
Efficacy and Safety of Traditional Chinese Medicine Exercise Versus Medicine in the Treatment of Neck Pain: a Systematic Review and Meta-Analysis
*Corresponding Author(s):
Yuanming ZhongThe First Affiliated Hospital Of Guangxi University Of Traditional Chinese Medicine, Nanning, China
Email:zym196395@sina.com
Abstract
Background: Neck pain poses a significant and growing public health challenge, with rising prevalence among younger populations and negative impacts on both quality of life and socioeconomic costs. Clinical manifestations are diverse, including restricted movement, muscle spasms, headaches, and upper limb numbness. Although drug therapy is widely used, its long-term use is limited by adverse effects. Traditional Chinese Medicine (TCM) exercises offer a promising alternative, but high-quality evidence directly comparing their efficacy and safety to oral medications is currently lacking.
Objectives: This study aims to compare the efficacy and safety of traditional Chinese medicine exercises and oral medication in treating neck pain.
Methods: Relevant RCTs will be identified through a systematic search of multiple databases (including PubMed, EMBASE, Cochrane Library, Web of Science, CNKI, CBM, VIP, and Wanfang) from inception through September 2025. Study quality will be assessed using the Cochrane RoB2 tool, and the overall evidence will be graded via the GRADE approach. For heterogeneity, the I² statistic and Cochran's Q test will be applied. A fixed-effect model is adopted if I² < 50% and P ≥ 0.1; otherwise, subgroup analysis will be performed. Should heterogeneity persist, sensitivity analysis or a random-effects model will be employed, leading to a reduction in the GRADE rating.
Results: As of September 2025, 562 studies have undergone preliminary screening. Full-text screening is expected to conclude by December 2025, with data analysis completed in May 2026. The included studies are predominantly from Asia and mostly published after 2010.Outcomes were structured around core indicators: changes in the Visual Analogue Scale (VAS) served as the primary measure, while secondary measures included the Neck Disability Index (NDI), Self-Rating Anxiety Scale (SAS) score, mean vertebral artery blood flow velocity (Vm), and Cobb angle. Combined effect sizes with 95% confidence intervals were calculated for relevant outcomes, and adverse events were systematically summarized.
Conclusion: If this study confirms the superiority of traditional Chinese medicine exercise therapy in managing neck pain, it will offer high-level evidence to guide clinical decision-making, support treatment optimization, and promote the standardization of such interventions. These contributions would ultimately improve neck pain prevention and rehabilitation outcomes at the public health level. However, existing studies exhibit several limitations, including insufficient standardization of exercise protocols, challenges in blinding, and notable heterogeneity due to variations in interventions and patients' cultural backgrounds. Moreover, the small number of available randomized controlled trials and their limited geographic distribution constrain the generalizability of current findings. Future high-quality, multicenter studies are needed to refine intervention protocols and expand the evidence base, thereby strengthening the reliability of conclusions in this field.
