
Journal of Neonatology & Clinical Pediatrics Category: Clinical
Type: Research Article
Effects of Early Intervention on the Language of Mexican and Galician Preterm Infants
*Corresponding Author(s):
Donna Jackson-MaldonadoFacultad De Lenguas Y Letras, Casa Fray Junipero Serra Queretaro-8, Universidad Autonoma De Queretaro, Santiago De Queretaro, Queretaro, Mexico
Tel:+52 442 2180264,
Email:djacksonqro@gmail.com
Received Date: Aug 13, 2016
Accepted Date: Mar 15, 2017
Published Date: Mar 29, 2017
Abstract
The study of preterm infants has increased considerably over the last decade due to the fact that more babies survive because of advances in the medical field. There has been interest in the development of this population as children born prematurely are at risk for cognitive, motor and linguistic development. Little research is available about the impact of motor or language intervention on late preterm infants. The goals of this study are to compare vocabulary comprehension and production in 3 groups of 10 month-old preterm infants in Spain and Mexico who have received different types of early intervention to full term infants. Results show strong effects of early intervention mostly for vocabulary comprehension principally for the group who received motor and language intervention. It is suggested that early language intervention has positive effects on language outcomes in preterm infants.
Keywords
Galician; Intervention; Preterm; Spanish; Vocabulary
INTRODUCTION
According to the World Health Association, 1 out of 10 babies worldwide are born prematurely or before the 37th week of gestation. There is a higher percent of Preterm Births (PR) in less developed countries [1,2]. The study of PR infants has increased considerably over the last decade due to the fact that more babies survive because of advances in the medical field. In this study we address PR populations that share cultural and language roots in Mexico and Spain, for which there is scant research available. These two populations are comparable at early stages of development in which first words are usually quite similar in both linguistic variants and languages that are closely related, such as Galician and Catalan.
In Mexico, there is a large discrepancy concerning the rate of premature births. The percentage of premature births reported ranges from 4.1 to 19.7% to depending on the state and the level of poverty being considered [3,4]. In Spain, it has been reported that approximately 7.4% of births are PR [2,5].
Despite medical advances, with differences in each country, there is still a large percent of PR infants who are at risk for brain damage or developmental disorders including difficulties with cognitive, motor and linguistic development [6-11]. In fact, it has been noted that PR infants are 50% more likely than Full Term (FT) infants to be enrolled in special education programs later in life [12,13].
In Mexico, there is a large discrepancy concerning the rate of premature births. The percentage of premature births reported ranges from 4.1 to 19.7% to depending on the state and the level of poverty being considered [3,4]. In Spain, it has been reported that approximately 7.4% of births are PR [2,5].
Despite medical advances, with differences in each country, there is still a large percent of PR infants who are at risk for brain damage or developmental disorders including difficulties with cognitive, motor and linguistic development [6-11]. In fact, it has been noted that PR infants are 50% more likely than Full Term (FT) infants to be enrolled in special education programs later in life [12,13].
FACTORS THAT AFFECT DEVELOPMENT
The developmental delays reported for PR infants may vary, as they are not a homogeneous group. Their developmental risks may vary based on multiple medical and environmental factors. Typically, the extent of cognitive, motor and language delays is inversely related to Gestational Age (GA) Birth Weight (BW) [14-16], and directly related with intrauterine growth restriction [6]. Infants may be classified by GA as late preterm if they are born between 34 and 36 weeks, moderately preterm between 32 and 33 weeks, very preterm between 28 and 31 weeks and extremely preterm, below 28 weeks of gestation. Though highly correlated with GA, birth weight has also been shown to be a contributing factor to infants’ developmental risk levels. There are also several levels of birth weight. The cut-off point is between 1.5 and 2.5 kilos. Approximately 10% of low birth weight infants exhibit cerebral palsy, and about 50% have cognitive and behavioral deficits [17].
Additional medical risk factors associated with PR include bronchopulmonary dysplasia, germinal matrix intraventricular hemorrhage, posthemorrhagic hydrocephalus, and Periventricular Leukomalacia (PVL). Environmental factors, such as socio-economic status, maternal affect and family context have also been found to affect PR infants’ risk [18-20]. Of these factors, of particular interest for this study is the effect of PVL.
PVL is a frequent type of lesion found in the brains of PR infants [21], consisting of white matter lesions surrounding the ventricles. This condition is identified by neuro-resonance imaging (fMRI) or by cranial ultrasound at birth. PLV can be classified by different degrees of severity. However, many studies do not clearly identify which type of PVL is present in the populations that are observed as not all PR infants are submitted to neuroimaging, the only currently available means for detecting PVL. This diagnostic distinction is important, as there are large differences in infants’ outcomes depending on the degree of lesion. For example, long-term cognitive and linguistic developmental effects have been associated with non-cystic PVL with diffuse lesions [17,22,23], whereas Cerebral Palsy is mostly correlated with focal necrotic lesions of PVL deep in the cerebral white matter [17]. Diffuse or Non-Cystic PVL (NC-PVL) may have symptoms that are not easily detected whereas the sequels of severe or cystic PVL are highly related to Cerebral Palsy.
Additional medical risk factors associated with PR include bronchopulmonary dysplasia, germinal matrix intraventricular hemorrhage, posthemorrhagic hydrocephalus, and Periventricular Leukomalacia (PVL). Environmental factors, such as socio-economic status, maternal affect and family context have also been found to affect PR infants’ risk [18-20]. Of these factors, of particular interest for this study is the effect of PVL.
PVL is a frequent type of lesion found in the brains of PR infants [21], consisting of white matter lesions surrounding the ventricles. This condition is identified by neuro-resonance imaging (fMRI) or by cranial ultrasound at birth. PLV can be classified by different degrees of severity. However, many studies do not clearly identify which type of PVL is present in the populations that are observed as not all PR infants are submitted to neuroimaging, the only currently available means for detecting PVL. This diagnostic distinction is important, as there are large differences in infants’ outcomes depending on the degree of lesion. For example, long-term cognitive and linguistic developmental effects have been associated with non-cystic PVL with diffuse lesions [17,22,23], whereas Cerebral Palsy is mostly correlated with focal necrotic lesions of PVL deep in the cerebral white matter [17]. Diffuse or Non-Cystic PVL (NC-PVL) may have symptoms that are not easily detected whereas the sequels of severe or cystic PVL are highly related to Cerebral Palsy.
EFFECT OF PREMATURITY ON LANGUAGE DEVELOPMENT
Empirical consensus on the effect of prematurity on language development has not yet been reached. In some studies, the performance of PR infants on a variety of communicative scales has been found to fall below that of Full Term (FT) children [24-28]. Other research findings do not suggest such definitive results [18, 29-32] or suggest that effects are observed later in life [30,33,34]. What is known, however, is that the effect of prematurity on language development is also related to several socio-demographic factors such as, maternal age and education, ethnicity and type of household [20,24,35]. Furthermore, infants from low Socio-Economic Status (SES) families are less likely to receive intervention services than children from higher SES groups, which could be a confounding factor [36].
Thus, there are no definite conclusions, and further studies are merited that differentiate risk characteristics. As most risk has been found in extreme populations of PR births, such as very and extremely premature infants, other groups need to be studied, such as moderate and late PR [7,11,18,37,38]. Another factor that affects development is the rate and type of early intervention the infant receives and this also needs to be studied in more depth. This study addresses early intervention in late preterm infants.
Thus, there are no definite conclusions, and further studies are merited that differentiate risk characteristics. As most risk has been found in extreme populations of PR births, such as very and extremely premature infants, other groups need to be studied, such as moderate and late PR [7,11,18,37,38]. Another factor that affects development is the rate and type of early intervention the infant receives and this also needs to be studied in more depth. This study addresses early intervention in late preterm infants.
EARLY INTERVENTION
Hospital care, intervention and doctor follow-up are all a vital part of the survival and development of PR infants as has been shown in the U.S. and most European countries [37-42]. The majority of studies of early intervention with PR infants have addressed health problems and motor development. Cognitive and language interventions after infants are discharged from Neonatal Intensive Care Units (NICU) have been less well documented. When early intervention is addressed in the existing literature, it has been strongly suggested that PR infants benefit positively, that is, developmental gaps are reduced. Most precisely it has been shown that intervention methods with strong parental interaction and that teach responsiveness have outcomes in which children who receive early intervention are statistically superior to children who do not in most of the areas that are analyzed [37,43].
There is inconsistent evidence to show the effects of early intervention on birth weight, gestational age, risk or type of intervention as many times these factors are not controlled for or are not reported in participant descriptions [12,16,35,37,38,43-50]. Another important finding of these studies is that strong positive effects of the intervention were observed later in childhood that may not have been apparent at early ages [33,44].
