
Evaluation of the Effect of Umbilical Cord Milking on Prognosis in Preterm Infants
*Corresponding Author(s):
Huseyin Avni SolgunDepartment Of Pediatrics, Altinbas University Medicine School, Istanbul, Turkey
Tel:+90 5058990572,
Email:hsynavn@gmail.com
Abstract
Background and aim
It has been reported that delayed cord clamping improves postnatal hemodynamic stability and decreases preterm morbidities, but it could delay initial resuscitation steps. Umbilical Cord Milking (UCM) method has been introduced as an alternative method. The aim of this study is to evaluate the effects of umbilical cord milking on prognosis in preterm infants.
Materials and methods
75 Preterm infants who had underwent to umbilical cord milking smaller than 34 weeks of gestation and 75 Preterm infants who had not underwent to umbilical cord milking smaller than 34 weeks of gestation were included in the study. Hemogram and bilirubin values on 1st and 3th days of life, duration of phototherapy treatment, nutritional status and preterm morbidities during hospitalizations were recorded.
Results
Hemoglobin on the 1st and 3rd days were significantly high in UCM group (p < 0,001). Bilirubin levels and duration of phototherapy on the 1st, 2nd and 5th days were found to be higher in UCM group (p < 0,05). The daily weight gain was higher for UCM group (p < 0,001).
Conclusion
Through the administration of umbilical cord milking, hemoglobin values of the first three days were high in infants. Bilirubin levels were high and duration of phototherapy was longer for these infants. None of the patients in the study required exchange transfusion. Furthermore, weight gain was higher in infants that underwent umbilical cord milking. Future research in the literature will help to determine the efficacy of the UMC method, especially in preterm infants under 34th weeks of gestation.
Keywords
Morbidity; Placental transfusion; Premature infant; Umbilical cord clamping; Umbilical cord milking
INTRODUCTION
Despite the developments in neonatology, the desired decrease in morbidities such as Intraventricular Hemorrhage (IVH), Necrotizing Enterocolitis (NEC), Retinopathy of Prematurity (ROP) and premature anemia in Very Low Birth Weight (VLBW) infants have not been achieved. These morbidities are associated with transfusion and therefore, preterm infants may require multiple erythrocyte transfusions due to phlebotomy losses and premature anemia [1]. With the clamping of the umbilical cord, decrease in blood pressure and deterioration in tissue perfusion may occur in preterm infants whose hemodynamic adaptation is slow. Related studies have focused on examining the results of applying placenta-fetal blood transfusion methods at birth to facilitate the adaptation to postnatal circulation in the early postnatal periods and to reduce transfusion-associated morbidities in the later periods in preterm infants [2]. Placental transfusion can be achieved by delaying cord clamping for 30 - 120 seconds (Delayed Cord Clamping - DCC) or through the administration of Umbilical Cord Milking (UCM) method. When the cord is clamped quickly postpartum, approximately 30 % of the feto-placental blood volume remains in the placenta, while the blood volume remaining in the placenta with DCC is approximately 13% [3]. It has been reported that the delay of cord clamping increases placental transfusion, decreases morbidities such as Periventricular Leukomalacia (PVL) and IVH by providing adequate blood volume postpartum when passing to extra uterine circulation [4]. Umbilical cord milking is an alternative way of achieving placenta-fetal transfusion at the time of delivery and also has been recently evaluated with recent studies.
The aim of this study is to evaluate the effect of UCM on morbidities and mortalities in preterm infants with 34 or below gestational weeks. The study was conducted on two groups; those who were administered UMC and those who were not.
