
Effects of Kinesiology Tape on Post-stroke Patients with Complex Regional Pain Syndrome Type 1: A Randomized Control Trial
*Corresponding Author(s):
Yuling WangDepartment Of Rehabilitation Medicine, The Sixth Affiliated Hospital Of Sun Yat-sen University, Guangdong, China
Tel:+86 2038476737,
Email:wangyul@mail.sysu.edu.cn
Abstract
Objective: To determine the effect of kinesiology tape on post-stroke patients with complex regional pain syndrome type 1.
Methods: Seventeen patients with post-stroke complex regional pain syndrome type 1 were randomized to a kinesiology tape group and a control group. The control group received conventional treatment, while the kinesiology group received conventional treatment plus kinesiology tape. Pain level was evaluated as the primary outcome, and hand edema and physical function were measured as the secondary outcome. The assessments were conducted before treatment as the baseline, in mid-term of treatment (1 week intervention) and end of treatment (2 weeks intervention).
Results: The kinesiology tape group showed a significant decrease in pain (P=0.012) at both mid-term and final assessments, while the control group only showed decreased pain in the final assessment. Furthermore, the kinesiology group demonstrated increased upper limb and hand function but not in the control group. Both groups demonstrated non-significant differences in hand edema and no significant between-group differences were observed in each assessment session.
Conclusion: Adding the kinesiology tape to the standard treatment for post-stroke complex regional pain syndrome type 1 patients could decrease the pain and increase upper-limb and hand function faster than standard treatment. Kinesiology tape is a promising treatment for post-stroke patients with complex regional pain syndrome type 1.
Keywords
Complex regional pain syndrome type 1; Kinesiology tape; Post-stroke
INTRODUCTION
Complex Regional Pain Syndrome (CRPS) is a complicated, disabling problem characterized with neuropathic pain, sensory deficit, edema and vasomotor disorder. CRPS is categorized into two types. Complex Regional Pain Syndrome type 1 (CRPS-1) occurs after an injury without overt nerve injury while Type II occurs with distinct nerve injury [1]. More than 48% of post-stroke patients suffer from CRPS-1disorder, which usually develops within 2 weeks to 3 months after stroke [2]. The post-stroke CRPS-1 patients are inflicted with several annoying symptoms, including pain hyperesthesia and/or allodynia, temperature asymmetry and/or skin color change, edema, as well as decreased range of motion and trophic deficit. Since the patho-physiological mechanisms of CRPS are unclear, the treatment for post-stroke CRPS-1 has focused on relieving these symptoms, maintaining normal joint alignment and motion, and improving muscle strength. However, no conclusive evidence supports any particular approach [3].
Kinesiology Tape (KT) was popularized by Kenzo Kaze in the 1970s. When fixing it onto the skin, KT is thought to increase local circulation, reduce further local edema, and may provide a positional stimulus to the skin for proper afferent input to the central nervous system [4]. Increasingly, many studies have reported that KT can reduce musculoskeletal pain, increase range of motion and strength. For example, in patients with knee osteoarthritis, a KT group exhibited greater pain reduction, less joint stiffness and functional improvement after 3 consecutive days of KT application [5]. Moreover, KT reduced hand edema in acute stroke patients [6], improved shoulder range of motion and reduced hemiplegic pain [7]. Specifically, Huang et al., reported that a 3-week KT plus standard therapy program reduced shoulder pain as well as improved shoulder range of motion and function [8].
However, for the study on hemiplegic shoulder pain, it didn’t classify pain into specific type unlike the hemiplegic pain, which can be classified into nociceptive, peripheral or central neuropathic pain or a combination of both the nociceptive and neuropathic pain [9]. The effect of KT on post-stroke CRPS-1 neuropathic pain, which is the common cause of pain and disability of upper extremity, still remains unknown.
Therefore, the aim of this study was to investigate the effectiveness of adding KT to physical therapy on post-stroke CRPS-I patients. We recruited post-stroke patients diagnosed with CRPS-1 and randomized the patients to the KT group and the control group. The patients in the KT group received standard conventional therapy plus KT while the control group received standard conventional therapy alone. We hypothesized that adding KT to conventional therapy for post-stroke CRPS-I would significantly decrease pain, increase shoulder range of motion, decrease hand edema and improve upper limb sensorimotor performance more than conventional therapy alone.
