
Electroacupuncture for Long COVID Depression: A Study of Its Effect on HAMD Scores
*Corresponding Author(s):
Xiangping PengAcuenergie Clinic, Canada
Email:acuenergie@gmail.com
Abstract
Objective: This article presents the results of a study on the effectiveness of electroacupuncture in treating 45 cases of long COVID depression in Eastern Canada and its impact on HAMD scores.
Method: 45 patients (mean age 31.56, range 20–50 years, 53% female, 47% male) with depression after a COVID-19 infection were treated with electroacupuncture using the scalp acupoints DU20 (Baihui), DU24 (Shenting), and EX-HN1 (Sishencong), and the abdominal acupoints ST25 (Tianshu), SP15 (Daheng), and GB26 (Daimai). The duration of each session was 30 minutes. The treatment was administered three times a week for four consecutive weeks. The HAMD Scale was used to assess depression before and after electroacupuncture treatment.
Results: After a 12-treatment course for each of the 45 patients, the overall efficacy rate was obtained by reviewing the HAMD scores before and after treatment. The average pre-treatment scores (22.51±9.99) dropped after 4 weeks of treatment scores (12.06±6.74). There was a statistically significant difference compared to the pre-treatment scores (P<0.05). Nineteen patients were clinically cured, 15 were markedly cured, and 11 were ineffective. The overall effectiveness was 75.56%.
Conclusion: Electroacupuncture has been found to not only treats long COVID depression, but also improves symptoms such as fatigue, sleep quality, and gastrointestinal disorders. It has been shown to be effective in reducing HAMD scores and helping patients recover from depression; restore their mental health; and return to work, school, and social life.
Keywords
Electroacupuncture; HAMD scores; Long COVID depression
Introduction
Long COVID is not yet well defined. The US Centers for Disease Control defines it as the experience of COVID-19-related symptoms, such as fatigue, brain fog, or respiratory, heart, neurological, or digestive symptoms, for more than four weeks after Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infection. It is believed that around 10% of patients develop long COVID [1]. Long COVID depression is a type of depression that affects individuals who have experienced prolonged symptoms of COVID-19 even after they have recovered from the initial infection. This form of depression is typically accompanied by symptoms, such as anxiety, increased fatigue, sleep disturbances, neurocognitive dysfunction, and reduced quality of life. Approximately 35% of patients have been reported to experience depressive psychopathology at different stages of follow-up after SARS-CoV-2 infection [2]. Depression and other mental illnesses have been linked to an increased risk of more severe COVID-19, including the risk of hospitalization, which is a risk factor for long COVID. A study conducted in Wuhan, China in January 2021 found that 23% of participants reported anxiety or depression six months after acute infection and hospitalization for COVID-19 [3]. Neurological and psychiatric sequelae of COVID-19 have also been reported. A study in May 2021 found that nearly a third of COVID-19 patients had been diagnosed with neurological or psychological symptoms, including anxiety, depression, PTSD, and psychosis, within six months of infection [4]. Researchers at Harvard T.H. Chan School of Public Health have found that psychological distress, such as depression, anxiety, worry, perceived stress, and loneliness, before COVID-19 infection is associated with a higher risk of long COVID [5].
General information
A total of 45 patients with long COVID depression were treated at the Acuenergie Acupuncture Clinic from June 2020 to June 2022. The age range of the patients was 20–50 years, and the breakdown of case distribution by age range was as follows: 23 cases in the age group of 20–30 years, 15 cases in the age group of 31–40 years, and 7 cases in the age group of 41–50 years. The study included 24 female and 21 male patients. The average age was 31.56±8.0 years. The mean time between the initial positive PCR test and initial acupuncture treatment was 5.02±1.47 months (Table 1).
Measures of depression
The Hamilton Depression Rating Scale 17-Item (HAMD17) was used in this study. It is the most widely used clinician-administered depression assessment scale [6]. The patients were rated by a clinician on 17 items, each of which was rated from 0 to 2 or 0 to 4. A score of 0 indicated that the symptom was absent, 1 indicated mild severity, 2 indicated moderate severity, 3 indicated severe severity, and 4 indicated incapacitating severity. The total score was calculated as the sum of the scores for the 17 items. According to the HAMD score level of depression, a score of 0 – 7 indicates normal levels of depression, 8 – 16 indicates mild levels, 17 – 23 indicates moderate levels, and a score above 24 indicates severe levels of depression. The maximum score on the 17-item scale is 52. In general, the higher the total score, the more severe the depression.