The cited research projects are based on social and cognitive interventions that are not the goal of our study. Here we are interested in the effects of a dynamic motor as well as language intervention. Static and dynamic methods of physical therapy differ on premises of the infant’s direct participation. The Bobath or Neurodevelopmental Therapy (Bobath or NDT) is a frequently used dynamic method, mostly in children with Cerebral Palsy. Several studies have shown that children advanced significantly in the Gross Motor Function Measure, motor reflexes as well as in self care [51-54]. Only one study to date, to our knowledge, has studied PR infants receiving Bobath using clinical trials [55]. Significant differences were found between the preterm treatment group and both control groups in posture, behavior and solicited items.
Another, less well known dynamic method is the Katona system [56-62]. It differs from the Bobath in the type of manipulation and specific technique, but the goal of having the infant respond actively to the movements is similar. Both interventions begin immediately after birth and target muscle tone control and posture as well as active participation of the caregivers [53,63,64]. Specific aspects of the technique and type of manipulation differ. The Katona method has a recent efficacy reports with PR infants [57]. Here two groups of preterm infants under 2 months of age were seen: with and without neurohabilitation intervention. Results showed that the group with intervention had a higher percent of children with normal neurodevelopmental outcomes than the non-treated group (90%). Two other studies have shown changes in neurological and motor functions for PR infants 6 to 8 months after intervention [65,66].
Based on extensive previous research cited above it has consistently been shown that PR infants may have cognitive and linguistic delays. The effect of intervention has been explored, though to a lesser degree in PR infants and only a handful of studies exist for Spanish-speaking children. Much less, is there evidence for the efficacy of dynamic motor treatment on the infant’s language development.
There is inconsistent evidence to show the effects of early intervention on birth weight, gestational age, risk or type of intervention as many times these factors are not controlled for or are not reported in participant descriptions [12,16,35,37,38,43-50]. Another important finding of these studies is that strong positive effects of the intervention were observed later in childhood that may not have been apparent at early ages [33,44].
The cited research projects are based on social and cognitive interventions that are not the goal of our study. Here we are interested in the effects of a dynamic motor as well as language intervention. Static and dynamic methods of physical therapy differ on premises of the infant’s direct participation. The Bobath or Neurodevelopmental Therapy (Bobath or NDT) is a frequently used dynamic method, mostly in children with Cerebral Palsy. Several studies have shown that children advanced significantly in the Gross Motor Function Measure, motor reflexes as well as in self care [51-54]. Only one study to date, to our knowledge, has studied PR infants receiving Bobath using clinical trials [55]. Significant differences were found between the preterm treatment group and both control groups in posture, behavior and solicited items.
Another, less well known dynamic method is the Katona system [56-62]. It differs from the Bobath in the type of manipulation and specific technique, but the goal of having the infant respond actively to the movements is similar. Both interventions begin immediately after birth and target muscle tone control and posture as well as active participation of the caregivers [53,63,64]. Specific aspects of the technique and type of manipulation differ. The Katona method has a recent efficacy reports with PR infants [57]. Here two groups of preterm infants under 2 months of age were seen: with and without neurohabilitation intervention. Results showed that the group with intervention had a higher percent of children with normal neurodevelopmental outcomes than the non-treated group (90%). Two other studies have shown changes in neurological and motor functions for PR infants 6 to 8 months after intervention [65,66].
Based on extensive previous research cited above it has consistently been shown that PR infants may have cognitive and linguistic delays. The effect of intervention has been explored, though to a lesser degree in PR infants and only a handful of studies exist for Spanish-speaking children. Much less, is there evidence for the efficacy of dynamic motor treatment on the infant’s language development.
PURPOSE OF THE STUDY
In this study, we concentrated our attention on PR infants in two quite similar cultural and linguistic contexts from a joint project between Mexico and Galicia, Spain. We considered four factors: Birth Weight (BW), Gestational Age (GA), medical complications (non-cystic Periventricular Leucomalacia, in particular) and early motor and communication interventions. The following research questions were addressed: (1) Does early motor intervention have an effect on PR’s vocabulary development? (2) Does early communication intervention with PR infants have a stronger effect on language competence than does motor intervention? We respond to the following hypothesis: PR infants who receive motor and/or language intervention will have higher vocabulary levels than their peers who do not receive any intervention. In order to address these questions, we compared 10 to 14 month old PR infants with and without NC-PVL in terms of their vocabulary comprehension and production by means of a well-known and experimented maternal report. We also compared PR infants who received post-NICU early motor and/or communication interventions to infants who did not receive intervention. We present a referential, full term group, in order to contrast with a typical population, but it is not specific goal of the paper to determine differences with this group.
All participants in this study were part of larger projects in which multiple aspects of development were assessed with different instruments. Data using the other instruments have been published elsewhere [18,29,67,68,69]. Here we will only concentrate on results from the parental report of communicative abilities.
All participants in this study were part of larger projects in which multiple aspects of development were assessed with different instruments. Data using the other instruments have been published elsewhere [18,29,67,68,69]. Here we will only concentrate on results from the parental report of communicative abilities.
METHOD
Participants
This study is based on three cohorts of PR infants and one group of Full Term (FT) infants in two countries: one PR and one FT group in Galicia, Spain [18,29,70] and two PR groups in Mexico [67,69,70]. All infants were participating in larger studies at the time these data were collected. Although the Galician infants were from both monolingual and bilingual (Galician-Spanish) families, we considered the populations comparable for three reasons: First, the Galician language is highly related to Spanish. Galician and Spanish are both Romance languages and are mutually intelligible languages in many cases. Second, early words used by children are frequently similar in both languages. Particularly, the first words comprehended by children at age 14 months are mostly the same in pronunciation and structure. For instance, a contrast between the language assessment instruments used in the study (based on an analysis of the forms by the first authors of this study) showed that 90% of the words were equal or only differed on a few sounds. Both instruments were versions of the MacArthur Bates Communicative Development Instrument Word & Gestures [71]. Many first words are indistinguishable between languages and, thus, bilingual status is hard or impossible to establish at this early age. For instance, of the first words comprehended [72] almost 100% are identical (mama, papa, galleta, pan, botella, comer, guaguá) or have similar pronunciations (auga-agua, leite-leche, baixar-bailar) that could easily be variants of the same word as children at this stage follow multiple phonological processes. At later stages, when morphology is more complex, differences between the two languages are more apparent and, thus, this type of study would no longer be relevant or reliable. Thirdly, Galician-Spanish and Mexican populations share similar cultural contexts, especially in early child rearing and family interaction both of which are important factors in this study.
The three cohorts of PR infants were between 10 and 14 months corrected age. The Galician cohort was included in order to contrast infants who had not received intervention as these were not readily available in Mexico. Most were followed from birth, but data at later dates is not available because children no longer participated in the project. Risk factors were controlled for and samples were similar at birth excluding the variables that were part of the study, like NC-PVL. Social and medical factors were similar (see below). The FT sample, Group 1 (GP1), was a referential group of Galician healthy, full term infants [18,68,70]. It consisted of 49 infants who were 10 months of age.
Group 2 (GP2) consisted of 32 Galician PR infants without NC-PVL or other relevant medical complication. These infants did not receive any post NICU intervention as it was not part of the hospital protocol. All infants were 10 months of age at the time of data collection.
Groups 3 and 4 were Mexican PR infants who were in different types of intervention. Group 3 (GP2) included 15 PR Mexican infants between the ages of 10 and 14 months who were diagnosed with NC-PVL and received Katona therapy (see above) in the first weeks after birth. They were part of the protocol of a research project at the XXX in which only Katona therapy was given. Group 4 (GP4) consisted of 30 PR Mexican infants with NC-PVL, between the ages of 10 and 14 months, who received Katona therapy and were also in an early post NICU intervention language program that was developed explicitly for the XXX center. Participants from Group 3 and 4 were randomly selected to participate in either type of intervention as they were part of different stages of a larger research project.
Mother’s educational level across for the Galician sample was mostly of High School and above (GP4 or FT = 61%, GP2, PR with no NC-PVL = 84%) for both PR and FT infants [18,68] with a slightly higher educational level in the PR group. The Mexican samples were also predominantly composed of more than High School educated mothers (GP2 = 77%, GP3 = 76%) Thus, all samples consisted mostly of parents who had educational levels of High School or above educational.
Table 1 presents descriptive information for each group of infants. It should be noted that not all descriptive statistics were run for corrected age for GPs 1 (full term) and 2 (PR with no intervention), as all children were seen at 10 months of age (plus or minus 15 days). A t test of independent measures yielded no significant differences (p = .41) between the other two PR (motor and motor and language intervention) groups for corrected age (GP3, M = 11.4, SD = 1.6; GP4, M = 10.7, SD = 1.31). All groups were compared for gender, Birth Weight (BW) and Gestational Age (GA). The groups were equivalent in gender proportion (p = .508). Birth weight (BW) in kilos, as would be expected, was significantly lower in all the PR groups than in the FT group, F(3,120) = 133, p < .001, ω2 = 0.762. No significant differences were found within the three PR groups for BW, F(2,72) = 1.2, p = .285 or for GA F(2,72) = 1.4, p = .23 (Table 1).