METHODS
Study design
This study was a single blind, randomized controlled clinical trial approved by the institutional Ethics Review Board of the Sixth Affiliated Hospital of Sun Yat-sen University, Guangzhou, China. Stroke patients less than 6 months after stroke diagnosis suffering from CRPS-1 were randomly allocated to one of the two groups (the KT group or the conventional rehabilitation comparison group). A computer-generated scheme was conducted by an investigator who was not involved in the recruitment or treatment. On the first day of the treatment, the treating physiotherapist opened an envelope to identify the allocation and another physiotherapist not involved in the therapy would assess the clinical outcomes at baseline, the end of the 1st week and the end of the 2nd week intervention.
Participants
Post-stroke patients diagnosed with CRPS-1 were recruited over a 36-month period from inpatient of the Sixth Affiliated Hospital of Sun Yat-sen University and the Second Affiliated Hospital of Guangzhou Medical University in Guangzhou, China. The inclusion criteria were (1) diagnosed with first-time stroke within the previous 6 months [10], (2) clinical symptoms conforming to the Budapest criteria of CRPS and pain in the shoulder [11], (3) agreed to participate in the experiment and (4) Mini Mental State Examination (MMSE)>24. The participant exclusion criteria were (1) CRPS-1 caused by cerebral tumor, or trauma; (2) pain or restricted movement of the shoulder joint caused by fracture or brachial plexus injury; (3) significant orthopedic or pain conditions such as fracture, peripheral neuropathy; (4) severe heart, liver or kidney disease, cognitive dysfunction, aphasia, or mental disorder; (5) fragile skin deemed at risk for tearing with tape application, and (6) allergies to tape adhesive.
Interventions
Twenty-three patients were enrolled in the study. Half of the sample (n=12) was randomly assigned to the control group (conventional standard intervention), and the others (n=11) were randomly assigned to the intervention group (conventional standard intervention plus KT). Seventeen participants completed the intervention and assessments. See Figure 1 for the flow chart of the study.
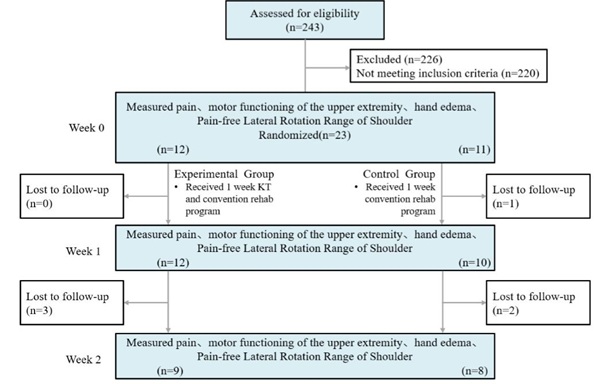
Figure 1: Study flow chart.
Outcome measures: Visual Analogue Scale (VAS); Hand Volumeter Measurement; Fugl-Meyer Assessment (FMA, upper limb portion); Pain-free Lateral Rotation Range of Shoulder.
The intervention group received both the same standard conventional physical therapy service and KT. THERABAND Kinesiology tape (THERABAND XACT STRETCH Kinesiology tape, Akron, Ohio) was used in the study with a width of 5cm and thickness of 0.5 mm. The KT was applied in a sitting position with the arm in adduction. An I-strip was placed at 75% tension over the humeral head crossing the line of shoulder joint. Another I-strip was placed above the acromion with 50% tension transversely and immediately above the acromioclavicular joint. There was no tension applied at the end of the tapes (Figures 2A and 2B). The KT application on the hand followed a dorsal and volar method suggested by Kase [4]. The subject’s wrist was passively moved into a maximum flexed position and the tape was applied to the dorsal surface of the affected hand with no stretch. The wrist was then extended to the end range passively and the tape was applied to the volar surface with no stretch tension. The tape was applied covering up to two-thirds the length of the forearm. The fan-shaped tape then crossed along the longitudinal axis of the fingers with no tension (Figures 2C and 2D). The participants in the KT group were told to leave the tape on for 5 consecutive days, and then the therapist removed the tape and checked the integrity of the skin. The experiment was stopped if any rash or allergy on the skin was observed. After 5days of KT application, the tape was removed for 2 days before the next taping session. The participants in the KT group received 5 days of tape application a week, for two weeks.All the participants received standard conventional physical therapy including active and passive range of motion, spasticity management, motor relearning, weight bearing exercise of the upper extremities, functional reach, grasp, hold and release activities, activities of daily living. However, modalities to reduce edema and pain (e.g. cold application, compression, transcutaneous electrical nerve stimulation and neuromuscular electrical stimulation) were excluded for both groups. Each participant received conventional physical therapy service for 30 minutes a day, 5 days a week for 2 weeks.
