
Epidemiological Therapeutic and Prognosis Aspects of Abruptio Placentae in an Insecure Area of Mali, Case of the Hospital of Timbuktu
*Corresponding Author(s):
Fane SeydouDepartement De Gynecologie Obstetrique Du Chu, Gabriel Touré Hospital, Bamako, Mali
Email:seydoufane@yahoo.fr
Traore Youssouf
Departement De Gynecologie Obstetrique Du Chu, Gabriel Touré Hospital, Bamako, Mali
Tel:+00223 66710194,
Email:drtraorey@yahoo.fr
Abstract
Obstetric hemorrhages remain the leading cause of maternal death in the world. In addition, an abruptio placenta is responsible for significant maternal and perinatal mortality in Sub-Saharan Africa. Our objective was to determine the prevalence, the maternal and perinatal prognosis of this pathology at the Timbuktu hospital.
Patients and methods
It’s a cross-sectional descriptive study with retrospective collection over a six - years period from January to December 2018, including all cases of abruptio placentae recorded at the Timbuktu hospital.
Results
We have collected 133 cases of abruptio placentae out of 5999 deliveries, in others words 2.21%. The mean age of the patients was 28 years with a predominance of multiparous patients (32.33%), evacuated (53.38%). No prenatal consultation was performed in 36.09% of cases. Arterial high blood pressure was found in 36.84% of patients and a grade 3 of Sheer in 60.15% (80 cases). The caesarean section rate was 74%. The maternal mortality rate was marked by bleeding disorder in 6.7% anemia requiring blood transfusion in 51.88% of patients. The perinatal mortality rate was 65.22%. The elements of poor perinatal prognosis were represented the severe maternal anemia odds with 95% confidence interval CI at 95% = 15 (3.6-70), the small birth weight ORCI at 95% = 4.8 (2.1-8), non-monitoring of pregnancies ORCI at 95% = 4.7 (2.1-8) and the lack of evacuation.
Conclusion
The maternal and prenatal mortality rate related to abruption placentae is high in our context. Its reduction requires improved prenatal care evaluation conditions and strengthening of the technical platform and qualified personnel.
Keywords
INTRODUCTION
PATIENTS AND METHODS
A cross-sectional study with retrospective data collection was carried out. It was conducted from 2013 to 2018. The study population was composed of all pregnant women 28 weeks of age and older who gave birth at the Timbuktu Hospital during the study period. We included in this study all women who had a retro placental hematoma. The variables studied were socio-demographic data, mode of admission, reference structures, reason for admission, medico-surgical history, evolution of previous pregnancies, pathologies associated with pregnancy, parity, number of prenatal consultation, clinical admission data, paraclinical data, length of hospital stay, maternal progress (complications, deaths), newborn status at birth, weight, sex, score Apgar, resuscitation, prematurity, hypotrophy, perinatal death and factors associated with perinatal mortality. Live newborns whose mothers had a retro placental hematoma were followed during the first 7 days of life in order to know the perinatal prognosis. The statistical tests used were the Pearson Chi2 test, the odds ratio and the significance p. The p was significant if the probability is ≤ 0.05. Ethical aspects have been respected guaranteeing confidential medical information.
RESULTS
Abruptio placentae frequency (Figure 1)
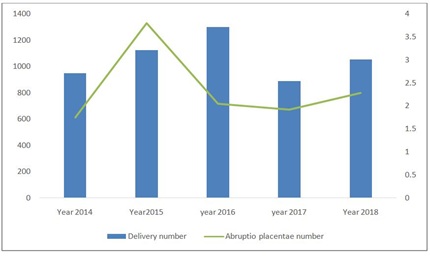 Figure 1: Evolution of the incidence of abruptio placentae in Timbuktu from 2015 to 2018.