There were 19 patients with mild depression (scores of 8 – 16), 20 with moderate depression (scores of 17 – 23), and six with severe depression (scores of 24 – 52). The average scores were (22.51±9.99) (Table 2).
The most common clinical symptoms of long COVID depression among the 45 patients were sadness, anxiety or panic, worry, tiredness, low self-esteem, frustration, anger, feelings of hopelessness, low mood, difficulty concentrating, loss of appetite, Irritable Bowel Syndrome (IBS), and sleep disruption (insomnia or hypersomnia).
|
Characteristic |
Values (n/%) |
|
Age , years, mean (SD) |
31.56 (8.0) |
|
Age group |
|
|
20 – 30 |
23 (51.1%) |
|
31 – 40 |
15 (33.3%) |
|
41 – 50 |
7 (15.6%) |
|
Gender |
|
|
Female |
24 (53.3%) |
|
Male |
21 (46.7%) |
|
Body mass index, mean (SD) |
20.11 (2.3) |
|
Months since positive PCR test, mean (SD) |
5.02 (1.47) |
|
Vaccinated (first shot) before positive PCR test |
|
|
Yes |
35 (77.8%) |
|
No |
10 (22.2%) |
|
COVID PCR test positive, numbers (year) |
10 (2020) |
|
21 (2021) |
|
|
14 (2022) |
Table 1: Clinical characteristics of 45 patients.
*Values are numbers (percentages), unless stated otherwise.
|
Scores |
Numbers |
Percentages |
|
HAMD-17 scores, mean (SD) |
45 |
22.51 (9.99) |
|
Mild ( 8 – 16) |
19 |
42.22% |
|
Moderate (17 – 23) |
20 |
44.44% |
|
Severe (24 – 52) |
6 |
13.33% |
Table 2: Hamilton Depression Rating Scale 17-Item (HAMD17).
*The baseline of average scores was (22.51±9.99).
Treatment acupoints and methods
Acupoints: Group 1: see figure 1
- DU20 (Baihui)
- DU24 (Shenting)
- EX-HN1 (Sishencong)
Group 2: see figure 2
- ST25 (Tianshu)
- SP15 (Daheng)
- GB26 (Daimai)
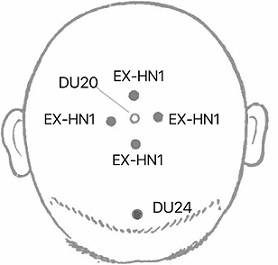 Figure 1: Needling Technique and Manipulation of Group 1.
Figure 1: Needling Technique and Manipulation of Group 1.
Note: Images were created by the authors. The locations of acupoints were referenced from Xuemin S. (2009), Practical Acupuncture. Beijing: China Press of Traditional Chinese Medicine.
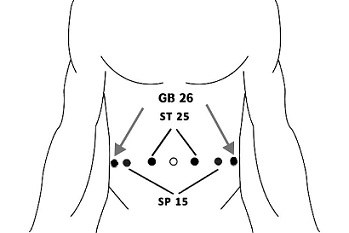 Figure 2: Needling Technique and Manipulation of Group 2.
Figure 2: Needling Technique and Manipulation of Group 2.
Note: Images were created by the authors. The locations of acupoints were referenced from Xuemin S. (2009), Practical Acupuncture. Beijing: China Press of Traditional Chinese Medicine.
Manipulation and methods
The intervention was performed using an electroacupuncture device (KWD-808I, Greatwall). The size of the disposable sterile needles used was 0.25 x 25 mm. After disinfecting all points with a cotton ball dipped in alcohol, the needles were inserted 30° to the scalp and 90° to the abdomen. After inducing de-qi sensations, the electroacupuncture device was connected to six needles. The six acupoints in groups 1 and 2 were alternately divided into three pairs. Then, each pair connected the wires of the positive and negative poles to the two needle handles randomly and set them to a continuous wave at 2 Hz. The duration of each session was 30 minutes. The frequency of treatment was three times a week for four consecutive weeks. Two groups of acupoints were used.
Outcomes
The overall effectiveness rate was calculated as follows: (number of clinically cured patients + number of markedly effective patients) / total number of patients × 100. After a 12-treatment course for each of the 45 patients, electroacupuncture alleviated both mental and physical symptoms, such as sadness, anxiety, panic, worry, tiredness, low self-esteem, frustration, anger, feelings of hopelessness, low mood, lack of concentration on everyday things, loss of appetite, irritable bowel syndrome, and sleep disruption. The overall health condition of the 45 patients, including mood, energy, sleep, and appetite, also improved.