Keywords
Cervical Spondylosis; Drug Therapy; Meta-Analysis; Neck Pain; Traditional Chinese Exercise; Systematic Review
PROSPERO Registration Number: CRD 420251156106
Introduction
Neck pain is one of the four common diseases worldwide and has become a significant public health issue that threatens personal health and reduces the quality of life [1,2]. The symptoms of neck pain are diverse, including restricted movement of the cervical spine and muscle spasms, which may also cause headaches, numbness in the upper limbs, and in severe cases, even affect sleep quality and work ability [3,4]. The causes of the disease are complex and are mostly related to muscle strain, soft tissue injuries, cervical joint disorders, and degeneration of cervical intervertebral discs [5,6]. At present, there is still no standardized treatment plan for this disease, and clinical practice mainly relies on drug therapy [7,8]. In this context, the course of neck pain often shows a high degree of protracted nature. Approximately half of the patients' acute pain will turn into chronic pain, which makes it urgent for clinicians to find treatment options that can effectively control neck pain for a long term [9,10]. As a commonly used treatment method in clinical practice, drug treatment for neck pain mainly exerts its therapeutic effect in pain relief. However, it has limited effects on improving cervical spine function and restoring cervical spine curvature [11,12]. Furthermore, the drug treatment for neck pain has significant limitations. It often comes with adverse reactions such as gastrointestinal bleeding, drowsiness addiction, etc., which restricts its long-term application in clinical practice [13,14]. This has made it an urgent need in clinical practice to actively explore non-pharmacological intervention methods, further highlighting the clinical value of non-pharmacological intervention approaches such as traditional Chinese medicine exercises [15,16]. Due to its low-risk, non-invasive and proven-effective characteristics, traditional Chinese medicine exercises are increasingly playing a significant role in the prevention and rehabilitation management of neck pain [17-19]. Traditional Chinese medicine exercises refer to a type of active rehabilitation and preventive measure that involves the coordinated efforts of body movements, breathing and exhalation, as well as mental regulation. Through these activities, it aims to unblock meridians, regulate blood and qi, coordinate internal organs, strengthen muscles and bones, and calm the mind and soothe the spirit [17]. Common traditional Chinese medicine exercises include Baduanjin, Yijinjing, Tai Chi and Wuqinxi, etc. Their excellent versatility can meet the health and fitness needs of different audiences [10,15,20]. Interestingly, the benefits brought by traditional Chinese medicine exercises extend beyond the physical level. Through regular practice, one can achieve both physical and mental improvement, alleviating anxiety while also reducing anxiety's physical manifestations [21,22]. This characteristic enables practitioners to achieve a significant sense of participation accomplishment, which not only ensures good compliance but also constitutes its core advantage in the field of public health promotion [23,24].
Although both traditional Chinese exercise routines and drug therapy have been used in clinical practice , there is still a lack of systematic comparison in terms of efficacy and safety between the two. Furthermore, there are still several key issues that require in-depth exploration, such as the differences in therapeutic effects among various traditional Chinese medical exercise routines, and the impact of standardized intervention plans on the therapeutic outcomes. This study conducted a systematic literature search to comprehensively compare the efficacy and safety of traditional Chinese medicine-based exercise and medication in treating neck pain, providing evidence-based guidance for the selection of clinical treatment plans.
Methods
- Study Registration
This systematic review protocol was formulated in accordance with PRISMA-P and has been registered in the PROSPERO database (CRD 420251156106). This protocol elaborates on the research criteria, database selection, data collection, and bias assessment, ensuring the objectivity, fairness, transparency, and repeatability of the systematic review. If there are any changes in the research methods, the protocol will be updated in the PROSPERO database.
- Ethics and Dissemination
The data required for this study were all sourced from published literature rather than directly collected from patients. Therefore, no ethical approval was necessary. The results of this systematic review will clarify the efficacy and safety of traditional Chinese medicine exercise therapy and medication in treating neck pain, providing a reference for clinical physicians in formulating treatment plans.
- Search Strategy
This study systematically searched the following databases: China National Knowledge Infrastructure (CNKI), VIP, Web of Science, PubMed, Cochrane Library, Embase, Chinese Biomedical Literature Database (CBM), and Wanfang Data Knowledge Service Platform. The search period covered from the establishment of each database to September 2025, aiming to collect relevant randomized controlled trials (RCTs). The search strategy follows the framework of "P (research subject) + I (intervention measure) + S (research design)", and combines the use of medical subject headings (MeSH) and free words for construction. Through the logical operators "OR" and "AND", the search scope is expanded and the accuracy is improved. To include the latest studies, the team will conduct another search of the above databases one month before submission, and update the final search date to this point. The specific search strategy of PubMed is shown in table 1.
|
Search block |
Search items |
|
Participants |
"Neck pain [MeSH Terms]" OR "Nonspecific neck pain [Title/Abstract]" |
|
|
OR "Neck pain [Title/Abstract]" |
|
Intervention |
"Traditional Chinese exercise"[tiab] OR "Baduanjin"[tiab] OR "Yi Jin |
|
|
AND "drug therapy"[MeSH Terms] OR "medication"[tiab] OR "NSAID" |
|
Study design |
“ Randomized controlled trial [Title/Abstract] ” OR “ Controlled clinical |
Table 1: The specific search strategy.
