
Endochemical Venous Ablation with Foam Prepared with Pure Oxigen, Excellent and Easy Alternative
Abstract
Results
Patients = 1300, adverse effects: Cough (0.15% O2, 3.7% Ra), Dizziness and migraine (0%, O2, 0.53% Ra), Visual disturbances (0%, O2, 0.13% Ra), Back pain (0%, O2, 0.73% Ra). The effectiveness of treatment was the same in both groups, but the Foam prepared with oxygen had better performance. Although Dr.Frullini has demonstrated that endothelin is the cause of the neurologic side effects, the use of physiological gases can prevent most of the undesirable’s effects of the sclerosing Foam. In conclusion, Foam sclerotherapy performed with Oxygen is a good option to reduce or even prevent adverse effects of polidocanol, easy to performance and with better stability in the Foam.
Keywords
INTRODUCTION
METHODS
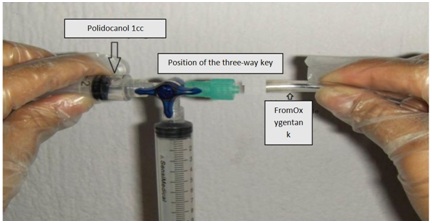 Figure 1: Way to connect the tube from the oxygen tank to prepare the foam.
Figure 1: Way to connect the tube from the oxygen tank to prepare the foam.RESULTS
|
|
Oxygen group (1,300) |
Room air group (1,500) |
||
|
Age (mean) |
54 years |
(28-80 y) |
60 |
(26-82 y) |
|
Male |
32% |
416 p |
28% |
418 p |
|
Female |
68% |
884 p |
72% |
1082 p |
|
Size |
1.6 m |
1.43-1.72 |
1.56 m |
1.40-1.83 |
|
Weight |
71 Kg |
43-120 |
75 Kg |
45-125 |
|
Right |
68 % |
884 legs |
58.4% |
876 p |
|
Left |
76 % |
988 legs |
41.6% |
624 p |
|
Volume (mean) |
14 ml |
3-60 ml |
2.8 ml |
1-15 ml |
|
Concentration (mean) |
1.5% |
(0.5-3)% |
1.5% |
(0.5-3)% |
|
→Veins |
Varicules |
Magnus Saphena |
Accessory saphena |
Cockett I |
Cockett II |
Cockett III |
Boyd |
May perf. |
Giacomini |
Hunter |
|
% |
74 |
16 |
10 |
30 |
12 |
7.5 |
42 |
17 |
8 |
10 |
|
Patients |
2,072 |
448 |
280 |
840 |
336 |
210 |
1,176 |
476 |
224 |
280 |
The side effects were practically eliminated and although at present it is not necessary, different volumes were applied having a maximum volume of 60 ml of Foam with average of 14ml.
The veins injected were the following:
In the Oxygen group there were no side effects, in the room air group there were minor side effects. The effectiveness of the treatment was the same in both groups. We had not secondary neurological effects (Table 3).
|
→Side eeffects |
Cough |
Dizziness and migraine |
Transient blindness |
Back pain |
Faiting |
Patients |
|
Room air |
56 (3.7%) |
8 (0.53%) |
2 (0.13%) |
11 (0.73%) |
2 (0.13%) |
1500 (100%) |
|
Pure oxygen |
2 (0.15%) |
0 |
0 |
0 |
0 |
1300 (100%) |
DISCUSSION
Dr. Frullini and Cols. demonstrated that endothelin is the cause of neurological side effects [12]. We know that the use of physiological gases reduces significantly the side effects, which may be due to some special interaction of nitrogen with the endothelium, which does not occur when CO2 or Oxygen is used [13]. Especially the prevention of neurological effects justifies the use of oxygen as a way to prevent easily these events. Beckitt et al. used a mixture of O2 and CO2 foam with physiological gases to prevent effects such as thrombophlebitis [14]. Although our series are small we must continue the use of physiological gases to prepare foam. It is believed that oxygen is more accessible than CO2, since it is a gas commonly used in doctors’ offices and hospitals. Likewise the Central Nervous System works better with Oxygen than with CO2 and if there are bubbles in some important area, it could be a factor for having or not neurological effects due to transient hypoxia. The duration of the foam with Oxygen is greater than with room air and it is an advantage when working with endovenous chemical ablation (sclerotherapy). More research is needed, although there is sufficient evidence that physiological gases are better than ambient air [15].
CONCLUSION
REFERENCES
- Alder G, Lees T (2015) Foam sclerotherapy. Phlebology 30: 18-23.
- Hamel-Desnos C, Allaert FA (2009) Liquid versus foam sclerotherapy. Phlebology 24: 240-246.
- Cavezzi A, Tessari L (2009) Foam sclerotherapy techniques: Different gases and methods of preparation, catheter versus direct injection. Phlebology 24: 247-251.
- Peterson JD, Goldman MP (2011) An investigation into the influence of various gases and concentrations of sclerosants on foam stability. Dermatol Surg 37: 12-17.
- Morrison N, Neuhardt DL (2009) Foam sclerotherapy: Cardiac and cerebral monitoring. Phlebology 24: 252-259.
- Morrison N, Neuhardt DL, Rogers CR, McEown J, Morrison T, et al. (2008) Comparisons of side effects using air and carbon dioxide foam for endovenous chemical ablation. J Vasc Surg 47: 830-836.
- Rasgado FV, Gallegos JS, Pastrana V, Ramirez C, Rasgado LAV, et al. (2018) Foam prepared with pure oxygen decrease adverse effects in sclerotherapy. Int Angiol 37: 6.
- Tessari L, Cavezzi A, Frullini A (2001) Preliminary experience with a new sclerosing foam in the treatment of varicose veins. Dermatol Surg 27: 58-60.
- Parsi K (2012) Paradoxical embolism, stroke and sclerotherapy. Phlebology 27: 147-167.
- Bush RG, Derrick M, Manjoney D (2008) Major neurological events following foam sclerotherapy. Phlebology 23: 189-192.
- Gillet JL, Donnet A, Lausecker M, Guedes JM, Guex JJ, et al. (2010) Pathophysiology of visual disturbances occurring after foam sclerotherapy. Phlebology 25: 261-266.
- Frullini A, Felice F, Burchielli S, Di Stefano R (2011) High production of endothelin after foam sclerotherapy: A new pathogenetic hypothesis for neurological and visual disturbances after sclerotherapy. Phlebology 26: 203-208.
- Gutierrez LR (2018) How to prevent complications and side effects from sclerotherapy of the lower limb veins. Phlebolymphology 25: 137-153.
- Beckitt T, Elstone A, Ashley S (2011) Air versus physiological gas for ultrasound guided foam sclerotherapy treatment of varicose veins. Eur J Vasc Endovasc Surg 42: 115-119.
- Wong M (2015) Should foam made with physiologic gases be the standard in sclerotherapy? Phlebology 30: 580-586.
Citation: Rasgado FV, Rendón F, Jiménez E, Rasgado LAV, Carmona V, et al. (2019) Endochemical Venous Ablation with Foam Prepared with Pure Oxigen, Excellent and Easy Alternative. J Angiol Vasc Surg 4: 025.
Copyright: © 2019 Fernando Vega Rasgado, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