MATERIALS AND METHODS
Between June 2014 and February 2016, 75 preterm infants born by cesarean section delivery with 26 - 34 gestational weeks were included in the study. All preterm infants whose umbilical cord was cut 30 cm long and was milked three times at the approximate speed of 10 cm/sec while at the same level as its mother during delivery formed the group with UCM. In 2014 - 2016, umbilical cord milking method was applied in the hospital clinic. 75 preterm infants born by cesarean section delivery between 26 - 34 gestational weeks before 2014 and whose umbilical cords were clamped immediately after delivery formed the group without UCM [5]. Infants who were born by vaginal delivery, who had major congenital anomalies, chromosome deficiencies, known Rh sensitization, congenital heart diseases, clinical suspicion of placental abruption at delivery due to excessive maternal bleeding and multiple pregnancies were excluded from the study (Figure 1). The infants’ data were obtained retrospectively from their files. The trial was approved by local Human Research Ethics Committee of Adana Numune Training and Research Hospital.
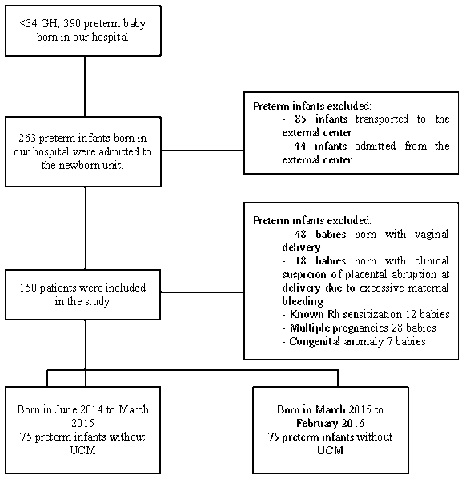
Figure 1: Flow diagram of the study group.
The features of the infants and their mothers were recorded (Table 1). The infants’ blood gas, hemogram and biochemical values, bilirubin values and the duration of their phototherapy treatment, their hospitalization duration, number of erythrocyte transfusion and total transfusion volume, first transfusion day and their Hemoglobin (Hb) values prior to the first transfusion, the day they started Total Parenteral Nutrition (TPN) and its duration, first enteral nutrition time and its amount, day of transition to full enteral nutrition, weight gain during hospitalization, mechanical ventilation and duration of oxygen requirement, Respiratory Distress Syndrome (RDS), IVH, PVL, NEC, sepsis, Patent Ductus Arteriosus (PDA), Bronchopulmonary Dysplasia (BPD) and ROP presence were recorded.
|
Groups |
|
Measurements no Milking (n = 75) Milking (n = 75) P Summary Criteria* Summary Criteria* |
|
Female 40 (53%) 41 (55%) 0.870 Male 35 (47%) 34 (45%) Gestation Week 30.29 ± 1.68 30.28 ± 1.97 0.965 (26 - 34) (26 - 34) Birth Weight (grams) 1560.7 ± 304.90 1454.4 ± 278.10 0.027 (910 - 2390) (840 - 2150) Apgar 1st minute 6.35 ± 0.98 6.4 ± 1.01 0.744 Apgar 5th minute 8.21 ± 0.78 8.19 ± 0.78 0.834 First Body 36.72 ± 0.52 36.79 ± 0.62 0.469 Temperature (°C) Urination in the first 3.74 ± 1.17 3.69 ± 1.27 0.809 24 hours (ml / kg / day) SNAP-PE-II score 22.1 ± 18 19.5 ± 13.10 0.784 16 (0 - 94) 16.5 (0 - 86) Total hospitalization 28 ± 15.86 31.65 ± 14.43 0.058 duration (days) 27 (4 - 87) 29 (3 - 72) Exitus 2 (3 %) 1 (1 %) 1 Discharged 73 (97 %) 74 (99 %) Mother’s Age (years) 27.73 ± 6.66 28.14 ± 6.38 0.708 (16 - 37) ( 16 - 41) Number of Pregnancies 2.45 ± 1.36 2.55 ± 1.44 0.703 2 (1 - 7) 2 (1 - 7) Number of live births 2.09 ± 1.02 1.84 ± 0.94 103 2 (1 - 6) 2 (1 - 4) |
Table 1: Premature infants and their mothers’ demographical features.