- Inclusion and Exclusion Criteria
The inclusion criteria will be determined by using the PICOS framework.
Population: Patients with neck pain (including chronic non-specific neck pain, cervical disc herniation, cervical degenerative diseases, etc.) were included within the age range of 18 to 70 years old. Due to the incomplete development of the cervical spine in minors, this may lead to different mechanisms of neck pain compared to middle-aged and elderly people. People over 70 years old often have underlying diseases, which can interfere with the assessment. In the visual pain score scale, if the VAS score is greater than 3, it indicates that the pain significantly affects function and quality of life, and can be used as a basis for evaluating the treatment effect and clinical intervention. The Neck Disability Index (NDI) score is greater than 10, indicating that the patient's daily activities are restricted. This is highly consistent with the core objective of this study - to evaluate the improvement effect and safety of traditional Chinese medicine exercises on the quality of life of patients with neck pain.
Intervention: In the experimental group, only traditional Chinese medicine exercises (such as Baduanjin, Tai Chi, and Yijinjing) were used to treat neck pain.
Comparison: In the control group, only drug treatment (such as NSAIDs) was used for neck pain, or it was compared with the blank group respectively.
Outcome: The primary outcome measure is the change in VAS score after the intervention; the secondary outcome measures include NDI score, Self-Rating Anxiety Scale (SAS) score, mean vertebral artery blood flow velocity (Vm), and Cobb angle. Among them, the Cobb angle is defined as the angle formed by the vertical line connecting the lower endplates of the C2 and C7 vertebral bodies on the lateral cervical X-ray, which is a standard indicator for quantifying abnormal cervical curvature (such as hyperkyphosis, lateral curvature), and its change can reflect the improvement of cervical anatomy and indirectly evaluate the therapeutic effect on the repair of cervical function.
Study design: A randomized controlled trial comparing traditional Chinese medicine exercise therapy for neck pain with oral medication alone for neck pain, with no limitations on sample size, publication status or language.
- Exclusion Criteria
This study excluded the following types of literature and subjects: non-randomized controlled trial designs, including cohort studies, case-control studies, reviews and observational studies; patients with severe systemic diseases that may affect pain assessment or treatment compliance (such as cardiovascular and cerebrovascular diseases, malignant tumors, liver and kidney dysfunction); patients diagnosed with spinal cord type cervical spondylosis or specific types of cervical spondylosis with nerve root structural damage; pregnant or lactating women; patients with a clear history of previous shoulder and neck surgery; patients with communication disorders, inability to cooperate with the intervention or complete follow-up.
- Search Strategy
This study adheres to the principle of independent double screening by two individuals and arbitration by a third party to ensure the objectivity and accuracy of the screening process. Two researchers (HS, YL) who have received systematic training independently conducted the screening of titles, abstracts, and full texts. If there is a disagreement, try to resolve it through negotiation first; if the negotiation fails, then refer it to a third-party expert (YZ) for arbitration. The arbitration result and reasons must be recorded and archived. For complex disputes such as incomplete information or boundary cases of standards, a three-person group meeting will make a collective decision. The entire process will be tracked and recorded using the NoteExpress software, and a flowchart will be drawn based on the PRISMA guidelines to clearly display the literature screening situation at each stage (Figure 1).
