
Evaluating two Postural Change Methods for the Positional Dynamic Measurement of the Diameters of the Michaelis Sacral Rhomboid Area
*Corresponding Author(s):
Marco SiccardiDepartment Of Obstetrics And Gynecology, San Paolo Hospital, Savona, Italy
Tel:+39 0198386311,
Email:marcosiccardi66@gmail.com
Abstract
Introduction: The diagnosis of “contracted pelvis” is still a challenge in the obstetric field. The early diagnosis could avoid neonatal and maternal complications resulting from suffering caused by prolonged labour and operative delivery, especially in countries with low socio-sanitary content. Radiological pelvimetry has shown that the endopelvic space is modified according to the posture that the subject assumes: between the prone position, the “four supports” and in the squat, changes of internal diameters have been highlighted. Our study would like to investigate the possibility of highlighting the same type of modifications through external pelvimetry.
Methods: Thirty healthy non-pregnant women were recruited. The transverse and longitudinal diameters of the Michaelis area were measured with two different dynamic methods to change the 3 postures in which to perform the measurements: upright position, 90° position of the hip, squat position. The measurements were taken with a suitable patented instrument.
Results: With both methods the diameters of the sacral area undergo an increase in measurements, suggesting a corresponding increase in the internal pelvic diameters with the passage from the standing station to the 90° position and the squat position.
Conclusion: The dynamic postural method of external pelvimetry, suitably adapted to clinical needs, demonstrates that it is possible to evaluate the range of pelvic movement with the shifting position.
INTRODUCTION
Dystocia is still one of the major causes of complicated delivery and maternal and neonatal morbidity [1,2]. Among the causes of dystocia, the most difficult to predict and prevent is the so-called “contracted pelvis” which does not allow the commitment of the part presented within the pelvic excavation or prevents its progression with possibly disastrous consequences for the woman and the fetus. A screening or diagnostic method addressed to the contracted pelvis would improve the quality of childbirth for mothers and babies. In obstetrics manuals and osteopathic learning courses [3-5], it is suggested to evaluate the shape and the postural changes of the area of the sacral rhombus of Michaelis from the upright to the squat position: it would relate the space in the pelvis for a safe childbirth. They generically stated that, by changing the posture, the shape and size of the sacral rhombus change when the pelvis is free to expand, and the sacral area widens progressively from the up right to the squat position. Despite such affirmations, the postures were not well described and standardized, a device to quantify and objectify the changes in the measures of the diameters was not developed, there do not normality reference curves, no correlation with the obstetric outcomes was statistically calculated.
The rationale of the present study comes from researches performed by MR and optoelectronic devices in pregnant and non-pregnant women [6-9]. They showed an increase in transverse internal diameters of the pelvis and a variation in the lumbosacral angle with the degree of flexion of the hip joints. Our hypothesis starts from the evidence that the pelvis is a whole: changing the position in the three-dimensional space of one of the iliac points applies to the movement of all the other points (Figure 1) [10]. If significant variations of the internal pelvic diameters have been demonstrated on MR, the same variations should also be found for the external pelvic diameters [10]. The human hand has fantastic proprioceptive properties and can manipulate small objects with great precision [11], manual medicine operators are trained to evaluate very small, almost non-quantifiable ranges of motion, while the expected range of motion for this study is around 5mm [6,12]. The few studies present in the literature have used two different postural procedures that have been used in the present study [6-8]. The present study aims to verify the precision, reliability and concordance of the quantitative measurement of the transverse and longitudinal diameters of the Michaelis area in the upright position, in the position with the hip joints at 90° and in the squat position; to test the correspondence of the measurements in the different positions. This is a preliminary study to check and choose the procedure for changing the positions, addressed to the possible use of the measurement method in women in the late third trimester of pregnancy.
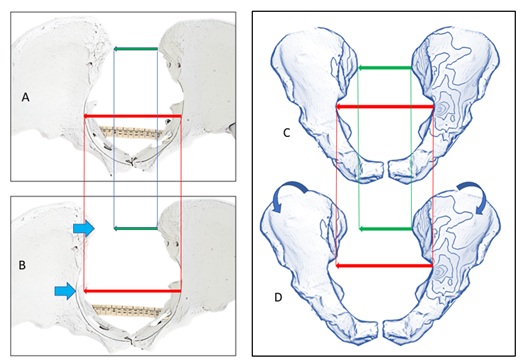 Figure 1: A and B osseous model of the pelvis. C and D reconstructed model of the pelvis. Changes of the width in internal diameter (pelvic inlet, red arrow) through the iliac anteriorly rotated (B and D) correspond changes in external pelvic diameter (transverse diameter of the Michaelis sacral rhomboid area, green arrows).
