
Evaluation of Energy Expenditure of Obese Subjects by Bioelectric Method
*Corresponding Author(s):
Ghouini APhysiology Laboratory Faculty Of Medicine, Blida 1 University, Ouled Yaïch, Algeria
Tel:+ 213 773839184,
Email:ghouinia@yahoo.fr
Abstract
Obesity is an inflation of the fatty tissue with harmful repercussions on health. The excess fat mass results from the imbalance of the energy balance strongly determined by the level of basal metabolism. The impedancemetric bioelectric method in routine clinical practice for estimating the energy expenditure associated with the measurement of body composition has proven to be a very accessible technique for monitoring obese patients.
Keywords
Energy metabolism; Impedancemetry; Obesity
INTRODUCTION
Obesity is defined by an excess of fat mass with harmful health effects; the increase in weight is made up on average for 2/3 by the fat mass and 1/3 by the lean mass. The proportion of adipose tissue is thus increased in overweight.
It is well accepted that the slightly hydrophilic adipose tissue has a higher resistance to the passage of an electric current compared to that measured through the water compartment rich in electrolytes [1]. Furthermore, there is a relationship between body composition and basal metabolism, a major determinant of energy metabolism [2].
Within the framework of the measurement of the energy expenditure of the obese subject, we carried out the measurement of the basic metabolism by bioelectric impedancemetry,
PATIENTS AND METHODS
Our study is part of the descriptive cross-sectional observational studies.
Patients
The subjects of the number of 172 recruited during the period from January 2014 to May 2017 are adults of both sexes, normal-weight or overweight.
- • Inclusion criteria: subjects whose body mass index (BMI = weight in kg / m2) is above 18.5 kg / m2, subjects of 2 sexes aged 17 - 65 years
- • Criteria for non-inclusion: lean, malnourished subjects, subjects suffering from endocrine disorders, children and subjects aged over 65 years.
Material
- • Bioelectric impedance measurement: in our protocols, we used a multifrequency impedance measurement such as "Bodystat Quadscan 4000".
Methods
Measurement of body composition and energy expenditure:
Bioelectrical impedance measurement: among non-anthropometric methods, it is certainly the one that is most used because it is the most easily accessible. There are several types of apparatus ranging from general public and inexpensive devices for analyzing the fat mass on a subject in a standing position, to more sophisticated devices, comprising several electrodes, used on a patient in decubitus and which allow segmental analyzes. of body composition. It is a non-invasive technique based on resistance to the passage of a low intensity electric current through the body (fatty and non-fatty tissue). From the total volume of body water which is estimated as a function of the conductance (impedance) of the electric current through the water compartment rich in electrolytes, the quantity of lean mass can be deduced knowing that it consists mainly of water: fat mass simply corresponds to a difference between body mass and lean mass [3] (Figure 1).

Figure 1: Impedancemeter: Bodystat Quadscan 4000
Impedancemetry measurements are taken on supine subjects in the morning on an empty stomach since certain factors can modify the amount of intracellular water such as diet and exercise. Patients being at rest when filling in the questionnaire. 5 -10 min of rest are necessary for optimal distribution of body fluids.
Two electrodes are placed at the level of the hand and two others at the level of the homolateral foot. Then the anthropometric measurements are saved in the device and the measurement is immediately carried out. The examination lasts a total of 4-5 min [4].
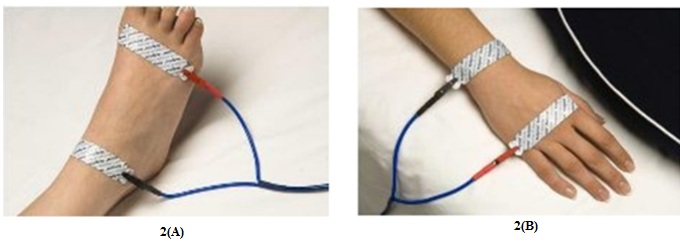 Figure 2: Installation of electrodes.
Figure 2: Installation of electrodes.
The electrodes at the level of the 2(A): On the dorsal side of the ankle, between the malleolus inside and outside; one finger below the head of the third metatarsal. 2(B): On the dorsal side of the wrist between the styloid process of the radius and ulna- and one finger below the head of the third metacarpal.
After entering all the patient's data into the device: gender, age, height, weight, waist measurement, hip measurement, activity level, a full body analysis is displayed.
- • Body fat, in percentage and absolute;
- • Lean mass, in percentage and in absolute;
- • The total weight;
- • Body water, in percentage and in absolute;
- • Lean dry mass;
- • Basic metabolism (BM);
- • Bm/weight;
- • Waist-to-hip ratio;
- • Estimated energy needs;
- • BMI;
- • The fat body mass index (BFMI),
- • The lean mass index.
The parameters on which our study was based include: age, sex, BMI, body fat in absolute, lean mass in absolute, BMR and estimated energy needs.
Statistic study
The Statistical Package of Social Science (SPSS 17.0) software was used for the statistical study. To judge the statistical significance of the parameters, we used the Student test (t). The 95% confidence interval represents the interval that contains the true value of the parameter with a 5% risk of error. The parameters are presented as averages.
