tried to undergo some type of diet prior to the surgical procedure and, due to failure; the option of bariatric intervention was then indicated. More than half of respondents (57.35%) did not practice any type of physical activity due to unidentified factors, and this circumstance is relevant in terms of encouraging physical re-education in overweight patients.
Furthermore, the survey addressed the existence of co morbidities, with 31 of the respondents (45.5%) having no disease associated with overweight, 10 (14.7%) had Systemic Arterial Hypertension and Orthopedic Problems, 4 (5, 88%) Sleep Apnea, 1 (1.47%) Diabetes Mellitus and 11 (16.17%) patients report having other types of co morbidities.
The relationship between surgical complications, such as fistulas and infections, was also investigated, and it was reported that only 1 patient (1.47%) had an infection.
Regarding the comparison between the adopted technique and total weight loss, it was evident that the result was better compared to Gastric Bypass. A reduction in body mass above 30 kilograms occurred in 30 patients undergoing this technique, corresponding to 44.11% of respondents, while only 25 (36.76%) of respondents who underwent the Sleeve technique had the same amount of reduction in weight. body mass. It becomes clear that even the most prevalent technique being the sleeve gastrectomy, the greatest weight reduction was with Bypass.
Finally, the data collected showed that all patients who underwent bariatric surgery, being subjected to the prevalent sleeve technique)and also by the Bypass method, they would indicate the procedure to other people. The recommendation factors are directly linked to postoperative success and the level of surgical satisfaction, and the classification of this level on a scale from 9 to 10 was equivalent to 88.23% of the interviewed patients and 11.7% between 7 to 8 of satisfaction.
Discussion
The incidence of obesity is growing rapidly all over the world, and it is currently a major public health problem. This disease can cause other illnesses such as diabetes, systemic arterial hypertension, dyslipidemia and obstructive sleep apnea among other diseases [16].
In search of effective treatments for obesity, different surgical interventions have been developed, however, the methods Roux-en-Y, Gastric Bypass (BGYR) and sleeve Gastrectomy (GV) or Sleeve are the most accomplished [17,18].
When we compare the safety of the two methods, considering the mortality rate, the improvement in quality of life and the reduction of co morbidities, the two methods proved to be equally effective [19-21]. Chaar; Lundberg; Stoltzfus [22] analyzed 141,646 procedures, through the records of the Accreditation and Quality Improvement Program in Metabolic and Bariatric Surgery, with 98,292 submitted to SG and 43,354 to RYGB. They analyzed the first thirty days after the procedures and found that the mortality rate was 0.1% for SG and 0.2% for RYGB, reoperation after RYGB was significantly higher compared to SG and readmission to a hospital/unit of intensive care was 2.8% for RYGB and 1.2% for SG. According to this study, SG appears to be safer in the first thirty days after the surgical procedure.
However, after five years or more of follow-up, patients undergoing RYGB surgery recorded the greatest reduction in excess weight [23-26].
Articles published By Ignat et al., Maffazioli et al., Oliveira et al., Peterli et al., Zhang et al., [19,21,27-29] found no significant differences in body weight reduction after the two surgical procedures.
Huang et al., [30] investigated the medical records of 68 patients, 44 undergoing RYGB and 24 undergoing GV. And found that after a year of follow-up there was no significant difference in body weight reduction, however, RYGB seemed more effective in treating diabetes. Both techniques were shown to be equally effective in the treatment of other co morbidities such as hypertension, hyperlipidemia and fatty liver hepatitis. The occurrence of reoperation was higher in patients undergoing RYGB.
Final Considerations
Bariatric surgery aims to improve not only the quality, but also increase the life expectancy of the obese, solving the physical, social and psychological problems that excess weight causes.
In the study performed, final weight loss was similar in gastric bypass and sleeve gastrectomy, as well as surgical and therapeutic success. These data were consistent with part of the bibliography consulted.
Possibly, the different ways of ascertaining the reduction in body weight used by the consulted studies favored the antagonistic results.
Even so, studies that analyze the safety and effectiveness of surgical procedures are important, as they will help physicians and patients to choose the best method.
In addition, orienting the post-surgical patient about the change in post-bariatric lifestyle habits is always a guideline for the success of the treatment.
References
- Yeh T-L, Chen H-H, Chiu H-H, Chiu Y-H, Hwang L-C, et al. (2019) Morbidity associated with overweight and obesity in health personnel: a 10-year retrospective of hospital-based cohort study in Taiwan. Diabetes, metabolic syndrome and obesity: targets and therapy 12: 267-274.
- Fandiño J (2004) Bariatric surgery: clinical-surgical and psychiatric aspects. Revista de Psychiatry of Rio Grande 26: 47-51.
- Castanha CR (2018) Assessment of quality of life, weight loss and comorbidities in patients undergoing bariatric surgery. Journal of the Brazilian College of Surgeons 45: 3.
- As MD, Hayashi ÂY (2020) status of weight loss after gastroplasty in obese patients. Brazilian Journal of Surgery and Clinical Research – BJSCR 1: 52-60.
- Ejtahed H-S, Angoorani P, Hasani-Ranjbar S, Siadat S-D, Ghasemi N, et al. (2018) Adaptation of human gut microbiota to bariatric surgeries in morbidly obese patients: A systematic review. Microbial pathogenesis 116: 13-21.
- Costa ACC (2009) Obesity in bariatric surgery candidates. Paulista Nursing Act 22: 55-59.