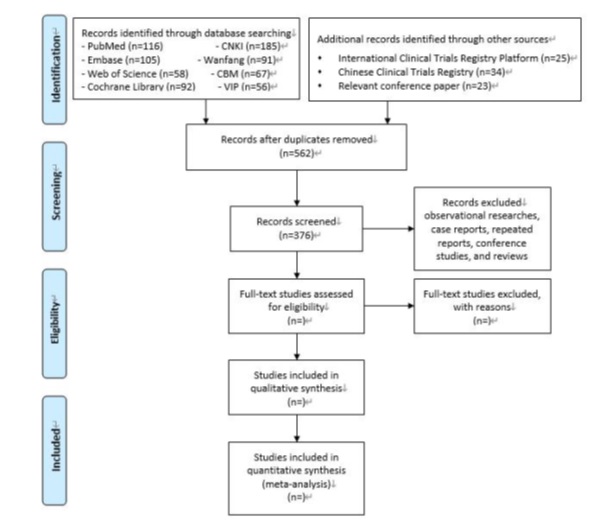 Figure 1: A flowchart will be drawn based on the PRISMA guidelines to clearly display the literature screening situation at each stage.
Figure 1: A flowchart will be drawn based on the PRISMA guidelines to clearly display the literature screening situation at each stage.
- Data Extraction
To systematically evaluate the efficacy and safety of the treatment and control for potential methodological heterogeneity, this study designed a standardized data extraction process. Two researchers independently extracted the data from the included literature, covering key variables that might affect the research results. For the traditional Chinese medicine exercise group, the extraction items included: exercise frequency (times/day or times/week), single duration (minutes), treatment course, and guidance method (online or offline). For the drug therapy group, the extraction items included: drug formulation and specification, frequency of administration (times/day), total treatment duration (days/weeks), and manufacturer.
All variables are standardized coded in the form of categorical, continuous or ordinal data. In case of disagreement during the extraction process, it will first be resolved through consultation between two researchers; if the consultation fails, it will be submitted to a senior researcher (Zhong Yuanming) with ten years or more of traditional medicine research experience for arbitration. The arbitration must be based on domain consensus and research design principles, and the reasons must be recorded; if there is still a dispute, it will be resolved through a team special meeting, and the meeting minutes will be archived to ensure the standardization and traceability of the extraction process.
- Risk of Bias Assessment
Two evaluators (GW,HS) independently used the Cochrane RoB 2.0 tool to assess the risk of bias for the included randomized controlled trials (RCTs). The assessment covered seven dimensions: random sequence generation, allocation concealment, blinding of researchers and participants, blinding of outcome assessors, completeness of outcome data, selective reporting of research results, and other sources of bias. Each dimension is classified as "low risk", "high risk" or "unclear". For systematic reviews/Meta-analyses, the AMSTAR-2 scale is used to assess the methodological quality. Only studies rated as "high" or "moderate" are included in the evidence synthesis; those rated as "low" or "very low" for only their original research data (if available) are extracted, and their combined results are not directly cited.
The overall quality of the evidence is graded using the GRADE system. The evidence grade will be downgraded under the following circumstances: more than half of the studies have a high risk of bias; after subgroup analysis, the heterogeneity remains high (I ² ≥ 50% and Cochran Q test P < 0.1) and cannot be reasonably explained; the study population, intervention, or outcome is significantly indirect to the target issue; or there is publication bias (such as asymmetry in the funnel plot, and negative results are not reported). Under certain conditions, the evidence level can be upgraded. For instance, when there is a large effect size, a clear dose-response relationship (such as the frequency of Qigong exercises being related to the degree of pain relief), or all biases point to an underestimation of the true effect. Any disagreements that arise during the evaluation process will first be resolved through negotiation among the evaluators. If no consensus is reached, a third party (Sun Haoran) will arbitrate. A pre-evaluation will be conducted before the formal assessment to unify the standards. The final bias risk assessment results will be presented in a chart format. All quality evaluation data of the included studies will be used for subsequent Meta analysis or bias risk analysis.