Figure 1: A and B osseous model of the pelvis. C and D reconstructed model of the pelvis. Changes of the width in internal diameter (pelvic inlet, red arrow) through the iliac anteriorly rotated (B and D) correspond changes in external pelvic diameter (transverse diameter of the Michaelis sacral rhomboid area, green arrows).
METHODS
Thirty healthy non-pregnant women were recruited, and the study protocol and its aims were explained: all of them expressed their informed consent. Only nulliparous subjects who did not report abdominal, pelvic or vertebral surgical interventions, did not suffer from lumbopelvic pains and did not have abdominal-pelvic diseases at the clinical evaluation were accepted. The study was conducted in conformity to the Helsinki declaration. The study protocol was defined by the first author who refers to the Obstetrics Department of “San Paolo” Hospital of Savona, Italy (board approval number: 119933-2019). The number of subjects recruited exceeds the minimum suggested of twelve/fifteen subjects for the evaluation trials in biomechanical studies concerning the significant effect on statistical power [13]. Two different ways of obtaining the three different positions were compared, using a suitable CE patented measuring instrument: the “Bone-Meter Kit” - BMK - Metrica SpA, Milano, Italy (Figure 2), which has an accuracy of 0.2mm and a resolution of 0.1mm [14].
 Figure 2: The “Bone-Meter Kit”, Metrica SpA, Milan, Italy, EU.
Figure 2: The “Bone-Meter Kit”, Metrica SpA, Milan, Italy, EU.
First postural method (“standing positions”, Sp) (Figure 3A-3C). Sp1: patients start on the standing position with feet parallel to the width of the hips. Extended lower limbs. Pelvis, spine and head in the neutral position as for the standard measurement of body height. Arms along the sides. Sp2: to bring the hip joints “at 90°”, the subjects perform flexion of the entire spine and pelvis around the hips, resting the arms and torso on the examination table placed at a suitable distance and maintaining the knees in full extension. Sp3: bending the lower limbs, keeping the heels resting on the ground, they move to the “squat” position. The arms and hands resting on the examination table can help maintain balance.
Second postural method (“kneeling positions”, Kp) (Figure 3D-3F). Kp1 (upright kneeling position): the upright position as in the previous method, with the difference that the support on the ground occurs through the knees, with the ground tibia flexed to 90° on the femur. Kp2: flexion of the hip joints “at 90°” using the position on the “four supports” (“all four”): the patient brings the weight forward resting her hands on the. Kp3: finally, bringing the ischial tuberosities towards the heels and the torso towards the supporting surface, subjects pass to the position of “squat” on the knees (“kneeling squat”).
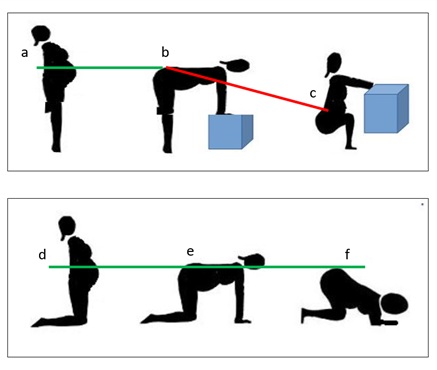 Figure 3: First postural method: a, b, c. Second postural method: d, e, f.
Figure 3: First postural method: a, b, c. Second postural method: d, e, f.
A: sp1; B: sp2; C: sp3; D: kp1; E: kp2; F: kp3
All thirty subjects performed both postural protocols, while the operator took measurements of the two diameters of the pelvic sacral area in all six positions. Procedure: (0) the operator shows both protocols “standing” and “kneeling”; (1 and 2) the subject performs the two protocols while the operator keeps the contact of the fingers on the posterior superior ischial spines to be able to correct movements and positions; (3 and 4) the subject performs the “standing” protocol twice, while the operator first measures the transverse diameter and then the longitudinal diameter of the diamond of Michaelis in the three positions; (5 and 6) the subject then executes the “kneeling” protocol twice while the operator measures the transverse and longitudinal diameters of the Michaelis diamond in the three positions. In the end, the subjects were asked to choose one of the two postural procedures, based on simplicity and ease of execution.