- Marcellin LF, Patrício ZM (2011) The complexity of obesity and the process of living after bariatric surgery: a matter of collective health. Science & Public Health 16: 4767-4776.
- Enes CC, Slater B (2010) Obesity in adolescence and its main determining factors. Brazilian Journal of Epidemiology 13: 163-171.
- Tavares TB, Nunes SM, Santos MDO (2010) Obesity and quality of life: literature review. Rev Med Minas Gerais 359-366.
- Bordalo LA, Teixeira TFS, Bressan J, Mourão DM (2011) Bariatric surgery: how and why to supplement. Rev Assoc Med Bras 57: 113-120.
- Zeve JLDEM, Novais PO, Júnior NDO (2012) Techniques in bariatric surgery: a literature review. Science & Health 5: 132.
- Flores CA (2014) Psychological assessment for bariatric surgery: current practices. Brazilian Archives of Digestive Surgery (São Paulo) 27: 59-62.
- Nora C (2016) Sleeve gastrectomy and gastric bypass in the treatment of metabolic syndrome. Portuguese Journal of Endocrinology, Diabetes and Metabolism 11: 23-29.
- Ramos AC, Silva ACS, Ramos MG, Canseco EGC, Galvão-Neto MP, et al. (2014) Simplified gastric bypass: 13 years of experience and 12,000 patients operated. Arq Bras Cir Dig 27: 2-8.
- Lopez-Nava G, Galvão MP, Bautista-Castaño I, Fernandez-Corbelle JP, Trell T, et al. (2017) Endoscopic Sleeve Gastroplasty For Obesity Treatment: Two Years Of Experience. Arq Bras Cir Dig 30:18-20.
- Zilberstein B. Santo MA, Carvalho MH (2019) Critical Analysis Of Surgical Treatment Techniques Of Morbid Obesity. Brazilian Archives of Digestive Surgery (São Paulo) 32: 03.
- Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, et al. (2018) IFSO Worldwide Survey 2016: Primary, Endoluminal, and Revisional Procedures. Obesity Surgery 28: 3783-3794.
- Kirkil C, Aygen E, Korkmaz MF, Bozan MB (2018) Quality Of Life After Laparoscopic Sleeve Gastrectomy Using Baros System. Arq Bras Cir Dig 31: 1385.
- Ignat M, Vix M, Imad I, Urso AD, Perretta S, et al. (2017) Randomized trial of Roux-en-Y gastric bypass versus sleeve gastrectomy in achieving excess weight loss. British Journal of Surgery 104: 248-256.
- Spaniolas K, Goldberg I, Yang J, Zhu C, Docimo S, et al. (2019) Hospital utilization 4 years after bariatric surgery: sleeve gastrectomy versus Roux-en-Y gastric bypass. Surgery for Obesity and Related Diseases 15: 1465-1472.
- Zhang Y, Zhao H, Cao Z, Sun X, Zhang C, et al. (2014) A Randomized Clinical Trial of Laparoscopic Roux-en-Y Gastric Bypass and Sleeve Gastrectomy for the Treatment of Morbid Obesity in China: a 5-Year Outcome. Obesity Surgery 24: 1617-1624.
- Chaar MEL, Lundberg P, Stoltzfus J (2018) Thirty-day outcomes of sleeve gastrectomy versus Roux-en-Y gastric bypass: first report based on Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. Surgery for Obesity and Related Diseases 14: 545-551.
- Barros FDE; Negrão MG, Negrão GG (2019) Weight Loss Comparison After Sleeve And Roux-En-Y Gastric Bypass: Systematic Review. Arq Bras Cir Dig 32: 1474.
- Golzarand M, Toolabi K, Farid R (2017) The bariatric surgery and weight losing: a meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surgical Endoscopy 31: 4331-
- Lee JH, Nguyen Q-N, Le QA (2016) Comparative effectiveness of 3 bariatric surgery procedures: Roux-en-Y gastric bypass, laparoscopic adjustable gastric band, and sleeve gastrectomy. Surgery for Obesity and Related Diseases 12: 997-1002.
- Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, et al. (2017) Bariatric Surgery versus Intensive Medical Therapy for Diabetes - 5-Year Outcomes. New England Journal of Medicine 376: 641-651.
- Maffazioli GD, Stanford FC, Reyes KJC, Stanley TL, Singhal V, et al. (2016) Comparing Outcomes of Two Types of Bariatric Surgery in an Adolescent Obese Population: Roux-en-Y Gastric Bypass vs. Sleeve Gastrectomy. Front Pediatr 4: 78.
- Oliveira PSCDE (2021) A Comparative Literature Review Between The Efficiency Of Sleeve Or Gastric Bypass In Y-De-Roux. Integrated Scientific Magazine 5: 1-19.
- Peterli R, H elmiö M, Ovaska J (2018) Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss in Patients With Morbid Obesity. JAMA 319: 241-254.
- Huang C-K, Garg A, Kuao H-C, Chang P-C, Hsin M-C (2015) Bariatric surgery in old age: a comparative study of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy in an Asia center of excellence. Journal of Biomedical Research 29: 118-124.
Citation: Lopes CCC, Lopes EB, Wietzycoski CR, Zanatta LR, Santos D (2021) Effectiveness of Bypass and Sleeve Bariatric Surgical Methods in Weight Reduction. J Altern Complement Integr Med 7: 194.
Copyright: © 2021 Cristianne Confessor Castilho Lopes, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

