
Epithelioid Hemangioendothelioma of Pterygomaxillary Fissure
*Corresponding Author(s):
José Francisco De Sales ChagasDepartment Of Head And Neck Surgery, São Leopoldo Mandic Medical School, Campinas, Brazil
Tel:+55 19997653010,
Email:josechagas@ig.com.br
Abstract
Introduction
Epithelioid Hemangioendothelioma (EH) is an uncommon vascular neoplasm (endothelial origin) which can affect any type of tissue. It rarely occurs in head and neck region, and has unpredictable clinical behavior.
Objective
The aim is to report a case of EH of unusual location (pterygomaxillary fissure) and histological rarity, andto establish an accurate differential diagnosis of EH and Juvenile Nasoangiofibroma (JNA).
Case report
A 19 year-old male with a chief complaint of recurrent epistaxis and an obstruction of the left nasal cavity. The diagnosis of JNA was suggested and surgery with tumor complete resection was the election treatment. However, clinical diagnosis was not confirmed postoperaively, through Immunohistochemistry (IHC). Histopathological findings showed a diagnostic reporting of EH. Tumor had no recurrence within three years after surgery.
Discussion
Apart from the rarity of the condition, EH varies according to their location in asymptomatic or with few symptoms. The presence of violaceous lesions indicates a huge range of vascular tumors. Thus, IHC has assumed very important for diagnosis confirmation.
Conclusion
The localization of EH in perygomaxillary fissure is a rare condition withpoor prognosis. The treatment choice for EH was the complete ressection.
Keywords
INTRODUCTION
CASE REPORT
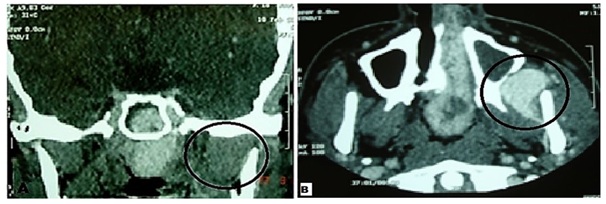
Figure 1A and 1B: Black circles in contrast-enhanced computed tomography (coronal and transverse sections, respectively) indicates HE localization in left side and structures envolved: pterygomaxillary fissure, nasal cavity, maxillary and sphenoid sinuses and upper limit near the greater wing of the sphenoid bone region.

Figure 2: Surgical specimen.
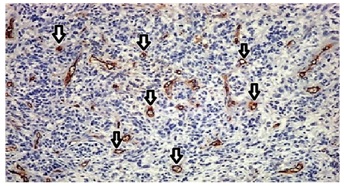
However, immunohistochemistry (CD34 marker) of tumor resection demonstrated that tumor was an EH. The presence of cellular atypia and mitotic frames are compatible with malignancy. There were no signs of neoplasia in bone tissue (Figure 3). Follow-up exams, quarterly periodical, were: nasopharyngolaryngoscopic and contrast-enhanced computed tomography, and there was no evidence of recurrence in three years.
DISCUSSION
CONCLUSION
REFERENCES
- Arcoverde LCA, Santos IC, Albuquerque BS, Romano S, Dias FL (2017) Hemangioendotelioma Epitelióide em cabeça e pescoço: Relato de caso tratado no Instituto Nacional de Câncer-RJ, Rio de Janeiro, Brazil.
- Demetris AJ, Minervini M, Raikow RB, Lee RG (1997) Hepatic epithelioid hemangioendothelioma: biological questions based on pattern of recurrence in an allograft and tumor immunophenotype. Am J Surg Pathol 21: 263-270.
- Ellis GL, Kratochvil FJ (1986) Epithelioid hemangioendothelioma of the head and neck: a clinicopathologic report of twelve cases. Oral Surg Oral Med Oral Pathol 61: 61-68.
- Chatelain B, Clairotte A, Euvrard E, Meyer C, Ricbourg B (2009) [Maxillary epithelioid hemangioendothelioma: case report and review of the literature]. Rev Stomatol Chir Maxillofac 110: 45-49.
- Fernandes AL, Ratilal B, Mafra M, Magalhaes C (2006) Aggressive Intracranial and Extra-Cranial Epithelioid Hemangioendothelioma: A Case Report and Review of the Literature. Neuropathology 26: 201-205.
- Lee JC, Lee JB, Wang SG, Kim HW (2006) Epithelioid haemangioendothelioma in the parapharyngeal space. J Laryngol Otol 120: 505-507.
- Lopes T, Clemente S, Feliciano A, Lourenço I, Costa A, et al. (2009) Hemangioendotelioma epitelióide do pulmão-Raridade, dificuldades diagnósticas e terapêutica. Revista Portuguesa de Pneumologia 6: 1167-1174.
- Mentzel T, Beham A, Calonje E, Katenkamp D, Fletcher CD (1997) Epithelioid hemangioendothelioma of skin and soft tissues: clinicopathologic and immunohistochemical study of 30 cases. Am J Surg Pathol 21: 363-374.
- de Oliveira CRGCM, de Camargo OP, Filho TEPB, Oliveira RP, Baptista AM (2001) Angiossarcoma epitelióide ósseo: relato de um caso, com estudo imuno-histoquímico. Acta Ortopédica Brasileira.
- http://www.lookfordiagnosis.com
- Santos CER, Correia MM, Pereira RS, Martins L, do Nascimento CM, et al. (2007) Hemangioendotelioma epitelióide hepático: relato de caso com tratamento multimodal. Revista Brasileira de Cancerologia 53: 217-222.
- Schoen FJ (1994) Vasos Sanguíneos. In: Robbins SL (ed.). Review of the book Patologia Estrutural e Funcional. Guanabara Koogan, Brazil.
- Weiss SW, Ishak KG, Dail DH, Sweet DE, Enzinger FM (1986) Epithelioid hemangioendothelioma and related lesions. Semin Diagn Pathol 3: 259-287.
- Stout AP (1943) Hemangio-endothelioma: a tumor of blood vessels featuring vascular endotheleal cells. Ann Surg 118: 445-464.
- Weiss SW, Enzinger FM (1982) Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer 50: 970-981.
Citation: Pascoal MBN, Chagas JFDS, Callegari FG, Ruba TDR, Leal MDOCD, et al. (2017) Epithelioid Hemangioendothelioma of Pterygomaxillary Fissure. J Otolaryng Head Neck Surg 3: 011.
Copyright: © 2017 Maria Beatriz Nogueira Pascoal, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