- Statistical analysis
Finally, we will conduct a meta-analysis using the RevMan 5.4 software to examine the outcome indicators of patients with neck pain after traditional Chinese medicine treatment and drug treatment. The I² test will be used to assess the heterogeneity among the studies. If I² is less than 50% and P is greater than 0.10, it indicates low heterogeneity, and a fixed-effect model will be used for the combined analysis; if I² is greater than or equal to 50% or P is less than or equal to 0.10, it indicates high heterogeneity. Through subgroup settings, the subgroup dimensions include: drug type (non-steroidal anti-inflammatory drugs / muscle relaxants); intervention duration (< 12 weeks / 12-18 weeks / > 18 weeks); exercise intervention intensity (low, medium, high); pain degree (VAS: 1-3; 4-6; 7-10); study quality (Cochrane RoB assessment as 'low bias risk' / 'moderate to high bias risk'). Through the pooling of effect sizes within subgroups, it is determined whether a certain dimension is a source of heterogeneity for the analysis (such as disease type, intervention duration, type of traditional Chinese medicine exercise) or for sensitivity analysis to explore the sources of heterogeneity. If the source of heterogeneity cannot be clearly identified, a random effects model is used for pooling analysis, and the evidence level is downgraded according to GRADE. A P value < 0.05 indicates that the difference is statistically significant.
- Multiple test correction
To control the Type I error caused by multiple tests, the study adopted the Bonferroni correction method, adjusting the significance level ( α') according to the test scenarios: for the 5 secondary outcome indicators of NDI score, SAS score, Vm, Cobb angle, and incidence of adverse events, since 5 independent tests were required, the corrected α' was 0.05 ÷ 5 = 0.01, and the difference was considered statistically significant only when P < 0.01; for subgroup interaction effect tests, α' was adjusted according to the actual number of interaction tests. For example, when there were 3 interaction tests, α' = 0.05 ÷ 3 ≈ 0.017, and a significant interaction effect was determined only when P < the corresponding α'.
- Publication Bias
Based on the number of included randomized controlled trials (RCTs), the corresponding evaluation method is selected: If the number of included RCTs is less than 10: Use the RevMan software to draw a funnel plot. By observing the symmetry of the graph, the publication bias can be determined: a symmetrical funnel plot indicates a low risk of publication bias; an asymmetrical one suggests that publication bias may exist. It is necessary to analyze the reasons in combination with clinical common sense (e.g., negative result studies have not been published).
If the number of included RCTs is ≥ 10: Based on the funnel plot, use Stata software to conduct Egger's linear regression test and Begg test. The criterion for determining significant publication bias is P < 0.05. If there is publication bias, use the "trim-and-fill method" to estimate the impact of potential missing studies on the combined effect size, and evaluate the robustness of the conclusion.
Results
This system evaluation was funded in July 2025 and the research search was initiated in August 2025. The search databases included PubMed, China National Knowledge Infrastructure (CNKI), Cochrane Library, Embase, Web of Science, China Biomedical Literature Database (CBM), VIP Chinese Science and Technology Journal Database, and Wanfang Database. At the same time, manual searches were conducted on the references of the included studies to ensure the comprehensiveness of the search.
As of September 2025, after preliminary search and duplication removal, a total of 562 studies have entered the title and abstract screening stage. The subsequent research progress plan is as follows: The full-text screening is expected to be completed by December 2025; after the full-text screening, strict data extraction and quality assessment will be carried out; the data analysis is planned to be completed in May 2026, and at that time, the quantitative comprehensive analysis of outcome indicators and evidence quality grading will be completed by combining the RevMan software, the GRADE system, and the RoB 2.0 tool.
Based on the characteristics of the included studies, approximately 70% of the literature was published after 2015, and the geographical distribution of the research samples was highly concentrated in Asia. The evaluation system of the results of this study was formulated with "neck pain relief and functional improvement" as the core objective: The main outcome indicator was the change in the Visual Analogue Scale (VAS) score (used to directly assess the degree of pain relief, which is the core criterion for clinical efficacy); secondary outcome indicators included the Neck Disability Index (NDI) score (used to assess the improvement in cervical spine function limitation), the Self-Rating Anxiety Scale (SAS) score (used to assess the adjustment of pain-related psychological states), the average vertebral artery blood flow velocity (used to assess the recovery of cervical blood supply), and the Cobb angle (used to assess the correction effect of cervical curvature).