 Figure 2: Application of kinesiology tape on shoulder and hand.
Figure 2: Application of kinesiology tape on shoulder and hand.
Outcome measurements
Outcome measurements were conducted by an assessor blinded for three times, at the baseline, after the 1st week of treatment and at the end of the 2nd week treatment. The primary outcome was the level of pain. A 10cm Visual Analog Scale (VAS) was used to measure the pain at the rest position with ‘0’ at one end representing no pain and ‘10’at the other end representing most extreme pain imaginable. The VAS has been shown to be reliable and satisfactory for the measurement of pain [12].
The secondary outcomes were the values of hand swelling, motor function of the upper extremity, and shoulder pain-free lateral rotation range. Swelling was assessed by the hand volumeter which is based on the principle of water displacement. All the participants were tested in sitting position. Measurement involved immersion of the hand in the water-filled volumeter until the top of the water level reaches the transverse crease of the wrist. Water temperature ranged from 20 to 30°C. Water was displaced from the volumeter into a measuring cylinder to indicate the volume of the hand [13].The pain-free lateral rotation range of the shoulder was assessed using a universal goniometer. The assessment was done in supine position [14]. Finally, motor function of the upper extremity was assessed using the Fugl-Meyer Assessment (FMA) for the upper extremity. The FMA is a stroke-specific, performance-based impairment index with the maximum score for the upper extremity motor domain being at 66. The interrater reliability of the FMA has been reported, with the intraclass correlation coefficient at 0.92 [15]. The assessor had 5 years working experience as a physical therapy. He was knowledgeable and skilled in using the assessing techniques.
STATISTICAL ANALYSIS
SPSS software v.21.0 (IBM Corp., Armonk, NY, USA) was used to analyze the data. Both the primary and secondary outcome analyses were performed with Intention-To-Treat (ITT). test was used to compare the group differences at baseline data (gender, stroke subtypes, educational level, etc). Wilcox on signed-rank test was used to measure the difference within groups (pretreatment, one-week post-treatment, and two-week post-treatment), with the Bonfferni correction, significant criteria was set as P<0.017. Mann-Whitney U test was used to compare the differences between groups with the significance set at P<0.05.
RESULTS
Participants
Two hundred and forty-three post-stroke patients were screened for eligibility from September 2014 to October 2017. Twenty-three patients met the inclusion criteria. Six subjects did not complete the study, including three from the experimented group because of skin allergy and three from the control group because of personal reasons. Seventeen participants completed the whole 2-week trial. No significant differences were observed in the demographic data or clinical characteristics between the groups (P>0.05), as showed in (Table 1).
|
Variable |
KT Group (n=9) |
Control Group (n=8) |
|
Age, mean (SD), y |
66.5(12.0) |
60.9(9.3) |
|
Sex |
|
|
|
Male |
5(56) |
6(75) |
|
Female |
4(44) |
2(25) |
|
Onset since stroke days |
77 |
94 |
|
Educational Level |
|
|
|
Illiteracy |
1(11) |
1(12.5) |
|
Graduated from primary school |
3(33) |
2(25) |
|
Graduated from junior school |
2(22) |
3(37.5) |
|
Graduated from high school |
0(0) |
0(0) |
|
Graduated from college |
3(33) |
2(25) |
|
Post-stroke hand function impair severity (Fugl-Meyer assessment) |
|
|
|
Mild |
1(11) |
2(25) |
|
Moderate |
2(22) |
2(25) |
|
Severe |
4(44) |
1(12.5) |
|
Very Severe |
2(22) |
3(37.5) |
|
Stroke subtype |
|
|
|
Hemorrhage |
1(11) |
2(25) |
|
Infarction |
8(89) |
6(75) |
|
Frequency of taking analgesic |
|
|
|
A few times |
9(100) |
8(100) |
|
Frequently |
0 |
0 |
|
Always |
0 |
0 |
Table 1: Baseline demographic and clinical characteristic of post-stroke CRPS-1 patients in the KT and Control Group.