The three cohorts of PR infants were between 10 and 14 months corrected age. The Galician cohort was included in order to contrast infants who had not received intervention as these were not readily available in Mexico. Most were followed from birth, but data at later dates is not available because children no longer participated in the project. Risk factors were controlled for and samples were similar at birth excluding the variables that were part of the study, like NC-PVL. Social and medical factors were similar (see below). The FT sample, Group 1 (GP1), was a referential group of Galician healthy, full term infants [18,68,70]. It consisted of 49 infants who were 10 months of age.
Group 2 (GP2) consisted of 32 Galician PR infants without NC-PVL or other relevant medical complication. These infants did not receive any post NICU intervention as it was not part of the hospital protocol. All infants were 10 months of age at the time of data collection.
Groups 3 and 4 were Mexican PR infants who were in different types of intervention. Group 3 (GP2) included 15 PR Mexican infants between the ages of 10 and 14 months who were diagnosed with NC-PVL and received Katona therapy (see above) in the first weeks after birth. They were part of the protocol of a research project at the XXX in which only Katona therapy was given. Group 4 (GP4) consisted of 30 PR Mexican infants with NC-PVL, between the ages of 10 and 14 months, who received Katona therapy and were also in an early post NICU intervention language program that was developed explicitly for the XXX center. Participants from Group 3 and 4 were randomly selected to participate in either type of intervention as they were part of different stages of a larger research project.
Mother’s educational level across for the Galician sample was mostly of High School and above (GP4 or FT = 61%, GP2, PR with no NC-PVL = 84%) for both PR and FT infants [18,68] with a slightly higher educational level in the PR group. The Mexican samples were also predominantly composed of more than High School educated mothers (GP2 = 77%, GP3 = 76%) Thus, all samples consisted mostly of parents who had educational levels of High School or above educational.
Table 1 presents descriptive information for each group of infants. It should be noted that not all descriptive statistics were run for corrected age for GPs 1 (full term) and 2 (PR with no intervention), as all children were seen at 10 months of age (plus or minus 15 days). A t test of independent measures yielded no significant differences (p = .41) between the other two PR (motor and motor and language intervention) groups for corrected age (GP3, M = 11.4, SD = 1.6; GP4, M = 10.7, SD = 1.31). All groups were compared for gender, Birth Weight (BW) and Gestational Age (GA). The groups were equivalent in gender proportion (p = .508). Birth weight (BW) in kilos, as would be expected, was significantly lower in all the PR groups than in the FT group, F(3,120) = 133, p < .001, ω2 = 0.762. No significant differences were found within the three PR groups for BW, F(2,72) = 1.2, p = .285 or for GA F(2,72) = 1.4, p = .23 (Table 1).
| N | Corrected Age | Gestational Age | Weight at Birth | %prod (SD) | % comp (SD) | |
| GP1 | 32 | 10 (0) | 30.8 (2.89) | 1.44 (444) | 1.29 (1.96) | 20.83 (17.97) |
| GP2 | 15 | 10.7 (1.31) | 32.9 (2.22) | 1.64 (696) | 1.36 (1.54) | 33.86 (13.59) |
| GP3 | 30 | 11.4 (1.60) | 30.9 (2.86) | 1.65 (670) | 2.75 (3.10) | 37.88 (19.23) |
| GP4 | 49 | 10 (0) | 39.8 ** | 3.38 (415) ** | 1.66 (5.72) | 18.71(15.30) * |
Table 1: Descriptive information of full sample: age, birth weight, mean percent vocabulary words produced and comprehended (Standard Deviation).
Note: GP1 = Premature without NC-PVL or intervention, GP-2 = Premature with NC-PVL and motor intervention, GP3 = Premature with NC-PVL and motor and language intervention, GP4 = full term.
% prod (SD) = Percent produced of total words on CDI (Standard Deviation), % comp (SD) = Percent comprehended of total words on CDI (Standard Deviation).
% prod (SD) = Percent produced of total words on CDI (Standard Deviation), % comp (SD) = Percent comprehended of total words on CDI (Standard Deviation).
Measures
All infants were evaluated using several different language and cognitive measures; although in this study we will concentrate only on data from parental report instruments. Many clinicians and related professionals may consider that parent report could be biased and that parents are not good agents in determining their child’s communicative abilities. There is strong evidence to the contrary. An extensive literature beginning with the seminal work by Bates and colleagues [73] has documented the validity of properly obtained parent report, in fact in many situations superior to that of direct child assessment or observation [74]. There are currently over 70 languages that have developed MacArthur-Bates Communicative Development Inventories (MBCDI) [71,75] all with high validity and reliability [76,77]. Further, the MBCDIs are applied in the assessment of children with different language and cognitive disorders. Thus, the MBCDI versions for Spanish and Galician were considered to be optimal instruments for measuring vocabulary comprehension and production in this study.
Another issue that was considered in the instrument selection, to best appreciate language development, was in line with the literature that has consistently has shown variability in vocabulary development within age groups. There is also robust data showing that in language development variability across all age ranges is the norm rather than the exception [78]. Nelson [79], based on an ample sample of toddlers, proposed that individual differences and variability manifested by different learning styles (including number and types of words) should be considered when analyzing language development, but all within certain milestones. Contrary to medical tests, language tests should illustrate these differences within groups with evidence based cut-off points to determine risk. As shown in Fenson et al., [78] the MBCDIs do reflect this expected variability.
The Galician and Spanish versions of a parental report, the MBCDI Palabras e Xestos or Primeras Palabra y Gestos (First Words and Gestures) [80-82] were used in this study. Parental report measures, such as these, have been shown to be adequate measures to determine communicative development at very early stages of development and with preterm infants [83]. Parents of all children filled out the forms for their specific language (Galician or Spanish) at home, in the hospital or during visits to the university clinics. A brief explanation was given to parents that included the difference between comprehension and production, word variations because of pronunciation, contexts in which words are used, etc. In this study, we will only report on the vocabulary comprehension and production sections of these measures. The Galician form consists of 384 words whereas the Spanish form has 428 words. In order to equate scores, rather than report raw scores or percentiles, we calculated percent of words identified by parents.
Another issue that was considered in the instrument selection, to best appreciate language development, was in line with the literature that has consistently has shown variability in vocabulary development within age groups. There is also robust data showing that in language development variability across all age ranges is the norm rather than the exception [78]. Nelson [79], based on an ample sample of toddlers, proposed that individual differences and variability manifested by different learning styles (including number and types of words) should be considered when analyzing language development, but all within certain milestones. Contrary to medical tests, language tests should illustrate these differences within groups with evidence based cut-off points to determine risk. As shown in Fenson et al., [78] the MBCDIs do reflect this expected variability.
The Galician and Spanish versions of a parental report, the MBCDI Palabras e Xestos or Primeras Palabra y Gestos (First Words and Gestures) [80-82] were used in this study. Parental report measures, such as these, have been shown to be adequate measures to determine communicative development at very early stages of development and with preterm infants [83]. Parents of all children filled out the forms for their specific language (Galician or Spanish) at home, in the hospital or during visits to the university clinics. A brief explanation was given to parents that included the difference between comprehension and production, word variations because of pronunciation, contexts in which words are used, etc. In this study, we will only report on the vocabulary comprehension and production sections of these measures. The Galician form consists of 384 words whereas the Spanish form has 428 words. In order to equate scores, rather than report raw scores or percentiles, we calculated percent of words identified by parents.
PROCEDURES
Informed consent was obtained from all of the infants’ parents at the beginning of the studies. Ethical regulations for all three of the university sites involved were appropriately followed (Universidad XX, Universidad XXX and Universidad XXXX).
Infants in the Galician study were part of a larger longitudinal study [18,68,81]. Families were initially contacted through the hospital setting and asked to participate. Infants were not in early intervention programs after hospital discharge. At 15 days of age (after birth) the infants were evaluated with the Neonatal Behavioral Assessment Scale (NBAS) [84,85]. Preterm infants scored higher in motor and range of state cluster, while FT infants had higher scores in regulation of state clusters. At that time, the mothers of the infants participated in a long interview in which family environment and general health information was obtained for each child. For the Galician group, exclusionary criteria for this sample included Cerebral Palsy (as diagnosed up until 9 months of age), Periventricular Leukomalacia (PVL), Intraventricular Hemorrhage (IVH) greater than grade II, hydrocephalus, encephalopathy, genetic malformations, chromosomal syndromes, metabolic syndromes associated to mental retardation, or important motor or sensorial impairments.
The PR Mexican sample was obtained as part of another large study at the Unidad X [67,70]. Two different samples were obtained from different project within the center and were independently assigned to each study. Infants participated in a range of neuropsychological tests, and the Bayley Scales [86] was used as a neurodevelopmental measure. Infants with scores that showed significant delays on the neurodevelopmental measures and motor or sensorial impairments were not included. The motor intervention sample (GP3) was part of the initial research project at the XXX whereas the GP4 (motor and language intervention) infants participated in the early intervention program that was developed as part of a specific research project [69]. Before the study, when infants were between 42 and 46 weeks of age (corrected) a clinical neuropediatric assessment [87] was carried out to identify non-normal neuropsychological signs that could be signify problems other than NC-PVL. Magnetic Resonance Imaging (fMRI) using a Phillips Intera of 1 Tesla was completed in order to diagnose NC-PVL, which was an inclusionary criterion for both Mexican samples. A clinical EEG was also obtained for all infants to determine whether electrical cerebral activity was normal. Visual and Auditory Evoked Potentials (VEPs and AEPs) were intact. Infants with cystic PVL, cerebral hemorrhages, brain infarcts, brain malformations or other pathological lesions apart from diffuse PVL were excluded.