Of the 45 patients, 19 were clinically cured, 15 were markedly cured, and 11 were cured ineffectively. The overall effectiveness rate was 75.56% (Table 3). The HAMD scores decreased at each level. There were 19 patients in the normal range (scores < 7), 15 in the mild range (scores of 8 – 16), 5 in the moderate range (scores of 17 – 23), and 6 in the severe range (scores of 24), but their scores dropped from 52 to 24. The average scores from 22.51±9.99 dropped to 12.06±6.74. The total number of patients with each level of depression decreased (Table 4). There was a statistically significant difference between the HAMD scores before and after treatment (P < 0.05) (Table 5).
|
Depression |
Clinically cured |
Markedly effective |
Ineffective |
Total rate |
|
N=45 |
19 (42%) |
15 (33%) |
11 (24%) |
75.56% |
Table 3: Outcomes of the 45 cases of long COVID Depression (n (%)).
|
|
Before treatment |
After 2 weeks |
After 4 weeks |
|||
|
|
Level |
Numbers (n/%) |
Level |
Numbers (n/%) |
Level |
Numbers (n/%) |
|
Depression |
Normal |
0(0%) |
Normal |
7 (15.6%) |
Normal |
19 (42.2%) |
|
(N=45) |
Mild |
19 (42.2%) |
Mild |
16 (35.6%) |
Mild |
15 (33.3%) |
|
|
Moderate |
20 (44.4%) |
Moderate |
16 (35.6%) |
Moderate |
6 (13.3%) |
|
|
Severe |
6 (13.3%) |
Severe |
6 (13.3%) |
Severe |
5 (11.1%) |
Table 4: Comparison of numbers of depression before and after treatment.
|
|
Before treatment |
After 2 weeks |
After 4 weeks |
|
HAMD-17 scores |
22.51±9.99 |
16.64±6.61* |
12.06±6.74# |
Table 5: Comparison of HAMD scores before and after treatment (N=45)
*Statistically significant differences were found in HAMD scores before and after treatment. (*P < 0.05, #P < 0.05).
Discussion
Depression in traditional Chinese medicine (TCM)
According to the theory of Traditional Chinese medicine (TCM), depression belongs to the category of "Yu syndrome" that first appeared in the foundational treatise Medical Story (in Chinese, ![]() ), written by Yu Tuan, a famous physician from the Ming Dynasty (1438 – 1517). Yu syndrome is a sentimental disease that manifests with chest distress, belching, palpitation, insomnia, fatigue, irritability, and weeping. From the perspective of TCM, Yu syndrome is a disorder of qi and blood movement, imbalance of yin and yang, and accumulation of phlegm and blood stasis due to seven internal emotional injuries. It is located in the brain and involves the heart, liver, spleen, and kidneys [7]. The treatment strategy in TCM is to soothe the liver; invigorate qi and blood circulation; clear phlegm; and strengthen the heart, spleen, and kidney qi.
), written by Yu Tuan, a famous physician from the Ming Dynasty (1438 – 1517). Yu syndrome is a sentimental disease that manifests with chest distress, belching, palpitation, insomnia, fatigue, irritability, and weeping. From the perspective of TCM, Yu syndrome is a disorder of qi and blood movement, imbalance of yin and yang, and accumulation of phlegm and blood stasis due to seven internal emotional injuries. It is located in the brain and involves the heart, liver, spleen, and kidneys [7]. The treatment strategy in TCM is to soothe the liver; invigorate qi and blood circulation; clear phlegm; and strengthen the heart, spleen, and kidney qi.
The gut-brain connection theory and depression
The brain directly affects the stomach and intestine, and this connection occurs in both ways. A troubled intestine can send signals to the brain, similar to a troubled brain, which can send signals to the gut. This means that stomach or intestinal distress can cause or result in anxiety, stress, or depression. This is because the brain and Gastrointestinal (GI) systems are intimately connected [8]. A clinical study based on the theory of “brain-intestine” interaction showed that the abdominal acupoints ST25, RN12, and EN6 play valuable roles in treating depression [9]. A study demonstrated in an animal model closer to humans than the usual rodent models that Electroacupuncture (EA) at specific acupoints can modulate gut-brain axis communication, brain activity, and neurocognitive functions related to food pleasure and motivation [10].
