
Evaluating the Relationship between FeNO and Pulmonary Function Tests in Asthmatic Patients
*Corresponding Author(s):
Sana EffendiLake Erie College Of Osteopathic Medicine, Pennsylvania, United States
Email:SEffendi99606@med.lecom.edu
Abstract
Background: Asthma is a chronic inflammatory airway disease in which assessment of both airway inflammation and lung function is essential for diagnosis and management. Pulmonary Function Tests (PFTs), particularly Forced Expiratory Volume in one second (FEV1), are widely used but may be costly and less accessible in some settings. Fraction of Exhaled Nitric Oxide (FeNO) has emerged as a potential non-invasive biomarker of airway inflammation, but its relationship to pulmonary function remains unclear.
Objective: To evaluate the relationship between FeNO levels and pulmonary function parameters in asthmatic patients.
Methods: A cross-sectional dataset of 31 asthmatic patients (ages 7-90 years) was analyzed. Patient demographics and potential confounders (smoking history, height, weight) were recorded. FeNO values (ppb) and FEV1 % predicted were compared using linear regression analysis. Statistical significance was defined as p < 0.05.
Results: Regression analysis showed no significant correlation between FeNO and FEV1 % predicted (p=0.937). No discernible linear trend was observed between airway inflammation and lung function.
Conclusion: FeNO is not a reliable indicator of spirometric indices or disease severity in asthma. While valuable as a marker of eosinophilic inflammation, FeNO should be interpreted alongside pulmonary function tests and clinical assessment. Larger, longitudinal studies stratified by asthma phenotype are needed to better clarify this relationship.
Keywords
Asthma; FeNO; FEV1; Fraction of exhaled nitric oxide; Pulmonary function tests; Spirometry
Introduction
Asthma is a chronic inflammatory airway disease characterized by variable airflow obstruction and bronchial hyperresponsiveness, affecting an estimated 262 million people worldwide [1]. Accurate assessment of airway inflammation and lung function is crucial for effective diagnosis and management. Pulmonary Function Tests (PFTs), including spirometry and Forced Expiratory Volume in one second (FEV1), are standard tools to assess airflow limitation [2]. However, PFTs are resource-intensive and not universally available.
Fraction of Exhaled Nitric Oxide (FeNO) is a simple, non-invasive biomarker of eosinophilic airway inflammation. Elevated FeNO levels reflect upregulation of Inducible Nitric Oxide Synthase (iNOS) in airway epithelial cells in response to inflammatory cytokines [3], and have been used to guide corticosteroid therapy and adherence monitoring [4,5]. Yet, the correlation between FeNO and pulmonary function remains variable. While some studies suggest moderate associations between FeNO and spirometric indices, others report inconsistent results [6,7].
This study aimed to evaluate the relationship between FeNO and pulmonary function in asthmatic patients to determine whether FeNO can reliably predict lung function impairment.
Methods
Study Design and Participants
A cross-sectional study was conducted using data from 31 patients with physician-confirmed asthma. Ages ranged from 7 to 90 years. Patient demographics and clinical characteristics, including smoking history, height, and weight, were recorded to account for potential confounders.
Measurements
- Fractional Exhaled Nitric Oxide (FeNO): Measured in parts per billion (ppb).
- Pulmonary Function: Assessed via FEV1 % predicted.
Statistical Analysis
Linear regression was performed to assess the relationship between FeNO and FEV1 % predicted. Statistical significance was defined as p < 0.05. Scatter plots with best-fit regression lines were used to illustrate results.
Results
The linear regression analysis showed no significant correlation between FeNO and FEV1 % predicted. The regression coefficient was non-significant (p=0.937), with no discernible linear trend (Figure 1).
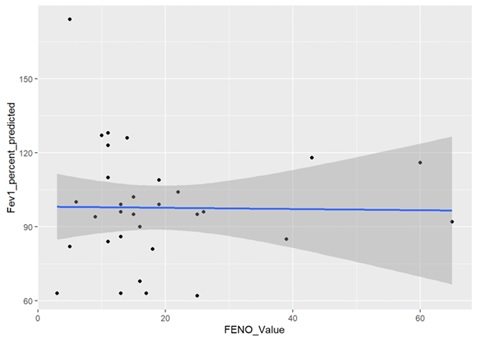 Figure 1: Relationship between FEV1 % predicted and FeNO values in 31 asthmatic patients.
Figure 1: Relationship between FEV1 % predicted and FeNO values in 31 asthmatic patients.
Discussion
This study demonstrated that FeNO is not a reliable surrogate for pulmonary function parameters in asthmatic patients. Although FeNO reflects eosinophilic airway inflammation, it does not correlate significantly with spirometric indices such as FEV1 % predicted.
Several factors may explain this discrepancy:
- FeNO Variability: Influenced by age, BMI, environmental exposures, and therapy adherence.
- Mechanistic Differences: FeNO reflects inflammation, whereas FEV1 measures airflow limitation. In non-eosinophilic asthma phenotypes, inflammation and obstruction may not align.
These findings align with previous studies indicating that FeNO should complement rather than replace spirometry in asthma assessment [5-7].
Limitations
- Small sample size reduced statistical power.
- Single cross-sectional design limited longitudinal insight.
- Rural cohort may reduce generalizability.
Clinical Implications
Asthma management should integrate both inflammatory markers and functional measures. FeNO may guide anti-inflammatory therapy, but spirometry remains necessary for evaluating airflow limitation.
Conclusion
FeNO is a useful biomarker of eosinophilic airway inflammation but not a reliable predictor of pulmonary function or asthma severity. A comprehensive approach to asthma management requires both FeNO and pulmonary function testing.
Future Directions
Future studies should include larger cohorts, adopt longitudinal designs, and stratify patients by asthma phenotype (eosinophilic vs. neutrophilic) to clarify the clinical utility of FeNO relative to spirometry.
References
- World Health Organization (2024) World Health Organization, Geneva, Switzerland.
- Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, et (2005) Interpretative strategies for lung function tests. Eur Respir J 26: 948-968.
- Barnes PJ (1995) Nitric oxide and airway Ann Med 27: 389-393.
- Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, et al. (2011) An official ATS clinical practice guideline: Interpretation of exhaled nitric oxide levels (FeNO) for clinical Am J Respir Crit Care Med 184: 602-615.
- Smith AD, Cowan JO, Filsell S, McLachlan C, Monti-Sheehan G, et (2004) Diagnosing asthma: Comparisons between exhaled nitric oxide measurements and conventional tests. Am J Respir Crit Care Med 169: 473-478.
- Rao DR, Phipatanakul W (2016) An overview of fractional exhaled nitric oxide and children with asthma. Expert Rev Clin Immunol 12: 521-530.
- Shaw DE, Berry MA, Thomas M, Green RH, Brightling CE, et (2007) The use of exhaled nitric oxide to guide asthma management: A randomized controlled trial. Am J Respir Crit Care Med 176: 231-237.
Citation: Effendi S, Tulsi Patel T, Nasir A (2025) Evaluating the Relationship between FeNO and Pulmonary Function Tests in Asthmatic Patients. HSOA J Community Med Public Health Care 12: 167.
Copyright: © 2025 Sana Effendi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