Notes: Data are n(%) unless otherwise indicated,
a. Post-stroke hand Function Impairment Severity (FMA), very severe, FMA score 0-11; severe, FMA score 12-22; moderate, FMA score 23-32; mild, FMA score 33+.
b. Definition of the frequency of taking analgesic?a few times, 1/1year, frequently, 1/1month, always, >1/week
c. Definition of the frequency of taking diuretic medicine?a few times, 1/1year, frequently, 1/1month, always, >1/week
Effect of intervention on pain
After 1-week of treatment, VAS score (4.32±1.86) decreased significantly in the KT group compared to the baseline (6.36±2.26) assessment (P=0.012) while there was no significant difference observed in the control group (P=0.027), see Table 2. However, both groups demonstrated a non-significant difference of the VAS score between the 1st week assessment and the 2nd week assessment (P=0.122 for KT group and P=0.061 for the control group). Similarly, both groups demonstrated significant decrease of the VAS score at the end of the 2nd week of treatment when compared to the baseline assessment (P=0.012 for KT group and P=0.012 for the control group). Between-group comparisons demonstrated no significant difference in each assessment (P=0.541 for the baseline comparison, P=0.606 for 1st week comparison and P= 0.423 for 2nd week comparison).
Effect of intervention on hand edema
Both groups had non-significant differences between the baseline assessment and the 1st week assessment (P=0.122 for KT group and P=0.061 for the control group). The same is also true between the baseline and the 2nd week assessment results (P=0.686 for KT group and P=0.109 for the control group). Between-group comparisons demonstrated no significant difference in each assessment (P=0.250 for the baseline comparison, P=0.571 for 1st week comparison and P=0.571 for 2nd week comparison).
Effect of intervention on range of shoulder pain-free lateral rotation
Both groups showed non-significant difference between the baseline assessment and the 1st week assessment results (P=0.401 for KT group and P=0.018 for the control group), although the control group approached significance. However, the KT group demonstrated a significant increase in pain-free lateral rotation in the 2nd week assessment compared to the 1st week assessment (P=0.012), while there was no significant difference observed in the control group (P=0.018). Both groups showed significant increase in the degree of the shoulder pain-free lateral rotation in the 2nd week assessment compared to the baseline assessment (P=0.015 for KT group and P=0.012 for the control group). For the between-group comparison, there was no significant difference in each assessment (P=0.423 for the baseline comparison, P=0.606 for 1st week comparison and P=0.541 for 2nd week comparison).
Effect of intervention on upper-extremity function
The KT group demonstrated significant increase in the Fugl-Meyer score in both the 1st week assessment (P=0.011) and the 2nd week assessment (P=0.008) compared to the baseline assessment results. The control group demonstrated a non-significant increase in the Fugl-Meyer score in both the 1st week assessment (P=0.109) and the 2nd week assessment (P=0.018) compared to the baseline assessment results, although it approached significance. Similarly, the between-group comparison demonstrated no significant difference in each assessment (P=0.743 for the baseline comparison, P=0.963 for 1st week comparison and P=0.815 for 2nd week comparison).
|
Variables |
KT group |
Control group |
||||||||||
|
Baseline |
T1 |
T2 |
P0 |
P1 |
P2 |
Baseline |
T1 |
T2 |
P0 |
P1 |
P2 |
|
|
VAS |
6.36(2.26) |
4.32(1.86) |
3.50(1.49) |
0.012 |
0.122 |
0.012 |
6.06(1.23) |
4.88(1.57) |
4.31(1.41) |
0.027 |
0.061 |
0.012 |
|
Volume |
348.47(32.74) |
357.13(28.72) |
359.33(43.52) |
0.686 |
0.5 |
0.686 |
377.39(13.62) |
370.57(15.03) |
366.10(13.47) |
0.109 |
0.109 |
0.109 |
|
External rotation |
29.41(19.85) |
31.67(14.03) |
40.89(16.88) |
0.401 |
0.012 |
0.015 |
21.25(16.18) |
28.21(10.74) |
34.83(8.90) |
0.018 |
0.018 |
0.012 |
|
Fugl-Meyer |
19.00(11.42) |
25.44(13.31) |
28.67(13.83) |
0.011 |
0.011 |
0.008 |
22.13(16.04) |
25.50(17.16) |
30.63(19.43) |
0.109 |
0.018 |
0.018 |
Table 2: Clinical features of participants at Baseline, 1st week after intervention and 2nd week after intervention in the KT and control group.
