
Efficacy of a Trigger-Pointinhibitor Device as Bridge Therapy in Patients Affected by Discal Protrusion and Low Back Pain
*Corresponding Author(s):
A PaladiniRadiology Institute, Services Diagnosis And Therapies Department, Maggiore DellaCarità Hospital, University Of Eastern Piedmont - UPO University, Novara, Italy
Tel:+39 03213732167,
Email:andreapaladini1988@gmail.com
Abstract
Purpose: We evaluated safety and efficacy of a neuromuscular device (Trigger drop®) capable of giving relief from muscular and articular pain. Placed on the trigger points, it acts on crossed muscular fibers points with an analgesic effect. The Dropping technique consists in applying devices of different shapes on the patients’ skin in different positions.
Materials and Methods: We enrolled 59 symptomatic patients candidate to percutaneous chemonucleolysis because of cervical (22 patients) and lumbar (37 patients) disc protusion. The treatment’s efficacy was evaluated with a Visual Analogic Scale (VAS) before and after the device placement. All patients were asked to interrupt the pharmaceutical analgesic therapy from the day of the device’s placement.
Results: The devices obtained an immediate relief of symptoms in 80% of cases, with a 69% mean reduction of the initial VAS [100-40]; while 20% of patients required additional analgesic drugs during the use of Trigger-Drop®. One self-limiting complication was reported in two patients (cutaneous erythema).
Discussion: In our experience, the application of Trigger-drop® in patients waiting for percutaneous chemonucleolysis was safe and effective in the short-term reduction of pain and in the improvement of the quality of life. The treatment proved effective in limiting the need for pharmacologic therapies and it acted as a useful “bridge” therapy towards the interventional radiology treatment.
Keywords
Back pain; Disk; Interventional radiology; Protrusion; Treatment; Trigger-point
INTRODUCTION
Throughout life, around 80% of the people in Western populations has at least one episode of back-pain caused by a diskprotrusion [1]. The most frequent disk protrusions involve the cervical and lumbar spinal tracts, while the dorsal tractis rarely involved. The condition affects mostly the people aging from 40 to 60 years [1,2].
All patients affected by adisk protrusion, regardless of the involved intervertebral disk, have the following features in common:
- • Different severity of pain often caused by a physical effort or a sudden movement. Paresthesiaand reduction of sensitivity and strength of the limbs can be observed.
- • Poorer quality of life in the daily activities.
- • Frequent need for analgesic pharmaceutical therapy (NSAID and Steroids)
Different types of treatment for the discopathies are reported in literature: nucleoplasty, ozone-therapy, percutaneous chemonucleolysis etc. All the aforementioned treatments have a common therapeutic target: the symptoms resolution and the reduction analgesic pharmaceutical therapy [3-7].
Regardless of the treatment, most patients go through a similar therapeutic iter across different departments: after undergoing a radiological evaluation (usually MRI) the patientsmay consult the interventional radiologistand undergo a more or less invasive Interventional Radiology (IR) procedure after a variable waiting time, from few weeks to several months [8,9]. Between the first consultation and the IR procedure, analgesic drugs are usually used to control pain.
We built a randomized perspective study with the application of Trigger-Drop® in patients affected by lumbar and cervical back pain associated or notwith radiculopathy. Moreover, we performed a clinical follow-up, from the first consultation until the interventional procedure, evaluating the devices efficacy as a “bridge to treatment”. We matched this group with a control group.
In our center the main therapy for disk protrusions is percutaneous chemonucleolysis performed in Day-Hospital routine.
MATERIALS AND METHODS
We designed a single-center, randomized and perspective study so as to evaluate the efficacy and safety of “Trigger-Drop”. Patients included in the study had a bulging disk (documented on MRI exam performed no longer than 30 days before the first IR consultation) and were affected by a cervical or lumbar back pain with or without radiculopathy. As aconsequence, they were eligible forapercutaneous IR procedure (chemonucleolysis).
Asymptomatic patients or symptomaticpatients not eligible for a percutaneous treatment were excluded from the study, as well as all patients with no radiologic signs of bulging disks or affected by concomitant pathologies that could reduce the possibility of evaluating the result of our treatment (psychiatric disorders, recent surgery in the same area, dementia).
Between April 2019 and March 2020, we consulted 92 patients with back pain for a possible IR procedure. 69 of them had a bulging disk but only 59 were candidates to the percutaneous procedure of chemonucleolysis and were therefore enrolled in the study.