The motor intervention that both Mexican groups (GP3 and GP4) received was based on Katona neurohabilitation [56,57,62]. Intervention began immediately after birth and continued throughout the study to take advantage of the plasticity of the central nervous system. Sessions were held on a weekly basis with active parental participation encouraged. Exercises were continued at home, as well.
In addition, GP4 also received early language intervention, along with the motor intervention. Mothers met individually with a certified speech-language pathologist biweekly for a total of 12 hourly training sessions focused on enriching infant communication development and parent training [88,89]. Intervention began, again, at birth or within the first month of age. Targeted topics included: (1) understanding the course of typical language development; (2) increasing sensitivity to the infants’ cues [88,89]; (3) creating a supportive environment for learning and growing; (4) applying focused stimulation [90,91]; (5) using infant-directed speech [50,92,93]; (6) increasing the quantity, quality, and responsitivity of communication [94]; (7) providing appropriate auditory stimulation [95]; and, (8) promoting early literacy experiences [96,97] Mothers first observed the speech-language pathologist using the targeted strategies with their infants. They then applied the same strategies with their infants while receiving immediate verbal and visual feedback to improve their interactions. In addition, an easy-to-read information sheet on each topic was provided in order to facilitate home review of the topic. Mothers were assigned work to do at home between training sessions in order to facilitate continued practice of the communication strategies in the home environment. The last training session was a review of all presented topics by means of a questionnaire.
Infants in the Galician study were part of a larger longitudinal study [18,68,81]. Families were initially contacted through the hospital setting and asked to participate. Infants were not in early intervention programs after hospital discharge. At 15 days of age (after birth) the infants were evaluated with the Neonatal Behavioral Assessment Scale (NBAS) [84,85]. Preterm infants scored higher in motor and range of state cluster, while FT infants had higher scores in regulation of state clusters. At that time, the mothers of the infants participated in a long interview in which family environment and general health information was obtained for each child. For the Galician group, exclusionary criteria for this sample included Cerebral Palsy (as diagnosed up until 9 months of age), Periventricular Leukomalacia (PVL), Intraventricular Hemorrhage (IVH) greater than grade II, hydrocephalus, encephalopathy, genetic malformations, chromosomal syndromes, metabolic syndromes associated to mental retardation, or important motor or sensorial impairments.
The PR Mexican sample was obtained as part of another large study at the Unidad X [67,70]. Two different samples were obtained from different project within the center and were independently assigned to each study. Infants participated in a range of neuropsychological tests, and the Bayley Scales [86] was used as a neurodevelopmental measure. Infants with scores that showed significant delays on the neurodevelopmental measures and motor or sensorial impairments were not included. The motor intervention sample (GP3) was part of the initial research project at the XXX whereas the GP4 (motor and language intervention) infants participated in the early intervention program that was developed as part of a specific research project [69]. Before the study, when infants were between 42 and 46 weeks of age (corrected) a clinical neuropediatric assessment [87] was carried out to identify non-normal neuropsychological signs that could be signify problems other than NC-PVL. Magnetic Resonance Imaging (fMRI) using a Phillips Intera of 1 Tesla was completed in order to diagnose NC-PVL, which was an inclusionary criterion for both Mexican samples. A clinical EEG was also obtained for all infants to determine whether electrical cerebral activity was normal. Visual and Auditory Evoked Potentials (VEPs and AEPs) were intact. Infants with cystic PVL, cerebral hemorrhages, brain infarcts, brain malformations or other pathological lesions apart from diffuse PVL were excluded.
The motor intervention that both Mexican groups (GP3 and GP4) received was based on Katona neurohabilitation [56,57,62]. Intervention began immediately after birth and continued throughout the study to take advantage of the plasticity of the central nervous system. Sessions were held on a weekly basis with active parental participation encouraged. Exercises were continued at home, as well.
In addition, GP4 also received early language intervention, along with the motor intervention. Mothers met individually with a certified speech-language pathologist biweekly for a total of 12 hourly training sessions focused on enriching infant communication development and parent training [88,89]. Intervention began, again, at birth or within the first month of age. Targeted topics included: (1) understanding the course of typical language development; (2) increasing sensitivity to the infants’ cues [88,89]; (3) creating a supportive environment for learning and growing; (4) applying focused stimulation [90,91]; (5) using infant-directed speech [50,92,93]; (6) increasing the quantity, quality, and responsitivity of communication [94]; (7) providing appropriate auditory stimulation [95]; and, (8) promoting early literacy experiences [96,97] Mothers first observed the speech-language pathologist using the targeted strategies with their infants. They then applied the same strategies with their infants while receiving immediate verbal and visual feedback to improve their interactions. In addition, an easy-to-read information sheet on each topic was provided in order to facilitate home review of the topic. Mothers were assigned work to do at home between training sessions in order to facilitate continued practice of the communication strategies in the home environment. The last training session was a review of all presented topics by means of a questionnaire.
DATA ANALYSIS
In order to test our hypothesis, we performed parametrical tests, t tests and ANOVAs when required. To test the effect size, we use Cohen d in t tests, omega square (ω2) in one way ANOVAs or eta square (?p2) in repeated measures ANOVAs.
We first examined gender effects and as no differences were found we did not consider gender in the rest of the analysis. Birth weight (BW) and Gestational Age (GA) effects were also analyzed in the first three groups to determine homogeneity. As groups were similar and our goal was not to analyze effects of these medical factors, further analysis will not be reported here for these variables. The rest of the analysis that was carried out was to determine the effect of three levels of intervention (GP2-no intervention, GP3-motor only and GP4-motor plus language) on vocabulary comprehension and production. As mentioned previously, percent reported scores for words comprehended and produced were calculated. Descriptive data for vocabulary comprehension and production are reported in Table 1.
We first examined gender effects and as no differences were found we did not consider gender in the rest of the analysis. Birth weight (BW) and Gestational Age (GA) effects were also analyzed in the first three groups to determine homogeneity. As groups were similar and our goal was not to analyze effects of these medical factors, further analysis will not be reported here for these variables. The rest of the analysis that was carried out was to determine the effect of three levels of intervention (GP2-no intervention, GP3-motor only and GP4-motor plus language) on vocabulary comprehension and production. As mentioned previously, percent reported scores for words comprehended and produced were calculated. Descriptive data for vocabulary comprehension and production are reported in Table 1.
RESULTS
We explored the relation between the groups with intervention (motor and/or language) and without intervention in relation to vocabulary comprehension and production. G1 was a full term group, with no intervention, Group 2 had no intervention, GP3 had motor stimulation, GP4 received motor and language stimulation, as described above. A two way ANOVA analysis was carried out in which the group factor was intervention (none, motor, motor and language,) and the repeated measure factor was vocabulary comprehension and production.
Table 1 presents descriptive information for each group of infants. It should be noted that descriptive statistics were not run for corrected age for GPs 1 and 2, as all children were seen at 10 months of age (plus or minus 15 days). A t-test of independent measures yielded no significant differences (p = .41) between the other two PR groups (with intervention) for corrected age (GP3, M = 11.4, SD = 1.6; GP4, M = 10.7, SD = 1.31).
Tests on vocabulary measures were run to determine differences between groups. As would be expected, there were significant differences between language comprehension and production, F(1,3) = 285.862, p < .001, ?p2 = 0.704). There was also a main effect of group, F(3,120) = 10.952, p < .001, ?p2 = 0.177. Next, the effects of intervention on both comprehension and production were analyzed. There was a significant interaction between group and repeated measures factor (comprehension and production), F(3,120) = 7.317, p < .001, ?p2 = .215. A post-hoc Bonferroni correction revealed significant differences between GP2 (PR, no intervention) and GP4 (PR, language and motor intervention) (p < .001), and between GP4 (PR, language and motor intervention) and GP1 (full term) (p < .001). The effects of intervention were strongest between the PR group that received no intervention and the combination of both language/motor intervention groups (p < .001) for both comprehension and production. What is interesting is that there was a significant difference favoring PR infants when compared to FT infants. Thus, early stimulation seems to have an impact on language development in general.
There was a larger effect on comprehension than on production (Figures 1 and 2). A one way ANOVA test for each language module (comprehension and production) yielded a significant difference between groups only in comprehension, F(3,120) = 10.012, p < .01 ω2 = .179. A Bonferroni post-hoc revealed significant differences between GP2 (PR, no intervention) and GP4 (PR, language and motor intervention) (p < .001), between GP4 (PR, language and motor intervention) and G1 (full term) (p < .001), and between GP3 (PR, motor intervention) and G1 (full term) (p < .001). No significant differences were found for vocabulary between GP 2 (PR, no intervention) and GP3 (PR, motor intervention). Thus, it appears, as would be expected because of the young age, that intervention had a stronger effect on comprehension than on production. Production levels were very low at this age and, thus any effects may be a product of the scarcity of vocabulary.