Figure 1: Evolution of the incidence of abruptio placentae in Timbuktu from 2015 to 2018.|
Characteristics |
% |
n/n |
|
Age |
||
|
15-19 years old |
11.3 |
15/133 |
|
20-34 years old |
66.1 |
88/133 |
|
35 years old |
22.6 |
30/133 |
|
Profession |
||
|
Housewife |
91.0 |
121/133 |
|
Pupils/students |
6.0 |
8/133 |
|
Merchant/worker |
1.0 |
1/133 |
|
Civil servant |
2.0 |
3/133 |
|
Schooling |
||
|
Non-schooling |
89.0 |
14/133 |
|
Educated |
11.0 |
89/133 |
|
Admission mode |
||
|
Evacuated/referred |
53.0 |
70/133 |
|
Come from herself |
47.0 |
63:133 |
|
Provenance structure |
||
|
Community health center |
35.0 |
47/133 |
|
Reference health center |
1.5 |
22/133 |
|
Medical office |
1.5 |
2/133 |
|
Home |
47.0 |
62/133 |
|
Residence of origin |
||
|
Timbuktu city |
83.5 |
111/133 |
|
Timbuktu city ring road |
4.0 |
5/133 |
|
Gourma-Rharous |
8.0 |
11/133 |
|
Goundam |
1.5 |
2/133 |
|
Niafunke |
1.5 |
2/133 |
|
Dire |
1.5 |
2/133 |
Clinical characteristics of patients
Treatment and prognosis
|
Characteristics |
% |
n/n |
|
Vascular filling |
||
|
Yes |
31 |
41/133 |
|
No |
69 |
92/133 |
|
Delivery route |
||
|
Caesarean |
26 |
35/133 |
|
Vaginal |
74 |
98/133 |
|
Anesthesia |
||
|
General anesthesia |
26 |
35/133 |
|
Locoregional |
4 |
5/133 |
|
None |
70 |
93/133 |
|
Clot weight (grams) |
||
|
< 500 |
15 |
20/133 |
|
≥500 |
15 |
20/133 |
|
Unspecified |
70 |
93/133 |
|
Delay between admission and expulsion (hours) |
||
|
≤ 2 |
74 |
99/133 |
|
> 2 |
26 |
34/133 |
|
Apgar at the first minute |
||
|
Still dead |
66 |
91/138 |
|
1 to 3 |
0.7 |
1/138 |
|
4 to 7 |
14 |
19/138 |
|
≥8 |
19.3 |
27/138 |
|
Transfusion |
||
|
Yes |
52 |
69/133 |
|
No |
48 |
64/133 |
|
State of the newborn |
||
|
Living |
91 |
43/47 |
|
Perinatal deaths |
4/47 |
|
|
Transfer pattern in neonatology |
||
|
Prematurity |
7.5 |
10/133 |
|
Respiratory distress |
4 |
5/133 |
|
Hypotrophy |
3 |
4/133 |
Factors associated with perinatal deaths
|
Factors |
Perinatal deaths |
Khi² |
Odds ratio CI 95 |
P |
||
|
Yes |
No |
|||||
|
Home |
Timbuktu |
71 |
37 |
0.4 |
1,1 (0.4-3.8) |
0.8 |
|
Other |
14 |
8 |
||||
|
Anemia (g/dl) |
? 7 |
36 |
2 |
20 |
0.000 |
|
|
≥ 7 |
44 |
39 |
||||
|
Fetal weight (gram) |
< 2500 |
56 |
16 |
16 |
4.8 (2.2-10.6 |
0.000 |
|
≥ 2500 |
21 |
23 |
||||
|
Antenatal visits |
No |
49 |
10 |
14 |
4.7 (2.1-10.8) |
0.000 |
|
Yes |
36 |
35 |
||||
|
Terms |
< 37 |
40 |
16 |
1.6 |
1.6 (0.7-3.3) |
0.2 |
|
≥ 37 |
50 |
32 |
||||
|
Admission mode |
Reference evacuation |
58 |
13 |
18 |
5.3 (2.3-11.6) |
0.000 |
|
Self - reference |
27 |
32 |
||||
|
High blood pressure |
Yes |
23 |
20 |
2.3 |
0.6 (0.2-1.2) |
0.1 |
|
No |
52 |
25 |
||||
Maternal and perinatal prognosis
DISCUSSION
Rate (Frequency)
Clinical aspects
Maternal and perinatal prognosis
While it is higher than those in developed countries which remains below 1% [16-18]. This thanks to a fast and adapted support in the middle of resuscitation. Our cases of death can be explained on the other hand, by the low health coverage in the peripheral area, the delay of patients to resort to health centers, evacuation conditions and on the one hand, by the insufficiency of effective resuscitation measures in the region. As for the fetal prognosis, it remains dark in our developing countries. In our series, fetal morbidity as dominated by a low birth weight in 55.80% of cases with an average weight of 2250 ranges against 2680 ranges for Thieba in Ouagadougou [9] and 4142 ranges for Thiam in Senegal [1]. Our rate of low birth weight is lower than that of Boisramé T [14] 68.2% in France against higher than that of Madagascar 43.7%. This difference could be explained by an unspecified estimate of this gestational age in our (date of the last imprecise, late ultrasound). The perinatal mortality rate was % (95 cases/ 138); this perinatal mortality rate is close to Coleman J et al., [6] in Nigeria, which found 63.9%. As for stillbirth it was 91 cases/ 138 or 66%; this is lower than that of Nayama [8] which found 71%. This significant proportion is explained by: the low rate of rough forms with live child, the patients often presenting on admission a severe clinical picture (more than 60% of grade 3 of Sheer). Some African authors [5,18-21]. Found as factors of bad perinatal prognosis: the gravity of the clinical picture, the medical evacuation, the importance of the blood clot, the low birth weight, and the way low as a mode of delivery. Factors that were statically associated with perinatal mortality in our setting were: severe maternal anemia, small birth, missed pregnancies and referral/evacuation (Table 3). The perinatal mortality in our study was estimated at 72% comparable to that of Thiam in Senegal 60% (1).