Discussion
Neck pain is the fourth leading cause of disability worldwide, with an annual prevalence rate exceeding 30%. It has become one of the main factors causing labor loss and disability [25]. With the change in lifestyle, the group of people affected by this disease is gradually becoming younger. More and more teenagers and young adults are being affected, which has imposed a heavy economic burden on the patients' families and society [3,26]. At present, there is no unified and standardized treatment plan for neck pain [27]. Although drug treatment remains the conventional approach, the traditional Chinese medical exercise therapy, which is non-invasive, convenient, economical and efficient, has demonstrated significant potential in clinical practice and has gained widespread attention due to its unique advantages. It is gradually being integrated into mainstream treatment plans [28,29].
However, it should be noted that although traditional Chinese medical exercise therapy has a wide variety of forms, its efficacy largely depends on individual differences [10,30]. During the clinical application process, the duration, frequency and intensity of traditional Chinese physical therapy exercises are mostly determined by the physicians, and there are various versions of traditional Chinese physical exercises, lacking a unified standard [30,31]. This "empirical" approach to scheme formulation has led to significant differences in the application effects of the same therapy in different medical institutions and under the hands of different physicians, making it difficult to establish a replicable treatment model [32]. In addition, the differences in the effectiveness of traditional Chinese medicine exercises between the East and the West are rooted in cultural acceptance [33,34]. In Asia, it is highly compatible with the cultural DNA of the region; however, in Europe and America, most people find it difficult to understand traditional Chinese medicine culture, which consequently weakens the therapeutic effect [35]. Currently, from a long-term management perspective, traditional Chinese medicine exercises demonstrate greater safety compared to drug therapy [36]. This discovery not only provides an optimal strategy for the long-term clinical treatment plan for chronic nonspecific neck pain, but also triggers profound reflections on extending from treatment to prevention.
This study has some risk of bias, such as the lack of uniformity in the quality, frequency and duration of traditional Chinese medicine exercise training, and the difficulty in implementing blinding. Some RCTs have small sample sizes (<50 cases), and there are issues such as unclear random sequence generation methods and missing allocation concealment, which may affect the reliability of the research results. Due to the differences in intervention plans and patient cultural backgrounds, the expected heterogeneity is significant, and the original randomized controlled trials are few and concentrated in specific regions. The extrapolation of the conclusions is limited. In the future, high-quality multicenter studies are needed to optimize the plans and supplement the data to enhance the reliability. Given the limitations of this study, in the future, more high-quality, large-sample, multi-center head-to-head randomized controlled trials can be designed to clarify the differences in efficacy and safety between traditional Chinese medicine exercise and drug treatment in different disease courses and various types of neck pain; secondly, a unified intervention plan for traditional Chinese medicine exercise (such as standard movements, practice frequency and duration in traditional Chinese medicine) and evaluation criteria for efficacy should be formulated to reduce heterogeneity among studies; thirdly, long-term follow-up studies ( ≥ 1 year) should be conducted to assess the long-term efficacy, recurrence rate and safety of traditional Chinese medicine exercise and drug treatment; finally, the effects of combined treatment with traditional Chinese medicine exercise and drugs should be explored, and the applicable population and optimal treatment plan for combined treatment should be clarified to provide more comprehensive evidence-based basis for clinical treatment.
Conflicts of Interest
None declared.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgment
This work was supported by the National Natural Science Foundation of China (Grant No.82260942).
Author’s Contribution
Conceptualization: GW, SY
Data curation: HS, YL
Formal analysis: JS, JL
Resources: JW, JS
Software: GW, JL
Writing (original draft): GW, HS
Writing (review & editing): SY, JS.YZ.
References
- Wu H, Li Y, Zou C, Guo W, Han F, et al. (2025) Global burden of neck pain and its gender and regional inequalities from 1990-2021: a comprehensive analysis from the Global Burden of Disease Study 2021. BMC Musculoskelet Disord 26: 94.