Table 1 presents descriptive information for each group of infants. It should be noted that descriptive statistics were not run for corrected age for GPs 1 and 2, as all children were seen at 10 months of age (plus or minus 15 days). A t-test of independent measures yielded no significant differences (p = .41) between the other two PR groups (with intervention) for corrected age (GP3, M = 11.4, SD = 1.6; GP4, M = 10.7, SD = 1.31).
Tests on vocabulary measures were run to determine differences between groups. As would be expected, there were significant differences between language comprehension and production, F(1,3) = 285.862, p < .001, ?p2 = 0.704). There was also a main effect of group, F(3,120) = 10.952, p < .001, ?p2 = 0.177. Next, the effects of intervention on both comprehension and production were analyzed. There was a significant interaction between group and repeated measures factor (comprehension and production), F(3,120) = 7.317, p < .001, ?p2 = .215. A post-hoc Bonferroni correction revealed significant differences between GP2 (PR, no intervention) and GP4 (PR, language and motor intervention) (p < .001), and between GP4 (PR, language and motor intervention) and GP1 (full term) (p < .001). The effects of intervention were strongest between the PR group that received no intervention and the combination of both language/motor intervention groups (p < .001) for both comprehension and production. What is interesting is that there was a significant difference favoring PR infants when compared to FT infants. Thus, early stimulation seems to have an impact on language development in general.
There was a larger effect on comprehension than on production (Figures 1 and 2). A one way ANOVA test for each language module (comprehension and production) yielded a significant difference between groups only in comprehension, F(3,120) = 10.012, p < .01 ω2 = .179. A Bonferroni post-hoc revealed significant differences between GP2 (PR, no intervention) and GP4 (PR, language and motor intervention) (p < .001), between GP4 (PR, language and motor intervention) and G1 (full term) (p < .001), and between GP3 (PR, motor intervention) and G1 (full term) (p < .001). No significant differences were found for vocabulary between GP 2 (PR, no intervention) and GP3 (PR, motor intervention). Thus, it appears, as would be expected because of the young age, that intervention had a stronger effect on comprehension than on production. Production levels were very low at this age and, thus any effects may be a product of the scarcity of vocabulary.
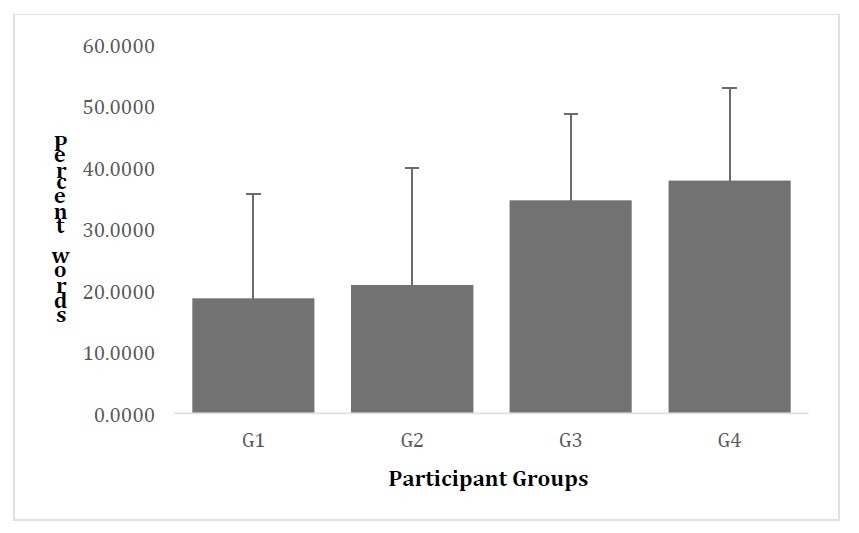
Figure 1: Percent Words Reported Comprehended by Participant Groups.
Note: G1 = Full term group, G2= Premature with no PVL or intervention group, G3 = Premature with PVL and motor intervention group, G4= Premature with PVL and motor/language intervention.
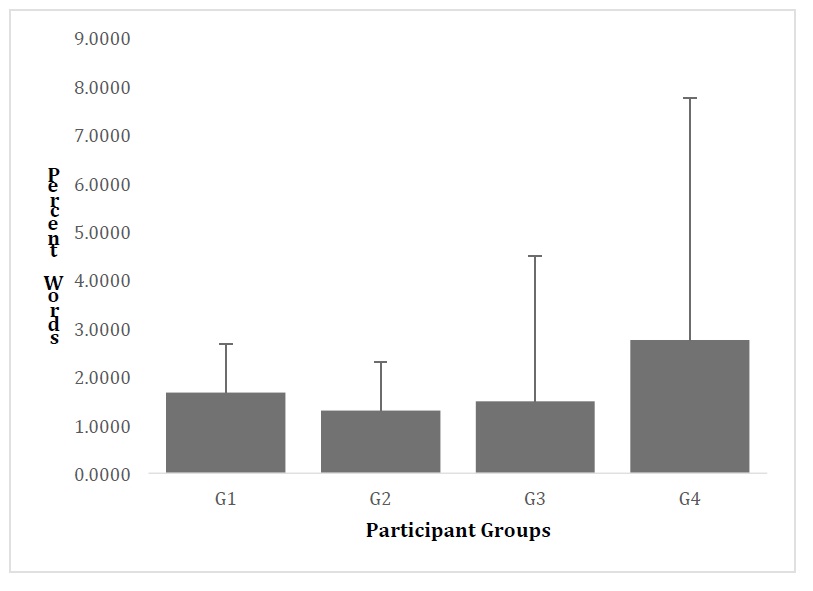
Figure 2: Percent Words Reported Produced by Participant Groups.
Note: G1 = Full term group, G2= Premature with no PVL or intervention group, G3 = Premature with PVL and motor intervention group, G4= Premature with PVL and motor/language intervention.
DISCUSSION AND CONCLUSION
This study addresses the effects of prematurity and intervention on vocabulary comprehension and production by comparing three cohorts of Preterm (PT) infants who did and did not receive intervention between the ages of 10 and 14 months. A group of FT infants was included as a reference.
One of the major issues at stake in this paper is the effect of early intervention on language development. As previously noted, there is scant literature on the effects of intervention in preterm Spanish-speaking samples, and much less on the effect of Katona and early language intervention programs. The available literature has stated that early intervention, of multiple types, has a positive effect on later development [37,44]. Some studies have analyzed specific intervention programs, but seldom, if ever, consider the relationship between physical or motor and language intervention. In this paper we explored a dynamic physical therapy system for which little evidence has been reported and a language intervention program that has parameters similar to programs previously reported on in the literature [88,89,98]. Our results illuminate differences based on intervention types and for language comprehension and production.
We first explored socio-economic and medical characteristics of our populations to determine if there were differences among groups. Most mothers had more than High School education, thus this socio-economic factor was not a variable that was included in the analysis. Mother’s education, as a means for analyzing socio-economic status is a determining factor in this and most populations. The fact that our sample was restricted in this sense is a limitation of the study and does not allow for extensive generalizations. Medical aspects, particularly birth weight and gestational age were also homogenous across groups and, thus, were not further explored. The goals of the study were restricted to a more homogeneous sample, and thus, effects from these variables were not measured. Also, it is possible, as proposed in other studies, that differences may appear at later stages of development [28,33,99] or only for infants with extremely low birth weight or gestational age who are at higher risk for language development problems. Both of these issues merit more in depth analysis that should be the focus of future research that includes longitudinal samples.
This discussion will concentrate on the main purpose of our study, to analyze differences in comprehension and production of early vocabulary based on different types of intervention. All results clearly reflect variability within the sample. This would not suggest a defect of the instrument, but rather support what has been proposed in language development research [71,77]. It must be recalled, as well, that vocabulary production is very low at the ages studied, regardless of premature birth or its associated complications [99]. Longitudinal studies could possibly answer questions related to later effects of prematurity on language production. At these early ages (10 to 14 months), effects may not yet be present. Thus, comprehension data may best answer our research questions. Results, taking into account post-hoc calculations, indicated that vocabulary scores were related to the type of intervention received. We must recall that GP 4 (PR with language and motor intervention) participated in an early language intervention program that underscored parental participation along with specific interactional components thought to boost communicative skills. This group had the highest vocabulary scores. In all cases, and as is expected because of the young age of the participating infants, there were larger effects for comprehension than for production.
When taking into account the motor intervention group (GP3), based on our hypothesis, we would have also expected higher scores in in their vocabulary when compared to the no-intervention (GP2) group. Contrary to our hypothesis, Group 3 was not significantly different when comparing it to the other groups. It is possible, as reported elsewhere [57], that effects could be found for neurodevelopmental factors, though not for vocabulary development. To further explore this relation, a larger, more diverse sample, would be required as it is has been shown that motor development is related to language [100,101].