For the comparison of the means, the result is given in the form of a p (statistical significance). If p ≥ 0.05: the comparison is not significant, if p < 0.05: the result is significant and if p = 0.001: the result is highly significant (Figures 3-7).
RESULTS
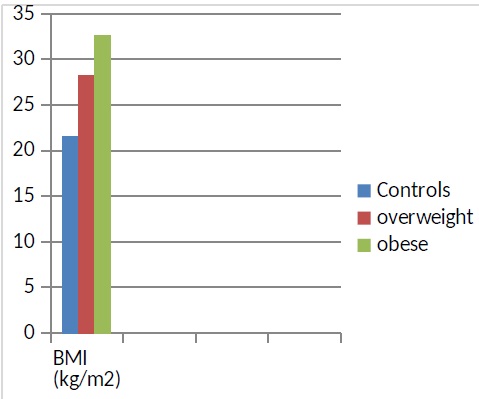 Figure 3: BMI comparison between the 3 groups.
Figure 3: BMI comparison between the 3 groups.
- Group 1 (controls): 44 normal subjects with a BMI between 18.5 and 25 kg / m2 with an average of 22 kg / m2
- Group 2: 44 overweight subjects with a BMI between 25 and 30 kg / m2 with an average of 28 kg / m2
- Group 3: 44 obese subjects whose BMI is ≥ 30 kg / m2 with an average of 35 kg / m2
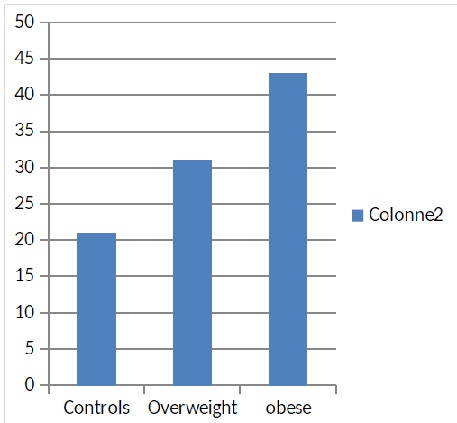 Figure 4: Body composition in the 3 groups.
Figure 4: Body composition in the 3 groups.
The average fat mass of the obese subject is the largest compared to that of the control and overweight subject. s.
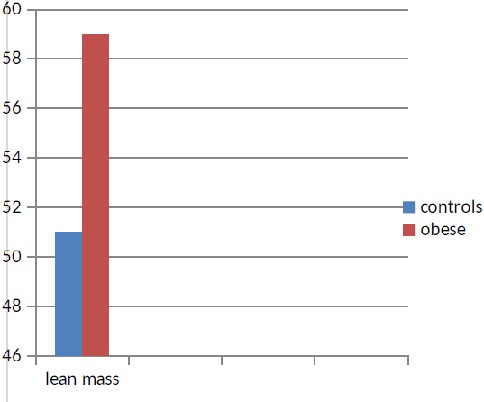 Figure 5: Comparison of the proportion of lean body mass between controls and obese subjects; it turns out that obese subjects have an expansion in lean mass and in our protocol, it appears higher than that of the normal weight subject (P <0.001).
Figure 5: Comparison of the proportion of lean body mass between controls and obese subjects; it turns out that obese subjects have an expansion in lean mass and in our protocol, it appears higher than that of the normal weight subject (P <0.001).
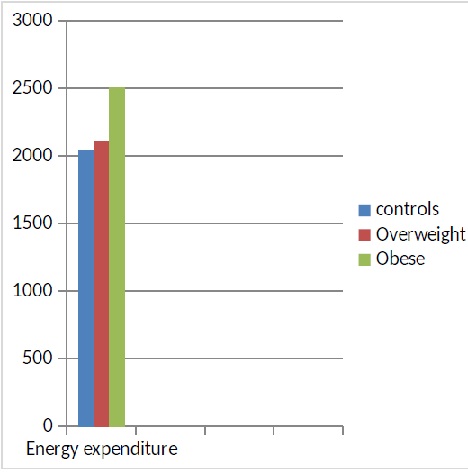 Figure 6: Energy expenditure (kcal / d) in the 3 groups of subjects: there is no significant difference between the controls and the overweight subjects while the energy expenditure of obese subjects is significantly higher than that of the other 2 groups.
Figure 6: Energy expenditure (kcal / d) in the 3 groups of subjects: there is no significant difference between the controls and the overweight subjects while the energy expenditure of obese subjects is significantly higher than that of the other 2 groups.
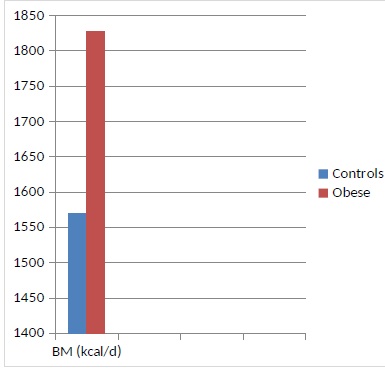 Figure 7: Comparison of basal energy expenditure between controls and obese subjects; as can be seen, the basal metabolism (BM) of the obese subject is higher than that of the normal-weight subjects (P <0.001).