- Safiri S, Kolahi AA, Hoy D, Buchbinder R, Mansournia MA, et al. (2020) Global, regional, and national burden of neck pain in the general population, 1990-2017: systematic analysis of the Global Burden of Disease Study 2017. BMJ 368: 791.
- Kazeminasab S, Nejadghaderi SA, Amiri P, Pourfathi H, Araj-Khodaei M, et al. (2022) Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord 23: 26.
- Mingels S, Granitzer M, Jull G, Dankaerts W (2025) The occurrence of cervicogenic headache: Amapping review. Musculoskelet Sci Pract 77: 103290.
- Kim R, Wiest C, Clark K, Cook C, Horn M (2018) Identifying risk factors for first-episode neck pain: A systematic review. Musculoskelet Sci Pract 33: 77-83.
- Binder AI (2007) Cervical spondylosis and neck pain. BMJ 334: 527-531.
- Hogg-Johnson S, Velde G, Carroll LJ, Holm LW, Cassidy JD, et al. (2008) The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 33: 39-51.
- Mazanec D, Reddy A (2007) Medical management of cervical spondylosis. Neurosurgery 60: 43-50.
- Zoete RM, Armfield NR, McAuley JH, Chen K, Sterling M (2020) Comparative effectiveness of physical exercise interventions for chronic non-specific neck pain: a systematic review with network meta-analysis of 40 randomised controlled trials. Br J Sports Med 54: 1307-1315.
- Gao Q, Li X, Pan M, Wang J, Yang F, et al. (2024) Comparative Efficacy of Mind-Body Exercise for Treating Chronic Non-Specific Neck Pain: A Systematic Review and Network Meta-Analysis. Curr Pain Headache Rep 28: 507-523.
- Peloso P, Gross A, Haines T, Trinh K, Goldsmith CH, et al. (2007) Medicinal and injection therapies for mechanical neck disorders. Cochrane Database Syst Rev 2007: CD000319.
- Huo L, Liu G, Deng B, Xu L, Mo Y, et al. (2024) Effect of use of NSAIDs or steroids during the acute phase of pain on the incidence of chronic pain: a systematic review and meta-analysis of randomised trials. Inflammopharmacology 32: 1039-1058.
- Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J (2018) A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in the Elderly. Aging Dis 9: 143-150.
- Huang JF, Meng Z, Zheng XQ, Qin Z, Sun XL, et al. (2020) Real-World Evidence in Prescription Medication Use Among U.S. Adults with Neck Pain. Pain Ther 9: 637-655.
- Lauche R, Wayne PM, Fehr J, Stumpe C, Dobos G, et al. (2017) Does Postural Awareness Contribute to Exercise-Induced Improvements in Neck Pain Intensity? A Secondary Analysis of a Randomized Controlled Trial Evaluating Tai Chi and Neck Exercises. Spine (Phila Pa 1976) 42: 1195-1200.
- Castellini G, Pillastrini P, Vanti C, Bargeri S, Giagio S, et al. (2022) Some conservative interventions are more effective than others for people with chronic non-specific neck pain: a systematic review and network meta-analysis. J Physiother 68: 244-254.
- Liu X, Pan F, Wang Q, Wang S, Zhang J (2024) Traditional Chinese Rehabilitation Exercise (TCRE) for Myofascial Pain: Current Evidence and Further Challenges. J Pain Res 17: 2801-2810.
- Kong L, Ren J, Fang S, He T, Zhou X, et al. (2022) Traditional Chinese Exercises on Pain and Disability in Middle-Aged and Elderly Patients With Neck Pain: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front Aging Neurosci 14: 912945.
- Lauche R, Stumpe C, Fehr J, Cramer H, Cheng YW, et al. (2016) The Effects of Tai Chi and Neck Exercises in the Treatment of Chronic Nonspecific Neck Pain: A Randomized Controlled Trial. J Pain 17: 1013-1027.
- Shao Y, Han JY, Li HL, Ren ZP, Yang H (2024) Effect of traditional Chinese exercises on the physical and mental health of stroke patients: a meta-analysis. Front Neurol 15: 1455679.