Notes: Values are mean (SD).
P0: P values were calculated with Wilcoxon signed-rank test, compared between the baseline assessment and 1st week assessment.
P1: P values were calculated with Wilcoxon signed-rank test, compared between the 1st week assessment and 2nd week assessment.
P2: P values were calculated with Wilcoxon signed-rank test, compared between the baseline assessment and 2nd week assessment.
?: P<0.05
DISCUSSION
In this study, adding KT to standard conventional physical therapy reduced pain and improved upper limb and hand function. Furthermore, the improvement of function and decreased pain level were acquired faster in the KT group. In addition, shoulder pain-free lateral rotation range significantly increased, however, the hand edema did not decrease significantly with the addition of KT. In fact, the problem of edema was found reduced in the KT group but increased in the physical therapy only.
The short-term effect of the KT on pain was above the minimum of the clinically worthwhile effect of 2cm [16], in addition, the upper extremity function also improved. The overall results in this study are similar to previous findings. Huang et al. applied a 3-week intervention for patients with hemiplegic pain and found the experimented group experienced greater reduction in pain and with a better score in the Disability Index [8]. Another study found 3-weeks of therapeutic KT being added to conventional therapy limited the occurrence of hemiplegic shoulder pain and improved shoulder flexion in sub-acute stroke patients with a flaccid shoulder joint [17]. As hemiplegic pain can be either nociceptive, peripheral or central neuropathic pain, or a combination of both nociceptive and neuropathic pain [9], our study contributes evidence to the effectiveness of KT on neuropathic pain of post-stroke CRPS-1.
The possible mechanism of the pain relief in CRPS-1 post-stroke patients after KT is likely neurological. In CRPS, the peripheral sensitization of afferent C fibers can trigger increased excitability and synaptic efficacy of the neurons in the central nervous system. KT might stimulate the neuromuscular pathway through increased afferent feedback. According to the Gate Control Theory, the mechanical stimuli induced by KT would occupy the afferent stimulus to the larger-diameter nerve fibers, which can then serve to mitigate the inputs received from the smaller-diameter nerve fibers conducting nociception [18]. Another possible explanation for the pain relief effects of KT can be related to the afferent information that is sent from the neural and movement feedbacks of the participants, which can eliminate the so-called neglect-like phenomenon [19] and the abnormal postures [20]. A study by Bae et al. found that when KT was applied to patients suffering chronic low back pain, it not only reduced pain but positively affected their postural control and Movement-Related Cortical Potential (MRCP) [21]. KT may first have an effect on the supra spinal system and it may intervene the cortical level. Therefore, KT may help to re-organize the sensory feedback and motor outputs. However, the mechanism of KT on post-stroke CRPS-1 required further study.
At both the mid-term and final assessments after taping, there were no significant differences in edema. The results were different from a study conducted by Aguilarferrandiz et.al [22]. Their results showed that, after an application of KT3 times/week for 4 weeks, a significant reduction of edema occurred in post-menopausal women with chronic venous insufficiency [22]. The possible explanation for the difference between these two studies may be simply due to the difference between the nature of the pathological swelling. In Aguilarferrandiz et.al’s study, the extracellular fluid in patients with chronic venous insufficiency [22] is usually a consequence of changes in the hydrostatic pressure and the level of proteins [23]. In contrast, the edema in post-stroke CRPS-1 is usually developed after tissue injury. As a response to tissue damage, various inflammatory cells and other exudates migrate to the injury site and release inflammatory mediators. Hence, the CRPS-1 swelling contents likely contain a higher level of protein substances [24]. The effect of KT on edema may be related to the effect of exu-date drainage and it does not change capillary permeability. Thus, the edema that occurs in Post-stroke CRPS-1 patients with higher concentration of protein in the edema may not benefit from KT [25].
Another possibility of the contrasting results in edema could be due to the different measurement methods for the swelling. Aguilarferrandiz et al., used bio-impedance to assess the swelling, which measures at a cellular level. Our study used “volume” to measure the swelling. In fact, Aguilarferrandiz et al., also measured the “volume” for KT intervention in their post-menopausal subjects with chronic venous insufficiency. They applied a 4 weeks period of KT on the subjects’ medial and lateral gastrocnemious muscle. They found no significant decrease in edema [26].