The enrolled patients were randomized and divided in two cohorts (Table 1):
|
TAB 1 |
Controls |
Cases |
|
Sample |
200 (100%) |
39 (100%) |
|
Age |
65.1 ± 9.9 months |
60.1 ± 11.8 months |
|
Sex |
8 M; 12 F |
16 M; 23 F |
|
Cervical Hernia |
9 (45%) |
15 (38.5%) |
|
Lumbar Hernia |
11 (55%) |
24 (61.5%) |
|
Therapy |
16 (80%) |
30 (76.9%) |
|
Irradiation |
12 (60%) |
18 (46.1%) |
|
Pain Duration |
34.8 ± 21.9 |
15.5 ± 13.3 |
|
BMI |
28.1 ± 3.4 |
25.2 ± 3.6 |
|
VAS pre-trigger |
7.4 ± 1.2 |
7.9 ± 1.3 |
|
Chemionucleolisis |
18 (90%) |
23 (58.9%) |
Table 1: Study population.
- • Group 1 (cases): 39Patients with application ofTrigger-Drop on their first consultation. The device was kept on site until the day of percutaneous procedure (21±8,4 days later).
- • Group 2 (controls): 20 Patients without application of Trigger-Drop with pain control obtained with the pharmacological and/or physiotherapeutic treatment until the procedure.
Patients in both the cohorts presented similar demographic characteristics, suchas mean age and BMI: 37 patients had a lumbar bulging disc (27 cases and 10 controls) and 22 were affected by a cervical bulging disc (12cases and 10 controls).
In the design of the perspective study our primary endpoint was:
- • Reduction of pain (evaluated with a Visual Analogue Score – VAS) of more than 4 points in Group 1 vs Group 2.
Our secondary endpoint was:
- • Suspensions of pharmacological and physiotherapeutic therapies in patients who received Trigger Drop application.
In the Trigger-Drop group (group 1) the mean time of the procedure was measured. On the first radiological consultation, the Interventional Radiologist analyzed the MRI of the affected segment (Figure 1) and evaluated clinical and anamnestic information.
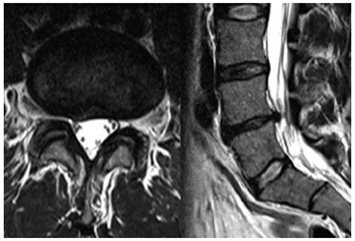 Figure 1: Lumbar discal protrusion.
Figure 1: Lumbar discal protrusion.
Patient affected by Low back pain. Axial (left) and sagittal (right) MRI reported a median discal protrusion associated with dehydration of the intervertebral disc.
The radiological examination is mandatory in order to evaluate the treatment feasibility and indication. Clinical informations are important in order to assess symptoms, functional limitations and the use of painkillers or other medical therapies (such as anticoagulants).
The Visual Analogue Scale (VAS) was used to evaluate the functional limitation and pain.
All patients enrolled in the study reported a localized pain with an initial VAS from 6 to 10. No significant difference in the mean value of VAS in both the study arms (7,9 VAS in group 1, 7.2 VAS in group 2) was found.
After the first visit, patients were randomized in two groups and the Trigger Drop devices were applied in the subjects included in group 1 we placed. All the devices were placed by an expert operator and all the patients did not reported any kind of pain during the procedure.The application of Trigger-Drop took place after the precise localization of the Trigger Point® (that is point where the patient reports the most acute pain) and its inhibiting point (the point on the skin that reduces or inhibits the trigger point when pressed as seen in figures 2 and 3), found through a Test-Pen that allows the operator to apply a modest pressure on a specific point stimulating the inhibitingpoint and relieving the reportedpain. The patient’s collaboration is mandatory because the patient himself guides the operator and helps localizing the exact inhibiting point. This point is found following the theory of the crossed muscle chains and it is usually located on the opposite point of the hurting muscle fascia.
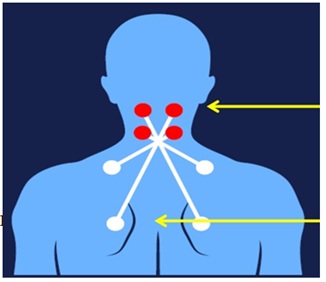 Figure 2: Neck pain Trigger Drop application. Trigger-Drop application in Patient affected by neck pain. Pain location (red round), Trigger-point inhibitor point (white round).