Although statistical results are extremely important, tendencies can be observed in figures 1 and 2 that illustrate percent number of words. Here we can see that both groups that receive intervention had higher scores (though not all have significant differences) than both the FT term and the no-intervention (GP2) groups in language comprehension. There does seem to be a different pattern for language production. In this case the FT group is similar to the language intervention group (GP4). We must take into consideration, as well, that both GP3 and GP4 were at a slight medical risk as they were identified with NC-PVL. Still, their language scores were found to be higher than infants who were not experiencing this risk factor, and who received no intervention.
To our knowledge, this is the first study of its kind study to explore the effect of different modalities of intervention on early communicative skills in preterm infants. We propose that early interventions that combine motor and language training techniques, particularly with high parent participation, can have effects on language outcomes in the first year of life.
One apparent weakness of this research is that we did not obtain language measures prior to administering the intervention. As a result, we do not know with certainty if the four groups were comparable in their initial language abilities. However, it is necessary to take into consideration that few, if any, reliable language measures are available for children younger than 8 months of age because children’s first words usually appear between 10 and 12 months of age [71,102]. Further, data from other behavioral and observational language measures could add to the understanding of the infant’s communicative abilities. Follow up studies when the infants are older could also be beneficial. This would entail creating large longitudinal cohorts with more diverse populations, as well to the effect of maternal education or other factors on the communicative abilities of PR infants. There is a need for such research.
One of the major issues at stake in this paper is the effect of early intervention on language development. As previously noted, there is scant literature on the effects of intervention in preterm Spanish-speaking samples, and much less on the effect of Katona and early language intervention programs. The available literature has stated that early intervention, of multiple types, has a positive effect on later development [37,44]. Some studies have analyzed specific intervention programs, but seldom, if ever, consider the relationship between physical or motor and language intervention. In this paper we explored a dynamic physical therapy system for which little evidence has been reported and a language intervention program that has parameters similar to programs previously reported on in the literature [88,89,98]. Our results illuminate differences based on intervention types and for language comprehension and production.
We first explored socio-economic and medical characteristics of our populations to determine if there were differences among groups. Most mothers had more than High School education, thus this socio-economic factor was not a variable that was included in the analysis. Mother’s education, as a means for analyzing socio-economic status is a determining factor in this and most populations. The fact that our sample was restricted in this sense is a limitation of the study and does not allow for extensive generalizations. Medical aspects, particularly birth weight and gestational age were also homogenous across groups and, thus, were not further explored. The goals of the study were restricted to a more homogeneous sample, and thus, effects from these variables were not measured. Also, it is possible, as proposed in other studies, that differences may appear at later stages of development [28,33,99] or only for infants with extremely low birth weight or gestational age who are at higher risk for language development problems. Both of these issues merit more in depth analysis that should be the focus of future research that includes longitudinal samples.
This discussion will concentrate on the main purpose of our study, to analyze differences in comprehension and production of early vocabulary based on different types of intervention. All results clearly reflect variability within the sample. This would not suggest a defect of the instrument, but rather support what has been proposed in language development research [71,77]. It must be recalled, as well, that vocabulary production is very low at the ages studied, regardless of premature birth or its associated complications [99]. Longitudinal studies could possibly answer questions related to later effects of prematurity on language production. At these early ages (10 to 14 months), effects may not yet be present. Thus, comprehension data may best answer our research questions. Results, taking into account post-hoc calculations, indicated that vocabulary scores were related to the type of intervention received. We must recall that GP 4 (PR with language and motor intervention) participated in an early language intervention program that underscored parental participation along with specific interactional components thought to boost communicative skills. This group had the highest vocabulary scores. In all cases, and as is expected because of the young age of the participating infants, there were larger effects for comprehension than for production.
When taking into account the motor intervention group (GP3), based on our hypothesis, we would have also expected higher scores in in their vocabulary when compared to the no-intervention (GP2) group. Contrary to our hypothesis, Group 3 was not significantly different when comparing it to the other groups. It is possible, as reported elsewhere [57], that effects could be found for neurodevelopmental factors, though not for vocabulary development. To further explore this relation, a larger, more diverse sample, would be required as it is has been shown that motor development is related to language [100,101].
Although statistical results are extremely important, tendencies can be observed in figures 1 and 2 that illustrate percent number of words. Here we can see that both groups that receive intervention had higher scores (though not all have significant differences) than both the FT term and the no-intervention (GP2) groups in language comprehension. There does seem to be a different pattern for language production. In this case the FT group is similar to the language intervention group (GP4). We must take into consideration, as well, that both GP3 and GP4 were at a slight medical risk as they were identified with NC-PVL. Still, their language scores were found to be higher than infants who were not experiencing this risk factor, and who received no intervention.
To our knowledge, this is the first study of its kind study to explore the effect of different modalities of intervention on early communicative skills in preterm infants. We propose that early interventions that combine motor and language training techniques, particularly with high parent participation, can have effects on language outcomes in the first year of life.
One apparent weakness of this research is that we did not obtain language measures prior to administering the intervention. As a result, we do not know with certainty if the four groups were comparable in their initial language abilities. However, it is necessary to take into consideration that few, if any, reliable language measures are available for children younger than 8 months of age because children’s first words usually appear between 10 and 12 months of age [71,102]. Further, data from other behavioral and observational language measures could add to the understanding of the infant’s communicative abilities. Follow up studies when the infants are older could also be beneficial. This would entail creating large longitudinal cohorts with more diverse populations, as well to the effect of maternal education or other factors on the communicative abilities of PR infants. There is a need for such research.
CLINICAL IMPLICATIONS
The main contribution of this study is the confirmation of the beneficial effect of early intervention in the promotion of first language development in a population of Spanish-speaking infants outside of the United States. In addition, differential effects were demonstrated in regards to the modality of intervention, with the greatest benefit gained by an intervention that combined motor and communicative goals. Infants who are at risk for developmental problems because of prematurity may outperform even full term infants when early intervention is provided.
ACKNOWLEDGEMENT
This research was supported by grants to second author from the Ministerio de Ciencia e Innovación of the Spanish Government (grants PSI2008-03905 and PSI2011-23210) and the Xunta de Galicia (INCITE) (grant PGIDIT07PXIB211044PR) and to the third author from DGPA, PAPIIT IN205605 and PAPIIT IN220110, CONACyT (36263-M, SA-LUD-2002-C01-7074 and 46270-Y) and CONCyTEQ (60), Fondo Mixto (QRO-04-C01-16) in Mexico.
REFERENCES
- Hamilton BE, Martin JA, Ventura SV (2013) Births: Preliminary data from 2012. Natl Vital Stat Rep 62: 1-20.
- Howson, CP, Kinney MV, Lawn LE (2012) Born Too Soon: The Global Action Report on Preterm Birth. March of Dimes, PMNCH, Save the Children, World Heath Organization, Geneva, Switzerland.
- Ramón MR, del Rocío CCP, Aguli RRR, Marcelino HV (2014) Incidencia de nacimientos pretermino en el IMSS (2007-2012). Ginecol Obstet Mex 82: 465-471.
- Miranda-Del-Olmo H, Cardiel-Marmolejo LE, Reynoso E, Oslas LP, Acosta-Gómez Y et al. (2003) Morbilidad y mortalidad en el recien nacido prematuro del Hospital General de Mexico. Revista Medica Del Hospital General, De Mexico 66: 22-28.
- Moro-Serrano M, Fernandez-Perez C, Figueras-Alloy J, Perez-Rodríguez J, Coll E, et al. (2008) SEN 1500: diseño y desarrollo del registro de niños de menos de 1500 gr al nacer en España. Anales de Pediatría 68: 181-188.
- Kallankari H, Kaukola T, Olsen P, Ojaniemi M, Hallman M, et al. (2015) Very preterm birth and foetal growth restriction are associated with specific cognitive deficits in children attending mainstream school. Acta Paediatr 104: 84-90.
- McGowan JE, Alderdice FA, Holmes VA, Johnston L (2011) Early childhood development of late-preterm infants: a systematic review. Pediatrics 127: 1111-1124.
- Ortiz-Mantilla S, Choudhury N, Leevers H, Benasich AA (2008) Understanding language and cognitive deficits in very low birth weight children. Dev Psychobiol 50: 107-126.
- Petrini JR, Dias T, McCormick MC, Massolo ML, Green NS, et al. (2009) Increased risk of adverse neurological development for late preterm infants. J Pediatr 154: 169-176.
- Velikos K, Soubasi V, Michalettou I, Sarafidis K, Nakas C, et al. (2015) Bayley-III scales at 12 months of corrected age in preterm infants: Patterns of developmental performance and correlations to environmental and biological influences. Res Dev Disabil 45-46: 110-119.
- Woythaler MA, McCormick MC, Smith VC (2011) Late preterm infants have worse 24-month neurodevelopmental outcomes than term infants. Pediatrics 127: 622-629.