Three out of the twelve participants experienced the problem of skin allergy during application in this study while few previous studies reported similar problems. Mikotajewska [27] reported a case of skin allergy during KT application, the author hypothesized that the allergy may be related to the substances used when tape is prepared and manufactured to eliminate the possibility of skin preparation substance allergy, we used clean water to prepare the skin and it was then dried with care. We found the outcome was encouraging. However, still 25% of the participants in the experiment group experienced a skin allergy, possibly due to the humid weather in southern China where the yearly average humidity level is up to 77%. Further studies are needed to address the skin allergy issue in post-stroke CRPS-1 patient.
The limitations of this research were that there was an absence of a group with no intervention given and there was no placebo group. If these were present in the design, more conclusive information may be available and brought forward. However, due to ethical consideration, no intervention for the control group could not be possible. In our study, we excluded the treatments that may carry medical effects to reduce pain and edema to address this limitation. The sample size in this study was also small and a larger population needed to be studied in the future. Furthermore, the majority of stroke patients recruited in this study were ischemic, it should be cautious to generalize these results to other types of stroke.
CONCLUSION
In conclusion, this study suggested that patients with post-stroke CRPS-1 benefit from the application of KT regarding pain range of shoulder pain-free lateral rotation and upper extremity function. KT can play a role as an adjunct treatment modality in a multi-modal approach to CRPS type 1 management after stroke. To our best knowledge, this is the first study on the application of KT for the treatment of post -stroke CRPS-1 patient. Further study with a larger sample size is recommended to further examine the clinical effects of KT for people suffering from post-stroke CRPS-1. Given the fact that the application of KT is a comfortable, time-saving and labor-saving treatment, it can be a promising adjunct treatment modality for post-stroke CRPS-1 patients. However, more research is warranted.
ACKNOWLEDGEMENT
The study was funded by grants from Guangzhou Major Industrial Technology Project of Guangzhou Science, Technology and Innovation Commission of China (No. 201802010039), Performance Health Academy of American (TB2014-3). We thank with great appreciation to all the participants for willingly and voluntarily joining in the trial, completing their questionnaires and attending all therapy sessions. We take the pride of thanking those staff who has given us their unfailing supports in the study design, statistical analysis and manuscript preparation (Beibei Feng, Xiaoxia Zhu, Yangyang Lin). We also extend our warmest acknowledgment to all those staff at all the centers for recruiting, motivating and treating our participants (Yisheng Chen, Weiming Wang).
CONFLICT OF INTEREST
The KT used in this study was supplied by Performance Health. We declare there are no competing and conflicting interests with our study.
REFERENCES
- Goh EL, Chidambaram S, Ma D (2017) Complex regional pain syndrome: a recent update. Burns Trauma 5: 2.
- Kocabas H, Levendoglu F, Ozerbil OM, Yuruten B (2007) Complex regional pain syndrome in stroke patients. Int J Rehabil Res 30: 33-38.
- O'Connell NE, Wand BM, McAuley J, Marston L, Moseley GL (2013) Interventions for treating pain and disability in adults with complex regional pain syndrome. Cochrane Database Syst Rev 30: CD009416.
- Kase K (2003) Clinical therapeutic applications of the Kinesio taping methods (2nd edn), Kinesio Taping Assoc Pg no: 249.
- Rahlf AL, Braumann KM, Zech A (2019) Kinesio Taping Improves Perceptions of Pain and Function of Patients With Knee Osteoarthritis: A Randomized, Controlled Trial. J Sport Rehabil 28: 481-487.
- Bell A, Muller M (2013) Effects of kinesio tape to reduce hand edema in acute stroke. Top Stroke Rehabil 20: 283-288.
- Chatterjee S, Hayner KA, Arumugam N, Goyal M, Midha D, et al. (2016) The California Tri-pull Taping Method in the Treatment of Shoulder Subluxation After Stroke: A Randomized Clinical Trial. N Am J Med Sci 8: 175-182.
- Huang YC, Chang KH, Liou TH, Cheng CW, Lin LF, et al. (2017) Effects of Kinesio taping for stroke patients with hemiplegic shoulder pain: A double-blind, randomized, placebo-controlled study. J Rehabil Med 49: 208-215.