Depression and Acupuncture & Electroacupuncture
Acupuncture, a branch of traditional Chinese Medicine (TCM), has been used to treat a wide range of diseases for over 2,000 years, and is generally regarded as a safe and effective method. Acupuncture is not only effective for post-COVID-19 treatment, but is also effective in preventing recurrence after recovery [11]. Electroacupuncture (EA) is a form of acupuncture in which a small electric current is passed through the acupuncture needles. This type of acupuncture is thought to enhance the effects of traditional acupuncture by stimulating acupuncture points using gentle electric current. For several decades, EA stimulation has been used to treat various mood disorders. A randomized controlled pilot study suggested that electroacupuncture is effective in the treatment of depression [12]. Electroacupuncture (EA) can alleviate symptoms in patients with depressive disorders without negative side effects [13-15]. Another randomized clinical trial found that electroacupuncture with standard care significantly alleviated insomnia in patients with depression [16].
A multicenter, randomized controlled trial evaluated the efficacy and safety of electroacupuncture treatment for depression [17]. Studies have found that electroacupuncture can regulate neurotransmitter levels of serotonin (5-HT), Noradrenaline (NE) and Dopamine (DA) in animal models of depression [18]. Electroacupuncture has both anti-inflammatory and cardio-protective effects [19]. Specifically, low-frequency EA causes the release of many neuropeptides, serotonin, endogenous opioids, and oxytocin in the Central Nervous System (CNS), which seems to be essential for inducing functional changes in different organ systems [20].
Based on the theory of Traditional Chinese medicine (TCM), the combination of scalp acupoints DU20 (Baihui), DU24 (Shenting), EX-HN1 (Sishencong), and abdominal acupoints ST25 (Tianshu), SP15 (Daheng), and GB26 (Daimai), most frequently used to treat depression, can alleviate depressive symptoms by dispersing liver qi and relieving qi and blood stagnation [21-23]. In animal studies, electroacupuncture at acupoints Shen Ting, Baihui, and Neiguan increased the activity of the antioxidant enzyme Superoxide Dismutase (SOD) and decreased the content of the oxidative stress marker Malondialdehyde (MDA) in the brain tissue of rats. This suggests that EA may improve the learning ability of rats with vascular dementia and enhance the ability of the body to scavenge free radicals [24]. EA may also regulate sympathetic nerve function and activate cholinergic neurons, which release chemical mediators such as serotonin and acetylcholine, thereby improving blood circulation and brain metabolism. Additionally, electroacupuncture may dilate capillaries and improve nutrient metabolism in the brain [25]. Electroacupuncture can restore the nutrient metabolism function of capillaries by dilating them, reducing blood flow resistance, and removing attachments in the capillary lumen [26].
Acupuncture at the Sishencong acupoints has been shown to enhance the activity of nitric oxide synthase (NOS), increase the content of Nitric Oxide (NO), adjust sleep issues and various neurological symptoms, and promote brain function. It can also significantly improve the thymus index, spleen index, and blood leukocyte count and enhance SOD activity in the brain [27]. A clinical study also found that acupuncture at the DU20 acupoint may be effective in treating post-stroke depression [28]. Overall, the research suggests that EA may have various neurological and physiological effects that can improve brain function and treat certain conditions.
The functions of selected electroacupoints are listed below
The DU20 (Baihui): Acupoint is located at the intersection of the governor meridian, the three yang meridians of the hand and foot, and the liver meridian. It is situated above the head, which is believed to be the organ of the primordial spirit in traditional Chinese medicine (TCM). In TCM, Baihui is referred to as "the sect of a hundred meridians, the meeting point of a hundred spirits" (in Chinese, ![]() ), and is believed to have the ability to regulate the mind, refresh the mind, relieve evil wind, and resolve phlegm.
), and is believed to have the ability to regulate the mind, refresh the mind, relieve evil wind, and resolve phlegm.
DU24 (Shenting): Also known as "Spirit Courtyard," is an important and powerful acupoint that benefits the brain and calms the mind and spirit. It is located at the intersection of the Governing Vessel with the Bladder and Stomach Channels. The main indications for its use include poor memory, anxiety, vertigo, insomnia, epilepsy, dizziness, depression, blurred vision, allergic rhinitis, and a runny nose.