Figure 2: Neck pain Trigger Drop application. Trigger-Drop application in Patient affected by neck pain. Pain location (red round), Trigger-point inhibitor point (white round).
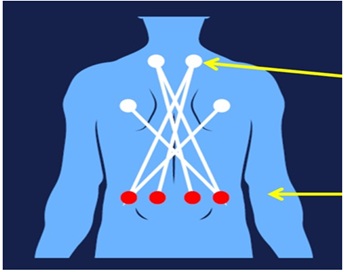 Figure 3: Low back pain Trigger Drop application. Trigger-Drop application in Patient affected by low back pain. Pain location (red round), Trigger-Point inhibitor point (white round).
Figure 3: Low back pain Trigger Drop application. Trigger-Drop application in Patient affected by low back pain. Pain location (red round), Trigger-Point inhibitor point (white round).
Once the inhibiting point (Trigger-Point®) is found, the Trigger-Drop device is fixed to the skin with a patch. The efficacy of the device is immediate. This is a fundamental characteristic to understand whether it is necessary to add a pharmacological therapy or if the device is sufficient to completely control the pain. The presence of very diffuse pain makes it difficult to find the trigger point.
STATISTICAL ANALYISIS
Each numeric variable was described as a percentage rate with its standard deviation. The data analysis has been carried out comparing independent groups with parametric tests such as Student’s T and analysis on contingency tables 2 by 2. Where the conditions of validity of the parametric tests were not met, the corresponding nonparametric test was used.
RESULTS
Follow-up for both cohorts was performed with telephone interviews every 7 days from the first visit to the percutaneous procedure. Modifications in pain, need for medical therapy or adverse reactions where noted.
The mean procedural time for the device application was around 10,5 minutes IC 95% (18,8-6,2).
In group 1 the immediate variation in VAS after Trigger Drop application was measured (time 1). For both patient groups, the mean time between the first visit and the percutaneous surgery was around 21±8,4 days. During this period of time, a telephone follow-up was made to analyze data such as VAS and variations in pharmacological therapy and-in group 1- adverse reactions.
Data on pre-procedural VAS and pharmacological therapy were also collected. Trigger-Drops were removed immediately before the procedure.
No major complications were encountered in group 1, except for a vague erythematous reaction appeared in two patients on the first week but self-limiting in the following days.
The primary endpoint (reduction >4points on VAS after the first Trigger Drop application) was reached in 79.4% (30 Patients). This percentage declined to 66.7% (26 Patients) on the day of the procedure. The remaining cases had a VAS reduction < 4 points. In group 2 (control group), there were no significant variations in VAS in the period of time between the first visit and the day of the procedure.
Regarding the secondary endpoint, the complete suspension of the pharmacologic therapy after Trigger-Drop application, it was obtained in 74.4% of cases (29 Patients).
DISCUSSION
TriggerDrop® is a recently introduced device, thereforethere are no other studies in literature to confirm its efficacy for the treatment of back pain.
This study is not focused on the interventional percutaneous treatment, but conversely on the efficacy and safety of this new device, that acts as a pain reliever. The analysis was focused on the period of time between the first clinical assessment and the IR procedure.
Back pain is one of the most common reason for seeking a medical consult; according to the American College of Physicians [10], a quarter of the adult population in the USA has suffered for at least a day of back pain in the last 3 months. This symptom is responsible for many costs for the healthcare system, both direct - due to the surgical or percutaneous procedures – and indirect – due to the functional limitation and reduced productivity of the affected people. Back pain can be classified in acute (<4 weeks), subacute (between 4 and 12 weeks) and chronic (>12 weeks) [10]. The radicular painis characterized by the association between pain, weakness and inferior limbs paraesthesias.
In a percentage between 26% and 39% of cases, back pain is determined by an inter-somatic disk protrusion; up to a third of patients refers persistent pain of moderate-high intensity for a long period of time (up to one year), with limitations in the daily activities [11]. Various therapeutic options are described in literature for these cases, mostly mini-invasive, requiring a percutaneous approach. The most common IR procedures in clinical practice are: chemonucleolysis, laser, ozone [12].