*: Summary criteria is given in numbers (%) for gender, results, usage of antenatal magnesium and mother’s smoking. The gestation week, birth weight, SNAP-PE-II, total hospitalization duration, mother’s age, number of pregnancies and number of live births are presented as mean ± Standard deviation, Median (bottom-top), and as mean ± Standard deviation for the other measurements.
The infants who had positive blood cultures were considered as proven sepsis, while those who did not have positive blood cultures but complied with two or more clinical sepsis criteria were considered as clinical sepsis cases [6]. The SNAP-PE-II system was used for the mortality scoring.
STATISTICAL ANALYSIS
IBM SPSS Statistics Version 20.0 software was used in the statistical analysis of the data. Categorical measurements were summarized in numbers, percentages and numerical measurements as mean and standard deviation (median and minimum-maximum where necessary). Chi-square test was used in the comparison of categorical measurements between the groups. The normal distribution of numerical measurements was evaluated using the Kolmogrov Smirnov test. In the comparison of numerical measurements between groups, when the assumptions were justified, t-test was used in independent groups and when assumptions were not justified, Mann-Whitney U test was used. Statistical significance was taken as 0.05 in all tests.
RESULTS
In total 150 premature infants, 75 infants with UCM and 75 infants without UCM were evaluated in the study. The birth weights of the infants without UCM were identified to be higher (p < 0.05). No differences were observed between the groups in terms of the other features of the infants and their mothers (Table 1).
There were no significant differences among the groups in terms of prenatal steroid application to their mothers, preterm delivery reasons, need for resuscitation (positive pressure ventilation, intubation and compressions). The blood gases examined at the 1st and 24th hour of hospitalization and the urea, creatinine, uric acid and albumin levels at the 24th hour were found to be similar in both groups, while the mean Hb values within the 24 hours of life and the 3rd day of the group with UCM were determined to be significantly high (p < 0.001), there was no difference between the groups in terms of white blood cells and Absolute Neutrophil Count (ANC) values. There was no significant difference between the hematologic values of the patients in both groups on the 28th day (Table 2). Although the number of patients who had erythrocyte transfusions, the number of erythrocyte transfusions and the total erythrocyte volume transfused were determined to be higher in the group without umbilical cord milking versus to umbilical cord milking group 8 to 10; this difference was not found to be statistically significant.
|
Measurements Groups |
|
Without milking With milking P (n = 75) (n = 75) |
|
1st day Hemoglobin (g/dl) 15.33 ± 1.54 18.22 ± 1.69 < 0.001 1st day Thrombocyte (x103 / μl) 207.22 ± 62.78 202.64 ± 57.71 0.642 1st day White cells (/ μl ) 10446.1 ± 5416.50 9906.1 ± 3708.80 0.936 1st day Absolute 3574.2 ± 2670.60 2996.7 ± 2202.90 0.167 neutrophil count (/ μl) 3rd day Hemoglobin (g / dl) 14.59 ± 2.390 17.03 ± 2.09 < 0.001 3rd day Thrombocyte 208.21 ± 79.40 198.08 ± 73.55 0.436 (x 103 / μl) 3rd day White cells (/ μl ) 10084.8 ± 5010.50 9427 ± 4697.50 0.494 3rd day Absolute 4122 ± 2816.60 4038.1 ± 3609.10 0.534 neutrophil count (/ μl) 28th day Hemoglobin (g / dl) 12.04 ± 2.79 12.06 ± 2.35 0.968 28th day Thrombocyte 333.7 ± 122.81 304.63 ± 108.74 0.148 (x103/ μl) 28th day White cells (/ μl ) 10810.3 ± 3366.40 11552.8 ± 4325.60 0.521 28th day Absolute 3206.2 ± 17960 3845.1 ± 2755.20 0.363 neutrophil count (/ μl) |
Table 2: The hematological parameters of the patients on the 1st, 3rd and 28th day of hospitalization.