EX-HN1 (sishencong): Is a star-shaped group of acupoints located around the DU20 at the vertex of the head (Figure 1). The front and rear acupoints were situated on the line of the Du meridian, whereas the left and right acupoints were on the line of the bladder meridian. The Du meridian, which passes through the spine, belongs to the kidney and enters the brain, while the bladder meridian crosses the forehead and ascends to the top of the brain. EX-HN1 (Sishencong) is commonly used to treat insomnia and regulate sleep as well as a variety of mental and nervous symptoms. It is effective in treating a range of neurological and psychological diseases, with the main indications being headache, vertigo, insomnia, poor memory, and epilepsy.
ST25 (Tianshu): Is located on the stomach meridian of foot yangming and is commonly used for the treatment of abdominal pain, bloating, constipation, diarrhea, dysentery, irregular menstruation, and dysmenorrhea. In clinical practice, it is often used to treat abdominal pain, bloating, constipation, diarrhea, irregular menstruation, indigestion, acute and chronic gastritis, and enteritis. Tianshu is known to be effective in treating emotional volatility and mood swings as well as fluctuations in energy levels.
SP15 (Daheng): Belongs to the Spleen Meridian of Foot-Taiyin and is commonly used to treat abdominal pain, diarrhea, constipation, dysentery, and intestinal ascariasis. In clinical practice, it is used to treat constipation, intestinal carbuncle caused by stagnation of qi, diarrhea due to cold evils, abdominal pain, and physical weakness with hyperhidrosis.
GB26 (Daimai): Belongs to the Gallbladder Meridian of Foot-Shaoyang and is commonly used to treat dysmenorrhea, irregular menstruation, leucorrhea, amenorrhea, hernia, lower back pain, uterine prolapse, pelvic inflammatory disease, and other conditions. In clinical practice, it is used to treat irregular menstruation, amenorrhea, leukorrhea, abdominal pain, hernias, and pain in the lumbar and hypochondriac regions.
In summary, electroacupuncture at the scalp acupoints DU20 (Baihui), DU24 (Shenting), EX-HN1 (Sishencong), abdominal acupoints ST25 (Tianshu), SP15 (Daheng), and GB26 (Daimai) have been shown to provide efficient results in the treatment of long COVID-related depression and improve the quality of life in post-COVID-19 syndrome. This is worth promoting in clinical applications.
Conclusion
Electroacupuncture not only treats long COVID depression, but also improves symptoms such as general fatigue, sleep quality, and gastrointestinal disorders. Electroacupuncture has the effect of decreasing HAMD scores and helps patients recover from depression, restore their mental health, and return to work, school, and social life.
Authorship and Contribution
Xiangping Peng prepared this manuscript. Guanhu Yang contributed to the use of traditional Chinese medicine (TCM) theory for depression.
Funding
The authors declare that they did not receive any funding for the preparation of this manuscript.
Conflict of Interest
The authors declare no conflict of interest.
Ethical Compliance
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Data Statement
The data used to support the findings of this study are included within the article.
References
- Greenhalgh T, Knight M, A'Court C, Buxton M, Husain L (2020) Management of post-acute covid-19 in primary care. BMJ 370: 3026.
- Mazza MG, Palladini M, Poletti S, Benedetti F (2022) Post-COVID-19 Depressive Symptoms: Epidemiology, Pathophysiology, and Pharmacological Treatment. CNS Drugs 36: 681-702.
- Huang C, Huang L, Wang Y, Li X, Ren L, et al. (2021) 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 397: 220-232.
- Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ (2021) 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 8: 416-427.
- Wang S, Quan L, Chavarro JE, Slopen N, Kubzansky LD, et al. (2022) Associations of Depression, Anxiety, Worry, Perceived Stress, and Loneliness Prior to Infection With Risk of Post–COVID-19 Conditions. JAMA Psychiatry 79: 1081-1091.
- Hamilton M (1967) Development of a rating scale; for primary depressive illness. Br J Soc Clin Psychol 6: 278-296.
- Lanying L, Lingling W (2003) The Guiding Significance of the Theory of “The Brain is the Home of the Primordial Spirit” in the Treatment of Depression with Acupuncture and Moxibustion. Clinical Journal of Acupuncture and Moxibustion 19: 6-8.
- Harvard Health Publishing (2022) The gut-brain connection. Harvard Health Publishing, USA.
- Zhang X, Fan X, Wang M (2022) The experience of treating depression with acupuncture and moxibustion from the perspective of “brain-intestine” interaction. Proceedings of the 2022 Chinese Acupuncture and Moxibustion Society Annual Conference, China.