The measurements of the study refer to the transverse and longitudinal diameters of the Michaelis rhombus [14-16] (Figure 4). The transverse diameter is subtended by the two Posterior Superior Ischial Spines (PSIS). The longitudinal diameter has as extremes: the posterior border of the spinous process of the fifth Lumbar vertebra (L5) and the medial union point of the insertions of the right and left gluteus muscles, which corresponds to the sacral hiatus, at the fourth-fifth sacral segment. The study protocol was chosen to have only one variable at a time to study. A single evaluation was used for each measurement and not the average of several evaluations, to better highlight the measurement discrepancies, and a single operator was used to minimize the variability of inter-individual manual sensitivity [17-18]. The position of the operator was behind the participants and on the opposite side from his dominant hand. The contact was through the thumbs placed on the SIPS and the other fingers on the iliac crests, to be stable and supportive with both iliac (Figure 5). By maintaining continuous contact, the operator’s hands followed the pelvic movement during the postural changes. The operator kept the eyes closed while the subject moving, to concentrate the perception of the hands firmly in contact with the anatomical points to be measured [14]. He started from the measurements in the “upright” station (Sp1 and Kp1), then moved to the “90°” position (Sp2 and Kp2) to end in “squat” position (Sp3 and Kp3). After that, the operator keeps contact with the two-second fingers on L5 and S5 proceeding similarly, resembling the Schober’s test for the clinical evaluation the range of motion of the lumbar-sacral joint flexion [19].
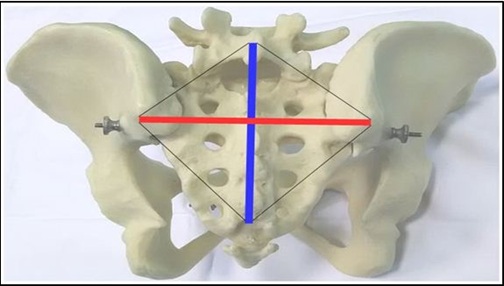 Figure 4: The sacral rhomboid area of Michaelis. Red line: the transverse diameter. Blue line: the longitudinal diameter.
Figure 4: The sacral rhomboid area of Michaelis. Red line: the transverse diameter. Blue line: the longitudinal diameter.
 Figure 5: The BMK handhold. Patient in “hands-to-knees” position.
Figure 5: The BMK handhold. Patient in “hands-to-knees” position.
Participants were asked to give a preference between the two postural methods of the position change with three possible answers: no preference, preference for the standing protocol, preference for the kneeling protocol.
Statistical analysis
The OpenOffice spreadsheet was used to record the measurements (Apache OpenOffice 4.1.2 Copyright 2015 The Apache Software Foundation. Http://www.openoffice.org). Data are expressed in millimeters and reported as mean, Standard Deviation (SD), Standard Error of the Mean (SEM) and 95% Confidence Interval (95% CI). The calculation of Intraclass Correlation Coefficients (ICC), the t-test for repeated measurements (paired t-test) was performed with the dedicated statistical software (Statstodo Trading PTY, Ltd, Brisbane, Queensland, Australia; http://www.statstodo.com). The reference table for the assessment of the ICC is: 0.0-0.2 indicates poor agreement: 0.3-0.4 indicates modest agreement; 0.5-0.6 indicates good agreement; 0.7-0.8 indicates strong concordance; >0.8 indicates an almost perfect concordance. ICC values higher than 0.70 were considered statistically significant. For the paired Student t-test, the value of p <0.05 was considered significant.