- Kalichman L, Ratmansky M (2011) Underlying pathology and associated factors of hemiplegic shoulder pain. Am J Phys Med Rehabil 90: 768-780.
- Cacchio A, De Blasis E, De Blasis V, Santilli V, Spacca G (2009) Mirror therapy in complex regional pain syndrome type 1 of the upper limb in stroke patients. Neurorehabil Neural Repair 23: 792-799.
- Harden RN, Bruehl S, Perez RS, Birklein F, Marinus J, et al. (2010) Validation of proposed diagnostic criteria (the "Budapest Criteria") for Complex Regional Pain Syndrome. Pain 150: 268-274.
- Huskisson EC (1974) Measurement of pain. Lancet 2: 1127-1131.
- Boland R, Adams R (1996) Development and evaluation of a precision forearm and hand volumeter and measuring cylinder. J Hand Ther 9: 349-358.
- MacDermid JC, Chesworth BM, Patterson S, Roth JH (1999) Intratester and intertester reliability of goniometric measurement of passive lateral shoulder rotation. J Hand Ther 12: 187-192.
- Sanford J, Moreland J, Swanson LR, Stratford PW, Gowland C (1993) Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. Phys Ther 73: 447-454.
- Hagg O, Fritzell P, Nordwall A (2003) The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J 12: 12-20.
- Huang YC, Leong CP, Wang L, Wang LY, Yang YC, et al. (2016) Effect of kinesiology taping on hemiplegic shoulder pain and functional outcomes in subacute stroke patients: a randomized controlled study. Eur J Phys Rehabil Med 52: 774-781.
- Kneeshaw D (2002) Shoulder taping in the clinical setting. Journal of Bodywork and Movement Therapies 6: 2-8.
- Galer BS, Jensen M (1999) Neglect-like symptoms in complex regional pain syndrome: Results of a self-administered survey. J Pain Symptom Manage 18: 213-217.
- Bank PJ, Peper CL, Marinus J, Beek PJ, van Hilten JJ (2013) Deficient muscle activation in patients with Complex Regional Pain Syndrome and abnormal hand postures: An electromyographic evaluation. Clin Neurophysiol 124: 2025-2035.
- Bae SH, Lee JH, Oh KA, Kim KY (2013) The effects of kinesio taping on potential in chronic low back pain patients anticipatory postural control and cerebral cortex. J Phys Ther Sci 25: 1367-1371.
- Aguilar-Ferrándiz ME, Castro-Sánchez AM, Matarán-Peñarrocha GA, Guisado-Barrilao R, García-Ríos MC, et al. (2014) A randomized controlled trial of a mixed Kinesio taping-compression technique on venous symptoms, pain, peripheral venous flow, clinical severity and overall health status in postmenopausal women with chronic venous insufficiency. Clin Rehabil 28: 69-81.
- Labropoulos N, Giannoukas AD, Nicolaides AN, Veller M, Leon M, et al. (1996) The role of venous reflux and calf muscle pump function in nonthrombotic chronic venous insufficiency. Correlation with severity of signs and symptoms. Arch Surg 131: 403-406.
- Ludwig J, Baron R (2004) Complex regional pain syndrome: An inflammatory pain condition? Drug Discovery Today: Disease Mechanisms 1: 449-455.
- Lund T, Onarheim H, Reed RK (1992) Pathogenesis of edema formation in burn injuries. World J Sur 16: 2-9.
- Aguilar-Ferrándiz ME, Castro-Sánchez AM, Matarán-Peñarrocha GA, García-Muro F, Serge T, et al. (2013) Effects of kinesio taping on venous symptoms, bioelectrical activity of the gastrocnemius muscle, range of ankle motion, and quality of life in postmenopausal women with chronic venous insufficiency: A randomized controlled trial. Arch Phys Med Rehabil 94: 2315-2328.
- Miko?ajewska E (2010) Allergy in patients treated with kinesiology taping: A case report. Medical Rehabilitation 14: 29-32.
Citation: Li X, Zhou T, Zou Z, Ye Z, Page P, et al. (2020) Effects of Kinesiology Tape on Post-stroke Patients with Complex Regional Pain Syndrome Type 1: A Randomized Control Trial. J Phys Med Rehabil Disabil 6: 040.
Copyright: © 2020 Xian Li, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