- Zhang X, Chen H, Laillet VD (2021) Hypothesis paper: electroacupuncture targeting the gut–brain axis to modulate neurocognitive determinants of eating behavior—toward a proof of concept in the obese minipig model. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity 26: 61-74.
- Peng X (2022) The Effectiveness of Acupuncture in The Treatment of Post COVID-19 Condition: A Retrospective Study. J Gynecol Reprod Med 6: 106-109.
- Sun H, Zhao H, Ma C, Bao F, Zhang J, et al. (2013) Effects of electroacupuncture on depression and the production of glial cell line-derived neurotrophic factor compared with fluoxetine: a randomized controlled pilot study. J Altern Complement Med 19: 733-739.
- Manber R, Schnyer RN, Allen JJ, Rush AJ, Blasey CM (2004) Acupuncture: a promising treatment for depression during pregnancy. J Affect Disord 83: 89-95.
- Leo RJ, Ligot JS (2007) A systematic review of randomized controlled trials of acupuncture in the treatment of depression. J Affect Disord 97: 13-22.
- Whiting M, Leavey G, Scammell A, Au S, King M (2008) Using acupuncture to treat depression: a feasibility study. Complement Ther Med 16: 87-91.
- Yin X, Li W, Liang T, Lu B, Yue H, et al. (2022) Effect of electroacupuncture on insomnia in patients with depression: a randomized clinical trial. JAMA Netw Open 5: 2220563.
- Cai W, Ma W, Chen AW, Shen WD, et al. (2020) Effects of electroacupuncture therapy for depression: Study protocol for a multicentered, randomized controlled trial. Medicine 99: 22380.
- Leung MC, Yip KK, Ho YS, Siu FK, Li WC, et al. (2014) Mechanisms underlying the effect of acupuncture on cognitive improvement: a systematic review of animal studies. J Neuroimmune Pharmacol 9: 492507.
- Xiao Y, Chen W, Zhong Z, Ding L, Bai H, et al. (2020) Electroacupuncture preconditioning attenuates myocardial ischemia-reperfusion injury by inhibiting mitophagy mediated by the mTORC1-ULK1-FUNDC1 pathway. Biomedicine & Pharmacotherapy 127: 110148.
- Victorin SE, Jedel E, Janson PO, Sverrisdottir YB (2009) Low-frequency electroacupuncture and physical exercise decrease high muscle sympathetic nerve activity in polycystic ovary syndrome. Am. J. Physiol. Regul. Integr. Comp. Physiol 297: 387-395.
- He J, Shen PF (2007) Clinical study on the therapeutic effect of acupuncture in the treatment of post-stroke depression. Zhen Ci Yan Jiu 32: 58-61.
- Yan L, Yao F (2013) Observation on clinical curative effect of scalp acupuncture combined with body acupuncture in treating depression with stagnation of liver qi. Journal of Clinical Acupuncture and Moxibustion 2013: 31-32.
- Jing Z (2015) Comparative study on the efficacy of abdominal acupuncture and western medicine in treating menopausal women’s depression. World Latest Medical Information Abstracts 145: 146.
- Lingli G, Xiaodong F (2016) Effects of electro-acupuncture at Shenting and Baihui points on learning and memory ability and the expression of autophagy-related genes and proteins in cognitively impaired rats after cerebral ischemia-reperfusion. Journal of Rehabilitation 26: 17-22.
- Kai X, Xiuling C, Renhan L (2011) Effect of electroacupuncture at Sishencong point on blood of patients with depression Clinical observation on the influence of Qing 5-HT and DA content. New Chinese Medicine 43: 87-89.
- Zhenhua L, Shijun W (2015) Effects of acupuncture on Sishencong and Baihui on the expression of clock genes and amino acid neurotransmitters in brain tissue of rats with insomnia. Chinese Gerontology 35: 6067-6069.
- Gao XY, Ma QL, Hu B (2007) Effects of acupuncture on Sishencong on the physiological function of sleep disorder model mice. China Acupuncture 27: 681-683.
- He J, Shen PF (2007) Clinical study on the therapeutic effect of acupuncture in the treatment of post-stroke depression. Zhen Ci Yan Jiu 32: 58-61.
Citation: Peng X, Yang G (2022) Electroacupuncture for Long COVID Depression: A Study of Its Effect on HAMD Scores. J Altern Complement Integr Med 8: 311.
Copyright: © 2022 Xiangping Peng, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