RESULTS
Each subject participating in the study performed the 2 postural protocols 3 times, each protocol included the passage in 3 different postures: a total of 18 movements by the patient and 12 measurements from each patient by the operator. The operator recorded a total of 360 measurements. The participants were aged (mean±SD) of 34.6±6.5 years, a height of 164.7±5.5 centimeters and a weight of 57.8±9.1 kilograms. Data from 29 subjects were analyzed (an exclusion due to data transcription error). Between the two methods of shifting positions, the standing method and the kneeling method, a nearly perfect correlation between the measurements was shown. Measurements vary considerably from the upright position to the squat posture, passing through the intermediate position (Table 1). All the measurements taken in the starting position are smaller than the intermediate and squat positions. For the transversal diameter, the absolute value is lower in the squat position than in the intermediate position (Table 1), showing agreement between the methods. The Range of Movement (ROM) is statistically significant in the transition between p1 and p2 positions and between p1 and p3 positions, for both methods. There was no statistical difference between p3-p2 positions, excepted for the Sp3-Sp2 of the transverse diameter (Table 2). The ICC is almost perfect concerning all the total and single absolute measures, except for the p2 of the longitudinal diameter (Table 1). While the total ICC of the ROMs reaches the significant statistical value, it is not for p2-p1 and p3-p2 shifting positions of the transverse diameter (Table 2).
|
|
“Upright” position (1) |
“hips 90°” position (2) |
“Squat” position (3) |
|||
|
|
Standing |
Kneeling |
Standing |
Kneeling |
Standing |
Kneeling |
|
Transverse diameter: Mean (SD) |
108.4 (11.7) |
108.4 (11.6) |
115 (14.9) |
114.3 (12.2) |
112.5 (15) |
112.7 (13.8) |
|
95% CI |
104.1-112.7 |
104.2-112.6 |
109.1-120.8 |
109.8-118.7 |
107-118 |
107.6-117.7 |
|
ICC |
0.98 |
0.94 |
0.95 |
|||
|
Longitudinal diamet: Mean (SD) |
138.8 (22.9) |
142.4 (23) |
144 (7.2) |
150.6 (8.0) |
158.3 (15.5) |
160.8 (14.6) |
|
95% CI |
127.2-150.3 |
130.8-154.1 |
135.8-152.1 |
141.5-159.7 |
145.7-170.6 |
149.1-172.5 |
|
ICC |
0.93 |
0.69 |
0.94 |
|||
Table 1: Measurements of the transverse and longitudinal diameters of the Michaelis sacral area in the three positions of the two methods. The data, expressed as absolute measurements in millimetres, report the average, the Standard Deviation (SD) and the 95% Confidence Interval (95% IC). For each position, the values of each methods (“standing” and “kneeling”) are written in pairs and the Intraclass Correlation Coefficient (ICC) of their agreement is reported.
|
Transverse diameter |
Sp2-Sp1 |
Kp2-Kp1 |
Sp3-Sp1 |
Kp3-Kp1 |
Sp3-Sp2 |
Kp3-Kp2 |
|
Mean (SEM) |
7.4 (1.05) |
5.8 (1.6) |
4.1 (1.2) |
4.2 (1.1) |
-2.8 (0.9) |
-1.5 (0.8) |
|
95% CI |
5.2-9.6 |
4.5-7.1 |
1.5-6.6 |
1.8-6.6 |
0.8-4.8 |
-0.3-3.3 |
|
p-value |
<0.0001 |
<0.0001 |
0.002 |
0.001 |
0.008 |
0.06 |
|
ICC° |
0.58 |
0.79 |
0.64 |
|||
°Total ICC Standing-Kneeling: 0.80.
|
Longitudinal diameter |
Sp2-Sp1 |
Kp2-Kp1 |
Sp3-Sp1 |
Kp3-Kp1 |
Sp3-Sp2 |
Kp3-Kp2 |
|
Mean (SEM) |
30.3 (3.06) |
30.3 (3.1) |
42.7 (3.3) |
36.4 (2.9) |
13.1 (5.4) |
5.5 (1.2) |
|
95% CI |
22.9-38.7 |
23.4-37.1 |
35.4-49.5 |
30.2-42.6 |
-0.8-27.1 |
-2.8-8.2 |
|
p-value |
0.0002 |
<0.0001 |
<0.0001 |
<0.0001 |
NS |
NS |
|
ICC* |
0.94 |
0.91 |
0.85 |
|||
*Total ICC Standing-Kneeling: 0.91.
Table 2: The Paired t-test of the difference between the measurements in the different positions to evaluate the Range Of Motion (ROM). Data expressed in millimetres as mean, Standard Error of the Mean (SEM) and the 95% Confidence Interval (95% CI).