- Lu Y, Li J, Ni W, Li J, Song J, et al. (2023) Effectiveness of mind-body exercise via Baduanjin on physical and psychological outcomes in patients with pulmonary ground-glass nodules: A non-randomized controlled pilot study. Complement Ther Clin Pract 50: 101679.
- Wang X, Luo H (2024) Effects of traditional Chinese exercise therapy on pain scores, sleep quality, and anxiety-depression symptoms in fibromyalgia patients: a systematic review and meta-analysis. BMC Musculoskelet Disord 25: 99.
- Yeung A, Lepoutre V, Wayne P, Yeh G, Slipp LE, et al. (2012) Tai chi treatment for depression in Chinese Americans: a pilot study. Am J Phys Med Rehabil 91: 863-870.
- Yu Y, Wu T, Wu M, Liu S, Chen X, et al. (2024) Evidence map of traditional Chinese exercises. Front Public Health 12: 1347201.
- Cohen SP (2015) Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc 90: 284-299.
- Fu F, Liu B, Gu H, Chen L, Chen X, et al. (2025) Temporal trends in neck pain prevalence among adolescents and young adults aged 10-24 from 1990 to 2019. Arch Med Sci 21: 514-525.
- Xia W, Liu J, Liu C, Xu S, Wang K, et al. (2024) Burden of neck pain in general population of China, 1990-2019: An analysis for the Global Burden of Disease Study 2019. J Glob Health 14: 04066.
- Hoy D, March L, Woolf A, Blyth F, Brooks P, et al. (2014) The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73: 1309-1315.
- Corp N, Mansell G, Stynes S, Wynne-Jones G, Morsø L, et al. (2021) Evidence-based treatment recommendations for neck and low back pain across Europe: A systematic review of guidelines. Eur J Pain 25: 275-295.
- Dong Y, Kuang X, Dong L, Chao G, Qi J, et al. (2023) Exploring the efficacy of traditional Chinese medicine exercise in alleviating anxiety and depression in older adults: a comprehensive study with randomized controlled trial and network meta-analysis. Front Psychol 14: 1290471.
- Oliveira-Souza AIS, Barbosa-Silva J, Gross DP, Costa BR, Ballenberger N, et al. (2025) Comparative effectiveness of manual therapy, pharmacological treatment, exercise therapy, and education for neck pain (COMPETE study): protocol of a systematic review with network meta-analysis. Syst Rev 14: 30.
- Dai M, Luo Z, Hu S, Chen H, Yang J, et al. (2023) Effects of traditional Chinese exercises on the rehabilitation of patients with chronic heart failure: A meta-analysis. Front Public Health 11: 1139483.
- Tang H, Huang W, Ma J, Liu L (2018) SWOT analysis and revelation in traditional Chinese medicine internationalization. Chin Med 13: 5.
- Chen T, Li J, Wang Y, Xie R, Dong L, et al. (2025) Global Research on the Treatment of Cancer Patients During the COVID-19 Pandemic: Visualisation and Bibliometric Analysis. Clin Oncol (R Coll Radiol) 40: 103774.
- Saeed SA, Cunningham K, Bloch RM (2019) Depression and Anxiety Disorders: Benefits of Exercise, Yoga, and Meditation. Am Fam Physician 99: 620-627.
- Tian Y, Liu ZY, Wang JH, Qian JH (2025) The efficacy and safety of Baduanjin exercise as complementary therapy for pain reduction and functional improvement in knee osteoarthritis: A meta-analysis of randomized controlled trials. Complement Ther Med 88: 103127.
Citation: Wang G, Yang S, Long Y, Sun H, Si J, Li J, et al. (2025) Efficacy and Safety of Traditional Chinese Medicine Exercise Versus Medicine in the Treatment of Neck Pain: a Systematic Review and Meta-Analysis. HSOA J Altern Complement Integr Med 11: 640.
Copyright: © 2025 Guancheng Wang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