Figure 7: Comparison of basal energy expenditure between controls and obese subjects; as can be seen, the basal metabolism (BM) of the obese subject is higher than that of the normal-weight subjects (P <0.001).
DISCUSSION
Obesity corresponds to an alteration of the system for regulating energy reserves. Whatever the implication of various factors in the development of obesity, it is always the result of an energy imbalance between the calories consumed and those expended [5,6]. In common obesity, it would be interesting to estimate the energy expenditure; this is what has been the main objective of this work.
Total Energy Expenditure (TEE) includes three main components: rest energy expenditure represents approximately 60 to 70% of TEE, postprandial food thermogenesis constitutes approximately 10% to 20% of TEE and finally expenditure of physical activity corresponding to any movement made during the day and is therefore the most variable item of energy expenditure [7-9].
Thus, in our study, we conducted a review of the anthropometric profile associated with the measurement of energy expenditure in a population of overweight and obese adults. By measuring resting metabolism, it was found an increase in basal energy expenditure and an increase in lean mass in obese subjects compared to other weight statuses; lean body mass being a major factor in resting energy metabolism.
This observation assumes that the imbalance in the energy balance of obese subjects is induced by a decrease in the other factors composing the overall energy expenditure such as expenditure due to physical activities and to the thermal effect of food which are necessarily lowered, as opposed to rest energy expenditure [10-12].
It is important to specify that the Basal Energy Expenditure (BEE), considered in absolute value, is higher in the subject obese compared to the normoponderal subject; indeed, the BEE is determined essentially by the importance of the lean mass and however if the BEE is expressed by kg of weight, in this case, it would be lower in the obese subject compared to the normoponderal subject. Other data have confirmed that the decline in overall energy expenditure is inversely correlated with overweight and obesity; indeed, a lowered basal metabolism is predictive of being overweight [13,14].
The development of fat mass is a consequence of an imbalance in the energy balance but, the starting point could be a primitive anomaly of adipose tissue with increased storage capacities. The energy balance would be sort of at the level of demand for storage capacity [15].
CONCLUSION
The field of energy metabolism has developed considerably with the development of different techniques for measuring energy expenditure (indirect calorimetry, doubly marked water method, portable and connected impedance meters, pedometers, accelerometers) usable according to objectives with a better understanding of the variability of energy expenditure. In obesity, indirect calorimetry, the benchmark technique for measuring resting energy expenditure, remains the examination of choice.
The use of smaller devices, called "pocket calorimeters", the validity of which compared to reference tools remains to be clarified, could contribute to the measurement and routine monitoring of energy expenditure of obese patients.
REFERENCES
- Fountain E, Peronnet F, Leverve X (2008) Energy metabolism. EMC Endocrinology Nutrition Pg No: 1-16.
- Ferré P (2016) Physiology of energy metabolism. Medicine of metabolic diseases 10: 6.
- Rigaud D (2009) Impedance measurement Bioelectrical impedance. Medicine for Metabolic Diseases 3: 65-67.
- Abacus A, Fricker J, Ferry M, Apfelbaum M (1991) Measurement of body composition by Bioelectric impedance. Nutr Clin Metabol 5: 165-174.
- Widmaier E, Hershel R, Kevin T (2013) Regulation of organic metabolism and energy balance. Vander Human Physiology (14th edn). Maloine, Paris.
- Ravussin E, Gautier JF (2002) Determinants and control of energy expenditure. Annals of endocrinology. 63: 96-105.
- Ritz P, Couet C (2006) Energy expenditure. Readjustment Med 26: 97103.
- Thermoregulation in humans. In: Wright, et al. Physiology applied to medicine.
- Tam CS, Ravussin E (2015) The role of energy metabolism in the regulation of energy balance. Nutrition and Dietetics Booklet 50: 7-14.
- White BS (2006) Energetics of obesity. Journal of the Biological Society 200: 29-35.
- Wells JCK, Fewtrell MS (2006) Measuring body composition. Arch Dis Child 91: 612-617.
- Montaurier C (2016) Calorimetric chambers for humans and analysis of gas. INRA Technical Guide Pg No: 98-106.
- Singer P, Singer J (2012) indirect calorimetry: a precise tool that is too little used. Resuscitation 21: 406-410.
- Dumont JC, Bruder N, Francois G (1991) Indirect calorimetry: recent data and uses practices-Technical Editions. Encycl Med Chir 11.
- Jastroch M, Divakaruni AS, Mookerje S, Treberg JR, Brand MD (2010) Mitochondrial proton and electron leaks. Essays In Biochemistry 47: 53-67.
Citation: Ghouini A, Khelfat K (2020) Evaluation of Energy Expenditure of Obese Subjects by Bioelectric Method. J Phys Med Rehabil Disabil 6: 059.
Copyright: © 2020 Ghouini A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