- Baumeister AA, Bacharach VR (1996) A critical analysis of the infant health and development program. Intelligence 23: 79-104.
- Martin JA, Osterman MJ, Sutton PD (2010) Are preterm births on the decline in the United States? Recent data from the National Vital Statistics System. NCHS data brief 39: 1-8.
- Aylward GP (2005) Neurodevelopmental outcomes of infants born prematurely. J Dev Behav Pediatr 26: 427-440.
- Currie J (2005) Health disparities and gaps in school readiness. Future Child 15: 117-138.
- Teti DM, Black MM, Viscardi R, Glass P, O'Connell MA, et al. (2009) Intervention with African American Premature Infants Four-Month. Results of an early intervention program. Journal of Early Intervention 31.
- Volpe JJ (2003) Cerebral white matter injury of the premature infant-more common than you think. Pediatrics 112: 176-180.
- Perez-Pereira M, Fernández P, Gómez-Taibo ML, Resches M (2014) Language development of low risk preterm infants up to the age of 30 months. Early Hum Dev 90: 649-656.
- Orcesi S, Olivieri I, Longo S, Perotti G, La Piana R, et al. (2012) Neurodevelopmental outcome of preterm very low birth weight infants born from 2005 to 2007. European Journal of Paediatric Neurology 16: 716-723.
- Wild KT, Betancourt LM, Brodsky NL, Hurt H (2013) The effect of socioeconomic status on the language outcome of preterm infants at toddler age. Early Hum Dev 89: 743-746
- Counsell S, Allsop J, Harrison M, Larkman DJ, Kennea NL, et al. (2003) Diffusion-weighted imaging of the brain in preterm infants with focal and diffuse white matter abnormality. Pediatrics 112: 1-7.
- Melhem ER, Hoon AH, Ferrucci JT, Quinn CB, Reinherdt EM, et al. (2000) Periventricular Leukomalacia: Relationship between Lateral Ventricular. Radiology 214.
- Volpe J (2009) Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. The Lancet Neurology 8: 110-124.
- Foster-Cohen SH, Edgin JO, Champion PR, Woodward LJ (2007) Early delayed language development in very preterm infants: evidence from the MacArthur–Bates CDI. J Child Lang 34: 655-675.
- Guarini A, Sansavini A, Fabbri C, Alessandroni R, Faldella G, et al. (2009) Reconsidering the impact of preterm birth on language outcome. Early Hum Dev 85: 639-645.
- Kern S, Gayraud F (2007) Influence of preterm birth on early lexical and grammatical acquisition. First Language 27.
- Plomgaard AM, Hansen BM, Greisen G (2006) Measuring developmental deficit in children born at gestational age less than 26 weeks using a parent-completed developmental questionnaire. Acta Pædiatr 95: 1488-1494.
- Stolt S, Lehtonen L, Haataja L, Lapinleimu H (2012) The development and predictive value of early vocalizations in prematurely born very-low-birth-weight children: a longitudinal study. Clin Linguist Phon 26: 414-422.
- Miguel P, Carmen FPD, Mariela R, Maria Luisa G, Manuel P (2011) Desarrollo linguístico y comunicativo temprano de niños prematuros Rev. logop. Foniatr. Audiol 31: 148-59.
- Bosch L (2011) Precursors to language in preterm infants: speech perception abilities in the first year of life. Prog Brain Res 189: 239-257.
- Bosch L, Ramon-Casas M, Sole J, Nícar L, Iriondo-Sanz M (2011) Desarrollo lexico en el prematuro: medidas del vocabulario expresivo en el segundo año de vida [Lexical development in premature babies: expressive vocabulary measures in the second year of life]. Revista de Logopedia, Foniatría y Audiología 31: 169-179.
- Sansavini A, Guarini A, Alessandroni R, Faldella G, Giovanelli G, et al. (2006) Early relations between lexical and grammatical development in very immature Italian preterms. J Child Lang 33: 199-216.
- Ohgi S, Arisawa K, Takahashi T, Kusumoto T, Goto Y, et al. (2003) Neonatal behavioral assessment scale as a predictor of later developmental disabilities of low birth-weight and/or premature infants. Brain Dev 25: 313-321.
- Stolt S, Haataja L, Lapinleimu H, Lehtonen L (2009) The early lexical development and its predictive value to language skills at 2 years in very-low-birth-weight children. Journal of Commun Disord 42: 107-123
- Landry SH, Smith KE, Swank PR (2002) Environmental effects of language development in normal and high-risk child populations. Seminars in Pediatric Neurology 9: 192-200.
- Litt JS, Perrin JM (2014) Influence of clinical and sociodemographic characteristics on early intervention enrollment after NICU discharge. Journal of Early Intervention 36.
- Guralnick, MJ (2012) Preventive interventions for preterm children: Effectiveness and developmental mechanisms. J Dev and BehavPediatr 33: 352-364.
- Ravn IH, Lars-Smith NA, Smeby N, Kynoe K, Sandvik L, et al. (2012) Effects of early mother–infant intervention on outcomes in mothers and moderately and late preterm infants at age 1 year: a randomized controlled trial. Infant Behav Dev 35: 36-47.
- Jansson-Verkasalo E, Ceponiene R, Valkama M, Vainionpa L, Laitakari K, et al. (2003) Deficient speech-sound processing, as shown by the electrophysiologic brain mismatch negativity response, and naming ability in prematurely born children. Neurosci Lett 348: 5-8.
- McCormick MC, Brooks-Gunn J, Buka SL, Goldman J, Yu J, Salganik M, et al. (2006) Early intervention in low birth weight premature infants: Results at 18 years of age for the Infant Health and Development Program. Pediatrics 117: 771-780.
- Sansavini A, Savini S, Guarini A, Broccoli S, Alessandroni R, et al. (2011) The effect of gestational age on developmental outcomes: a longitudinal study in the first 2 years of life. Child Care Health & Dev 37: 26-36.
- Schults A, Tulviste T, Haan E (2013) Early vocabulary in full term and preterm Estonian children. Early Hum Dev 89: 721-726.
- Guralnick MJ (2008) International perspectives on early intervention A search for common ground. Journal of Early Intervention 30: 90-101.
- Guralnick MJ (2011) Why Early Intervention Works: A Systems Perspective. Infants Young Child 24: 6-28.
- Kiechl-Kohlendorfer U, Merkle U, Deufert D, Neubauer V, Peglow UP, et al. (2015) Effect of developmental care for very premature infants on neurodevelopmental outcome at 2 years of age. Infant Behav & Dev 39: 166-172.
- Kynø NM, Ravn IH, Lindemann R, Fagerland MW, Smeby NA, et al. (2012) Effect of an early intervention programme on development of moderate and late preterm infants at 36 months a randomized controlled study. Infant Behav Dev 35: 916-926.
- Prats-Viñas JM (2007) A favor de la detección precoz e intervencionismo moderado: ¿Hasta que punto es efectiva? Revista de Neurología 44: 35-37.
- Orton J, Spittle A, Doyle L, Anderson P (2009) Do early intervention programmes improve cognitive and motor outcomes for preterm infants after discharge? A systematic review. Dev Med and Child Neurol 51: 851-859.
- Rodríguez-Ogando A, Miranda-Herrera P, Castro-de Castro P, Vázquez-López M, & Blanco-Bravoc D, et al. (2011) Estimulación precoz en los recien nacidos con peso al nacer entre 1.000 y 1.500 g. ¿Es siempre necesaria? Anales de Pediatría 75: 161-168.
- Thiessen, ED, Hill EA, Saffran JR (2005) Infant-directed speech facilitates word segmentation. Infancy 7: 53-71.
- DeGangi GA (1994) Examining the efficacy of short-term NDT intervention using a case study design: Part 2. Physical & Occupational Therapy in Pediatrics 14: 21-61.
- Jonsdottir J, Fetters L, Kluzik J (1997) Effects of physical therapy on postural control in children with Cerebral Palsy. Pediatric Physical Therapy 9.
- Knox V, Evans AL (2002) Evaluation of the functional effects of a course of Bobath therapy in children with cerebral palsy a preliminary study. Dev Med Child Neurol 44: 447-460.
- Ottenbacher KJ, Biocc Z, DeCremer G, Gevelinger M, Jedlovec KB, et al. (1986) Quantitative analysis of the effectiveness of pediatric therapy. Emphasis on the neurodevelopmental treatment approach. Phys Ther 66: 1095-1101.
- Girolami GL, Campbell SK (1994) Efficacy of a Neuro-Developmental Treatment program to improve motor control in infants born prematurely. Pediatric Physical Therapy 6.
- Barrera-Resendiz J (2010) Manual of Neurohabilitatory Therapy. National Autonomous University of Mexico, Mexico, USA.
- Harmony T, Barrera-Resendiz J, Juárez-Colín ME, Carrillo-Prado C, Pedraza-Aguilar M, et al. (2016) Longitudinal study of children with perinatal brain damage in whom early neurohabilitation was applied: Preliminary report. Neuroscience letters 611: 59-67.