Sp: standing position; Kp: kneeling position; 1: “upright” position; 2: “hips 90°” position; 3: “squat” position.
Participants were asked to give a preference between the two postural methods of the position change. There were three possible answers (no preference, preference for the standing or the kneeling protocol), so assuming a theoretical equality percentage of the judgments (33.3%), the evaluations were the following: “no preference” 4/30 (13.3%; 95% CI 5.3-29.6), “preference for the standing protocol” 0/30 (0.0%; 95% CI 0.0-11.3), “preference for the kneeling protocol” 26/30 (86.6%; 95% CI 70.3-94.6; p <0.0001).
DISCUSSION
The interest in pelvimetry as a screening test for operative delivery dates back several centuries [20]: the contracted pelvis is still one of the main causes of complicated childbirth and maternal and fetal morbidity. From Baudelocque to radiology, the external and internal pelvimetry considered the rough static pelvic diameters, not considering their changes in shifting position. As far as we know, no studies were performed to evaluate the dynamic modification of the shape and diameters of the sacral area of Michaelis and the external pelvic diameters. The two postural methods used in the present report were extrapolated from the few previous imaging studies on the internal pelvic diameters [6,7] and the clinical practice [8]. Studies that evaluated the postural changes of the diameters of internal pelvimetry using imaging methods [6,7] indicate an adaptation in the width of the transverse diameters of the pelvis in shifting position. The distance between the PSIS is the transverse diameter of the sacral rhombus and corresponds to the pelvic inlet in obstetric external pelvimetry [21]. In a previous study, the likelihood of a linear correlation between the internal and external pelvic coordinates was suggested [10]. Our study shows that the evaluation of the diameters of the sacral rhomboid diameters can also be performed using a clinical method with a simple tool, using the sensitivity of the operator's hands and the change in the posture of the subject to be examined. Concerning the transverse diameter, the study agrees with the literature data obtained with radiological methods [6,7]: this lays the foundations to go further performing the test in pregnant women to verify the validity and accuracy of the test as a screening test for the obstetric outcomes [12].
The obstetric external pelvimetry evaluation was performed in standing position [20], so in the present study, the erect starting positions are the reference position, as the supine position was for the radiological studies [6,7]. The choice of the squat position was dictated by the obstetric, postural, radiological and osteopathic literature because it is the traditional position of the expulsive phase of birth. A traditional saying of Jamaican midwives states that a woman has to open her back before giving birth [22]. The “back openness” could be interpreted as a widening of the space between the iliac at the level of the PSIS (the transversal diameter of the Michaelis area) together with the contra-nutation of the sacral base, which moves posteriorly flattening the lumbosacral angle and flexing the lower lumbar [23,24]. In biomechanics, the sacral base moves posteriorly and the lumbar spine moves into flexion shifting in the squat position while the promontory of the sacrum becomes less prominent anteriorly. The degree of the process corresponds to the progressive increase in the distance between the spinous process of the fifth lumbar vertebra and the sacral apex: that is the longitudinal diameter of the sacral area [5].
Some studies stated the greater importance of some pelvic diameters as compared to others in dystocia, and the largest diameter is measured in the intermediate position between supine and squat [8,24,25]. We chose to introduce these kinds of “90-degree hip joints” positions for some reasons: they are the steadiest and easiest positions to maintain for the time necessary to measure the diameters. The clinical experience showed that during the dilation phase of labour the giving-birth woman is often positioned with the trunk at 90° and the knees extended to withstand the pain of contractions (Figure 3B). The birth itself is carried out in the “all-four” position (Figure 3E), or on the Dutch stool or in support [26]. The results of our study confirm that the hip joints flexion at 90° with few degree abduction [8,26] and not the squat position favors the greater transverse diameter of the sacral area (corresponding to the pelvic inlet), in which the descent and the relationship of the child’s head to the maternal pelvis happened. The longitudinal diameter of the Michaelis area, related to the lumbar-sacral flexion [19] and the angle of the sacral promontory, did not statistically differ between the intermediate and the squat position. The present report shows that the position with the hip joints at 90° is adequate to evaluate the “back openness” [22]: in agreement with the recent optoelectronic studies [8,9,23-25].