CONCLUSION
PUBLIC DECLARATION OF INTEREST
REFERENCES
- Thiam O, Mbaye M, Diouf AA, Touré FB, Gueye M, et al. (2014) Epidemiological, prognostic and therapeutic aspects of retro placental hematoma (HRP) in a referral maternity in rural area. Pan Afr Med J 17: 11.
- Manuela GM (2016) Abruptio placentae: Inventory of fixtures at Grenoble Teaching Hospital Gynecology and obstet. Dumas-01349693.
- Leunen K, Hall DR, Odendaal HJ, Grové D (2003) The profile and complications of women with placental abruption and intrauterine death. J Trop Pediatr 49: 231-234.
- Musa J, Sagay AS, Ekwempu CC, Ibrahim SA (2007) Analysis of Some Risk Factors for Abruptio Placentae in Jos, Northern Nigeria. Trop J Obstet Gynaecol 24: 11-14.
- Tikkanen M (2011) Placental abruption: Epidemiology, risk factors and consequences. Acta Obstet Gynecol Scand 90: 140-149.
- Coleman J, Srofenyo EK, Ofori EK, Brakohiapa EK, Antwi WK (2014) Maternal and fetal prognosis in abruptio placentae at Korle-Bu Teaching Hospital, Ghana. Afr J Reprod Health 18: 115-122.
- Sananes N, Boisramé T, Langer B (2012) Placental abruptio. EM -Consulte. 2-3.
- Nayama M, Tamakloé-Azamesu D, Garba M, Idi N, Djibril B, et al. (2007) [Abruptio placentae. Management in a reference Nigerien maternity. Prospective study about 118 cases during one year]. Gynecol Obstet Fertil 35: 975-981.
- Thieba B, Lankoande J, Akotionga M, Kyelem C, Ouedraogo A, et al. (2003) [Abruptio placentae: Eepidemiological, clinical and prognostic aspects with respect to a 177 case series]. Gynecol Obstet Fertil 31: 429-33.
- Traore Y, Traore M, Mounkoro N, Teguete I, Sissoko A, et al. [Trauma and pregnancy: Clinical and prognosis about 152 cases recorded into Gabriel Toure Teaching Hospital]. Mali Med 24: 18-20.
- Macheku GS, Philemon RN, Oneko O, Mlay PS, Masenga G (2015) Frequency, risk factors and feto-maternal outcomes of abruptio placentae in Northern Tanzania: A registry-based retrospective cohort study. BMC Pregnancy Childbirth 15: 242.
- Sandjo FD (2013) Clinical epidemiology and therapeutic outcomes of abruptio placentae with living fetus at Teaching Hospital Gabriel Touré. FMOS.
- Mian DB, Guessan K (2003) Abruptio placentae and fetal death in utero: About Anesth Reanim [INTERET].
- Boisramé T, Sananès N, Fritz G, Boudier E, Viville B, et al. (2014) [Abruptio placentae. Diagnosis, management and maternal-fetal prognosis: A retrospective study of 100 cases]. Gynecol Obstet Fertil 42: 78-83.
- Bohec C, Collet M (2010) [Abruptio placentae]. Ann Fr Anesth Reanim 29: 115-119.
- Nkwabong E, Tiomela Goula G (2017) Placenta abruption surface and perinatal outcome. J Matern Fetal Neonatal Med 30: 1456-1459.
- Hall DR (2009) Abruptio placentae and disseminated intravascular coagulopathy. Semin Perinatol 33: 189-195.
- Mukherjee S, Bawa AK, Sharma S, Nandanwar YS, Gadam M (2014) Retrospective study of risk factors and maternal and fetal outcome in patients with abruptio placentae. J Nat Sci Biol Med 5: 425-428.
- De Lee JB (1901) Abruptio placenta. Am J obstet gynecol 44: 785.
- Oyelese Y, Ananth CV (2006) Placental abruption. Obstet Gynecol 108: 1005-1016.
- Akpadza K, Baeta S, Neglo Y (1996) Abruptio placentae Obstetric Gynecol at Teaching Hospital Tokoin-Lomé (Togo) from 1998 to 1992 of black African Medicine (vol-43): 342-347.
Citation: Seydou F, Amadou B, Mamadou K, Ibrahima K, Djibril S, et al. (2019) Epidemiological, Therapeutic and Prognosis Aspects of Abruptio Placentae in an Insecure Area of Mali, Case of the Hospital of Timbuktu. J Reprod Med Gynecol Obstet 4: 031.
Copyright: © 2019 Fane Seydou, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