Planning for these interventions requires a variable period of time from a few days to several weeks. During this time interval patients usually use analgesic therapy to relieve pain. The most commonly used drugs include NSAID and steroids (low efficacy), opioids (moderate efficacy), benzodiazepines and antidepressants (low efficacy reported). Alternatively, or in association to those drugs, a support therapy is usually suggested, such as mild physical activity, acupuncture or physiotherapy. It is undeniable that –at least in the short time period – the described treatments (pharmacological and others) have low reported levels of efficacy in the management of back pain [13].
Our results, although obtained in a limited number of patients, seem to suggest that Trigger-Drop could be a valid alternative to the traditional therapies [14] in the pre-operative management setting.
Trigger-Drop are adhesive plaques realized in inert material (E.V.A - ethylene vinyl acetate) and act as muscolar mediators with immediate efficacy, exploiting the muscular crossed chains to inhibit the trigger-points present on the opposite muscolar fascia. The device is non-magnetic and devoid of any chemical substance and comes in various shapes for an adequate therapeutic use.
The dropping technique requires the application of these devices in various spots on the body depending on the site where the pain is felt and have an immediate analgesic effect.
The results of this study suggest that these new devices may have a high efficacy in the immediate pain reduction in patients affected by a lumbar or cervical disk protrusion. In the group of treated patients, a reduction of >4 points on the VAS scale was obtained in 79, 4% of cases. This resulted in the suspension of pharmacological therapy with a following benefit both in economical and in quality of life terms.
The absence of similar studies in literature, however, doesnot allow for a comparison between this device with other types of treatment in the clinical practice before a surgical or percutaneous therapy.
Analyzing the results of efficacy and safety of Trigger-Drop we can conclude that it is a feasible, fast treatment, which proved safe and devoid of significant complications. This device turned out to be an effective “bridge-therapy” in the percutaneous treatments of cervical and lumbar dischopathy.
ACKNOWLEDGMENT
There are no conflicts of interest.
The authors received no financial support for the research, authorship and publication of this article.
REFERENCES
- Andersson GB (1999) Epidemiological features of chronic low-back pain. Lancet 354: 581-585.
- Kennedy M (1999) IDET: A new approach to treating lower back pain. WMJ 98: 18-20.
- Singh V, Derby R (2006) Percutaneous lumbar disc decompression. Pain Phys 9: 139-146.
- Choy DSJ, Ascher PW, Saddekni S (1992) Percutaneous laser disc decompressions: A new therapeutic modality. Spine 17: 949-956.
- Shields CB (1986) In defense of chemonucleolysis. Clin Neuro Surg 33: 397-405.
- Williams AL, Murtagh FR (2002) Intradiscal electrothermal therapy In: Handbook of diagnostic and therapeutic spine procedures. St Louis: CV Mosby, Missouri, USA.
- Gangi A, Dietemann JL, Ide C, Brunner P, Klinkert A, et al. (1996) Percutaneous laser disc decompression under CTand fluoroscopic guidance: Indications, technique and clinical experience. Radiographics 16: 89-96.
- Galluci M, Limbucci N, Paonessa A, Splendiani A (2007) Degenerative disease of the spine. Neuroimaging Clin N Am 17: 87-103.
- Almen A, Tingberg A, Besjakov J, Mattsson S (2004) The use of reference image criteria in X-ray diagnostics: An application forthe optimisation of lumbar spine radiographs. Eur Radiol 14: 1651-1567.
- Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines Committee of the American College of Physicians (2017) Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline from the American College of Physicians. Annals of Internal Medicine 166: 514-530.
- Carey TS, Evans AT, Hadler NM, Lieberman G, Kalsbeek WD, et al. (1996) Acute Severe Low Back Pain: A Population-based Study of Prevalence and Care-seeking. Spine 21: 339-344.
- Muto M, Giurazza F, Silva RP, Guarnieri G (2016) Rational approach, technique and selection criteria treating lumbar disk herniations by oxygen-ozone therapy. Interventional Neuroradiology 22: 736-740.
- Muto M (2015) Spine intervention. Eur J Radiol 84: 745.
- Barreto TW, Lin KW (2017) Noninvasive Treatments for Low Back Pain. Am Fam Physician 96: 324-327.
Citation: A Paladini, I Percivale, D Negroni, C D’Antona, M Spinetta, et al. (2020) Efficacy of a Trigger-Pointinhibitor Device as Bridge Therapy in Patients Affected by Discal Protrusion and Low Back Pain. J Phys Med Rehabil Disabil 6: 057.
Copyright: © 2020 A Paladini, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