The present study suggests that the correlation between the measurements obtained by the two methods is adequate, confirming the good precision of the instrument and the adequate reproducibility of the methods. This study shows that the two methods of postural change are similar, superimposable, regarding the absolute measures. Nonetheless, the correlation between methods concerning the ROM is not so perfect: one of the postural methods must be chosen for clinical purpose. The non-pregnant subjects examined gave a clear preference for the “kneeling” method, which was easier to perform. The operator can easier follow the movements of the subject’s pelvis in the kneeling position: the pelvis remains at the same level from the ground, more steadily in the three-dimensional space than the standing posture method (Figure 3). The definition of a reproducible methodology for all patients is fundamental to perform a preventive/diagnostic test [27], and the Evidence-Based Medicine stated that the compliance of the patient and the practical experience of the operator must be considered [28]. Considering the possible use for pregnant women in their third trimester or at term, the “kneeling posture” method of shifting positions is a reliable, reproducible, safe system that can be performed more easily than the “standing posture” method, either when they execute the test or when move back to the upright position from the squat position at the end of the procedure [14]. To evaluate the range of movement of the transverse diameter of the pelvic outlet, defined by the two ischial tuberosities, is feasible in the kneeling positions not in the standing: the “kneeling” for shifting positions could be adopted to evaluate and measure the ROM of all the obstetric external pelvimetry diameters [14].
In previous clinical reports, the transverse diameter of the Michaelis’ sacral area [15,16], and the range of lateral movement of the superior posterior iliac spines [12], are suggested to be related to the mode of delivery indicating a possible role as a predictive test during the third trimester of pregnancy for the risk of operative delivery.
CONCLUSION
The present report in non-pregnant women confirms the radiological studies in pregnant and non-pregnant women that demonstrated the different room in the pelvis in different body positions. It shows the capability to measure the changes of the external pelvic diameters using a clinical approach on the rhomboid area of Michaelis. It shows the widest transverse diameter of the sacral area in the intermediate positions, not in the squat positions, and concerning the longitudinal diameter similar degree of lumbosacral joint flexion (the flattest angle of the sacral promontory) in the intermediate and squat positions. Further studies need to investigate the method during pregnancy and to highlight the entire clinical potential of the traditional obstetric external pelvimetry bio-dynamically evaluated through the range of motion during shifting positions.
REFERENCES
- Drennan KJ, Blackwell S, Sokol RJ (2008) Abnormal Labor: Diagnosis and Management. Glob libr women’s med.
- Aliijahan R, Kordi M (2014) Risk Factors of Dystocia in Nulliparous Women. Iran J Med Sci 39: 254-260.
- Spandrio R (2014) Il canale del parto. In: Spandrio R, Regalia A, Bestetti G (eds.). Fisiologia della nascita: Dai prodromi al post partum. Carocci Faber Professioni sanitarie, Roma, Italy.
- Von Elke H (2006) Effects of Osteopathic work to Mother and Child regarding Foetal heart rate, Uterine contractions, Lumbosacral mobility, and objective Parameters of Delivery [Dissertation]. Masters' thesis Wiener Schule für Osteopathie, Wien, Austria.
- Aspalter W (2008) Can back pain caused by symptom-giving sacroiliac joint relaxation during pregnancy be reduced by applying osteopathic treatment? [Dissertation]. Masters' thesis Wiener Schule für Osteopathie, Wien, Austria.
- Reitter A, Daviss BA, Bisits A, Schollenberger A, Vogl T, et al. (2014) Does pregnancy and/or shifting positions create more room in a woman's pelvis? Am J Obstet Gynecol 211: 662.
- Michel SC, Rake A, Treiber K, Seifert B, Chaoui R, et al. (2002) MR obstetric pelvimetry: Effect of birthing position on pelvic bony dimensions. AJR Am J Roentgenol 179: 1063-1067.
- Desseauve D, Pierre F, Gachon B, Decatoire A, Lacouture P, et al. (2017) New approaches for assessing childbirth positions. J Gynecol Obstet Hum Reprod 46: 189-195.
- Gleason RL Jr, Yigeremu M, Debebe T, Teklu S, Zewdeneh D, et al. (2018) A safe, low-cost, easy-to-use 3D camera platform to assess risk of obstructed labor due to cephalopelvic disproportion. PLoS One 13: 0203865.