- Katona F (1982) Investigación del comportamiento sensorio motriz. In Katona F (ed.). Manual de prevención, diagnóstico y habilitación precoz de los daños cerebrales en el recien nacido y los primeros meses de la vida. Instituto Internacional para la Investigacio?n y Asesoramiento para la Deficiencia Mental, Madrid, Spain.
- Katona F (1983) An orienting diagnostic system in neonatal and infantile neurology. Acta Paediatr Hung 24: 299-314.
- Katona F (1988) Developmental clinical neurology and neurohabilitation in the secundary prevention of pre and perinatal injuries of the brain. In: Vietze P, Vaughon H (eds.). Early identification of infants with developmental disabilities. Allyn and Bacon, Boston, Massachusetts, USA.
- Katona F (1989) Clinical neuro-developmental diagnosis and treatment. In Zelazo PR, Barr RG (eds.). Challenges to developmental paradigms: Implications for theory and treatment. Lawrence Erlbaum Assoc, New Jersey, USA. Pg no: 167-187.
- Porras-Katz E, Harmony T (2007) Neurohabilitación: un metodo diagnóstico y terapeutico para prevenir secuelas por lesión cerebral en el recien nacido y el lactante. Bol Med del Hosp Infant Mex 64: 125-135.
- Mayston MJ (2001) People with cerebral palsy: effects of and perspectives for therapy. Neural Plasticity 8: 51-69.
- Mayston MJ (2001) The Bobath concept today. Synapse Synapse-Association of Chartered Physiotherapists Interested in Neurology. Pg no: 32-35.
- Alvarado-Guerrero I, Poblano A, Marosi E, Corsi-Cabrera M, Otero-Ojeda GA (2011) Early intervention in the neurodevelopment of premature infants during the first six months of life. Neuroscience and Medicine 2: 104-109.
- Alvarado-Ruiz GA, Martínez-Vázquez I, Sánchez C, Solís-Chan M, Mandujano-Valdes M (2012) Los movimientos elementales complejos del humano: Desarrollo postnatal. Reporte preliminar de nueve lactantes mexicanos Salud Mental 35: 99-107.
- Avecilla-Ramírez G, Harmony T, Porras-Kattz E, Ricardo-Garcell J, Fernández-Bouzas A, et al. (2012) Indicadores electrofisiológicos de la percepción fonetica en lactantes con riesgo de trastornos del lenguaje. Ciencia@UAQ 3: 14-26.
- Perez-Pereira M, Fernández P, Resches M, Taibo MLG (2013) Determinants of early language and communication in preterm and full term infants: A comparative study. Enfance 65: 59-76.
- Authors (2016) Efectos de estimulación temprana sobre el desarrollo de lenguaje de bebes prematuros. In: Bowater R (ed.). Investigación Cuantitativa y la Estadística en la UAQ. Queretaro: Universidad Autónoma de Queretaro, Mexico.
- Avecilla-Ramírez GN, Ruiz-Correa S, Marroquin JL, Harmony T, Alba A, et al. (2011) Electrophysiological auditory responses and language development in infants with periventricular leukomalacia. Brain Lang 119: 175-183.
- Fenson L, Marchman VA, Thal DJ, Dale PS, Reznick JS, et al. (2006) The MacArthur–Bates Communicative Development Inventories (CDIs): Users Guide and Technical Manual, (2nd edn), Communication and Language, Brookes Publishing Co, Baltimore, MD, USA.
- Jackson-Maldonado D, Thal D, Marchman V, Bates E, Gutierrez-Clellen V (1993) Early lexical development in Spanish-speaking infants and toddlers. J Child Lang 20: 523-549.
- Bates E, Bretherton I, Snyder L (1988) From First Words to Grammar: Individual Differences and Dissociable Mechanisms. Cambridge University Press 10.
- Mayor J, Plunkett K (2011) A statistical estimate of infant and toddler vocabulary size from CDI analysis. Dev Sci 14: 769-785.
- Fenson L, Dale PS, Reznick JS, Bates E, Thal DJ, et al. (1993) The MacArthur Communicative Development Inventories: Users Guide and Technical Manual, Brookes, Baltimore, MD, USA.
- Dale PS, Penfold M (2011) Adaptations of the MacArthur-Bates CDI into non-US English languages.
- Law J, Roy P (2008) Parental report of infant language skills: A review of the development and application of the Communicative Development Inventories. Child and Adolescent Mental Health 13: 198-206.
- Fenson L, Dale PS, Reznick JS, Bates E, Thal DJ, et al. (1994) Variability in early communicative development. Monogr Soc Res Child Dev 59: 1-173.
- Nelson K (1981) Individual differences in language development: Implications for development and language. Developmental psychology 17: 170-187.
- Fenson L (2003) MacArthur Inventarios Del Desarrollo de Habilidades Comunicativas: User's Guide and Technical Manual. Brookes PH, Baltimore, USA.
- Perez-Pereira M, Resches M (2011) Concurrent and predictive validity of the Galician CDI. J Child Lang 38: 121-140.
- Pereira MP, Soto XRG (2003) El diagnóstico del desarrollo comunicativo en la primera infancia: adaptación de las escalas MacArthur al gallego. Psicothema 15: 352-361.
- Sansavini A, Guarini A, Savini S, Broccoli S, Justice L, et al. (2011) Longitudinal trajectories of gestural and linguistic abilities in very preterm infants in the second year of life. Neuropsychologia 49: 3677-3688.
- Perez-Pereira M, Fernandez P, Gómez-Taibo M, Gonzalez L, Trisac JL, et al. (2013) Neurobehavioral development of preterm and full term children: biomedical and environmental influences. Early Hum Dev 89: 401-409.
- Brazelton TB, Nugent, JK (1997) Escala para la evaluación del comportamiento neonatal. Barcelona: Paidós, Barcelona, Spain.
- Bayley N (1977) BSID Escalas Bayley de Desarrollo Infantil: manual. TEA Ediciones (ed.). Fundación Dialnet, Calle Barriocepo, Spain.
- Amiel-Tison C (2002) Update of the Amiel-Tison neurologic assessment for the term neonate or at 40 weeks corrected age. Pediatr Neurol 27: 196-212.
- Barrera ME, Rosenbaum PL, Cunningham CE (1986) Early home intervention with low-birth-weight infants and their parents. Child Dev 57: 20-33.
- Shonkoff JP, Hauser-Cram P (1987) Early intervention for disabled infants and their families: A quantitative analysis. Pediatrics 80: 650-658.
- Girolametto L (1988) Improving the social conversation skills of developmentally delayed children: an Intervention study. J Speech Hear Disord 53: 156-167.
- Tallal P, Gaab N (2006) Dynamic auditory processing, musical experience and language development. TRENDS in Neurosciences 29: 382-390..
- Hoff E, Naigles L (2002) How children use input to acquire a lexicon. Child Dev 73: 418-433.
- Hurtado N, Marchman VA, Fernald A (2008) Does input influence uptake? Links between maternal talk, processing speed and vocabulary size in Spanish-learning children. Dev Sci 11: 31-39.
- Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F (2003) Less is more: meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull 129: 195-215.
- Cheour M, Ceponiene R, Lehtokoski A, Luuk A, Allik J, et al. (1998) Development of language-specific phoneme representations in the infant brain. Nature Neuroscience 1: 351-353.
- Butler D (1998) Babies Need Books: Sharing the Joy of Books with Children from Birth to Six. Heinemann, Portsmouth, UK.
- Raikes H, Pan BA, Luze G, Tamis-LeMonda CS, Brooks-Gunn J, et al. (2006) Mother-child bookreading in low-income families: correlates and outcomes during the first three years of life. Child Dev 77: 924-953.
- Girolametto L, Weitzman E, Wiigs M, Pearce P (1999) The relationship between maternal language measures and language development in toddlers with expressive vocabulary delays. American Journal of Speech Language Pathology 8: 364-374.
- Stolt S, Lehtonen L, Haataja L, Lapenleimu H (2011) The language used in early mother–child interaction by very-low-birth-weight children, with a focus on the emergence of grammar. Revista de Logopedia, Foniatría y Audiología 31.
- Ayres AJ, Mailloux Z (1981). Influence of sensory integration procedures on language development. Am J Occup Ther. 35: 383-390.
- Daniel HJ (1989) The vestibular system and language evolution. In: Wind J, Pulleyblank EG, de Grolier E, Bichakjian BH (eds.). Studies in Language Origins 1: 257.
- Dale PS, Goodman JC (2005) Commonality and individual differences in vocabulary growth. In: Tomasello M, Slobin DI (eds.). Beyond Nature-Nurture. Lawrence Erlbaum Assoc, New Jersey, USA. Pg no: 41-80.
Citation: Jackson-Maldonado D, Perez-Pereira M, Ramírez GA, Cycyk LM, Carrillo MC et al. (2017) Effects of Early Intervention on the Language of Mexican and Galician Preterm Infants. J Neonatol Clin Pediatr 4: 018.
Copyright: © 2017 Donna Jackson-Maldonado, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!