- Lalonde NM, Dansereau J, Aissaoui R, Pauget P, Cinquin P (2003) Differences between pelvic skin and bone landmark identification in different seated positions on spinal-cord injured subjects. IEEE Trans Biomed Eng 50: 958-966.
- Abraham L, Urru A, Normani N, Wilk MP, Walsh M, et al. (2018) Hand Tracking and Gesture Recognition Using Lensless Smart Sensors. Sensors (Basel) 18: 2834.
- Siccardi M, Valle C, Di Matteo F, Fiorenza P, et al. (2017) How osteopathy could help obstetrics in diagnosis and therapy, preliminary report about safety and efficacy of osteopathy in an obstetrics department in Italy. J Perinat Med 45: 308-309.
- Forrester SE (2015) Selecting the number of trials in experimental biomechanics studies. International Biomechanics 2: 62-72.
- Siccardi M, Valle C, Di Matteo F, Angius V (2019) A Postural Approach to the Pelvic Diameters of Obstetrics: The Dynamic External Pelvimetry Test. Cureus 11: 6111.
- Kordi M, Alijahan R (2012) The diagnostic accuracy of external pelvimetry to predict dystocia in nulliparous women. Zahedan J Res Med Sci 14: 36-38.
- Bansal S, Guleria K, Agarwal N (2011) Evaluation of sacral rhomboid dimensions to predict contracted pelvis: A pilot study of Indian primigravidae. J Obstet Gynaecol India 61: 523-527.
- Squara P, Imhoff M, Cecconi M (2015) Metrology in medicine: From measurements to decision, with specific reference to anesthesia and intensive care. Anesth Analg 120: 66-75.
- Vickers AJ (2003) How many repeated measures in repeated measures designs? Statistical issues for comparative trials. BMC Med Res Methodol 3.
- Tousignant M, Poulin L, Marchand S, Viau A, Place C (2005) The Modified-Modified Schober Test for range of motion assessment of lumbar flexion in patients with low back pain: A study of criterion validity, intra- and inter-rater reliability and minimum metrically detectable change. Disabil Rehabil 27: 553-559.
- Tarnier S, Budin P (1889) Traité de l'art des accouchements, Tome 3 [Book in French]. Steinheil Libraire, Paris, France.
- Kakoma JBSZ, Kalibushi J, Ramazani RK (2010) Pelvis and anthropometric study in Rwandan women at prenatal care settings in the southern province of Rwandan (Huye District). Rwanda Medical Journal 69: 13-25.
- Sutton J (2002) The rhombus of Michaelis. A key to normal birth, or the poor cousin of the RCT? Interview by Sara Wickham. Pract Midwife 5: 22-23.
- Hemmerich A, Diesbourg T, Dumas GA (2018) Development and validation of a computational model for understanding the effects of an upright birthing position on the female pelvis. J Biomech 77: 99-106.
- Hemmerich A, Bandrowska T, Dumas GA (2019) The effects of squatting while pregnant on pelvic dimensions: A computational simulation to understand childbirth. J Biomech 87: 64-74.
- Desseauve D, Fradet L, Lacouture P, Pierre F (2019) Is there an impact of feet position on squatting birth position? An innovative biomechanical pilot study. BMC Pregnancy and Childbirth 19.
- Huang J, Zang Y, Ren LH, Li F-J, Lu HL (2019) A review and comparison of common maternal positions during the second-stage of labor. Int J Nurs Sci 6: 460-467.
- Spörri S, Gyr T, Schollerer A, Werlen S, Schneider H (1994) [Methods, techniques and assessment criteria in obstetric pelvimetry]. Z Geburtshilfe Perinatol 198: 37-46.
- Fernandez A, Sturmberg J, Lukersmith S, Madden R, Torkfar G, et al. (2015) Evidence-based medicine: Is it a bridge too far? Health Res Policy Syst 13: 66.
Citation: Siccardi M, Valle C, Di Matteo F, Angius V (2020) Evaluating two Postural Change Methods for the Positional Dynamic Measurement of the Diameters of the Michaelis Sacral Rhomboid Area. J Reprod Med Gynecol Obstet 5: 035.
Copyright: © 2020 Marco Siccardi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