Though the number of patients requiring noninvasive mechanical ventilation was identified to be significantly higher in the UCM group (p = 0.04), noninvasive ventilation durations of the patients in both groups were similar. No difference was determined between the groups in terms of conventional mechanic ventilation, high frequency ventilation and oxygen therapy needs and durations, respiratory failure and surfactant requirements, IVH, PVL, NEC, ROP, PDA and BPD development analysis.
In terms of nosocomial infection development, the incidence of clinical sepsis and culture - proven sepsis frequency was found to be similar between the groups, while the incidence of two or more sepsis episodes was significantly lower in the UCM group (p < 0.05).
In the comparison of bilirubin levels and duration of phototherapy of the groups on the 1st, 2nd and 5th day, between UCM and without UCM group, bilirubin level on the 2nd day, peak bilirubin level, number of patients receiving phototherapy with the diagnosis of neonatal jaundice and total phototherapy duration were found to be high (p < 0.05 for all the examined parameters). The bilirubin levels on the 1st day and 5th day of the groups were found to be similar (Table 3).
|
Measurements Groups |
|
Without milking With milking P (n = 75) (n = 75) Summary Criteria* Summary criteria* |
|
1st day bilirubin 3.67 ± 1.72 4.17 ± 2.39 0.134 level (mg / dl) 2nd day bilirubin 5.88 ± 2.14 6.83 ± 2.29 0.011 level (mg / dl) 5th day bilirubin 7.36 ± 2.50 7.79 ± 2.84 0.339 level (mg / dl) Peak bilirubin 8.79 ± 2.34 9.67 ± 2.48 0.028 level (mg / dl) Total phototherapy 25.46 ± 24.77 36.39 ± 27.45 0.003 duration (hours) Hyperbilirubinemia 14 (19 %) 5 (7 %) 0.027 No Hyperbilirubinemia 61 (81 %) 70 (93 %) 0.027 |
Table 3: The bilirubin levels of the patients and phototherapy durations.
*: Summary criteria are given as numbers for jaundice (percentage) and as mean ± Standard deviation for the other measurements
The time and amount of feeding of the groups, the day of completely enteral feeding, the initiation time and duration of TPN were determined to be similar in both groups. Until the discharge day from the hospital, the daily weight gain was higher in the UCM group (p < 0.001).
DISCUSSION
Increasing evidence exists to suggest that there is improved postnatal hemodynamic stability and decreased neonatal morbidities in preterm infants due to the late clamping of the umbilical cord and the increase in placental transfusion [7]. Postpartum hemodynamic adaptation is slower in preterm infants compared to term infants [8]. Most of the mortalities and morbidities of very low birth weight infants are caused by reduced blood pressure and reduced blood flow to the organs during the postnatal adaptation period [3]. Superior Vena Cava (SVC) flow represents the blood entrance to the heart and is not affected by the presence of fetal shunts. Aladangady et al. [9], reported that through the administration of UCM, the SVC flow and right ventricular stroke volume is higher, no difference is observed in the left ventricular volume, since the left ventricular stroke volume is stable, no difference is found in the cerebral blood flow measured during the transition from fetal life to neonatal life, and better blood pressure and urination are observed in the first 24 hours. They suggested that the absence of fluctuations in cerebral blood flow during this critical time interval is related to the low probability of IVH [9]. The American Gynecological and Obstetrical Society reported in 2012 that DCC decreased the incidence of IVH in premature infants and suggested DCC for 30 - 60 seconds in all premature infants [10]. While the total IVH was found to have decreased in the studies, the fact that no change was found in the severity of IVH frequency suggests that in cesarean deliveries sufficient placental transfusion has not been achieved through DCC. In addition, DCC has not gained a wide range of application due to the concern that it could delay initial resuscitation steps. Thus, UCM method has been introduced as an alternative to DCC [10]. In a meta-analysis of seven randomized controlled studies investigating the effects of UCM on preterm infants with 33 or lower gestational weeks, higher levels of Hb, and decrease in the oxygen need and total IVH cases in the 36th postconceptional week have been reported through the administration of UCM [11]. It has been suggested that UCM improves systemic blood flow and perfusion by increasing SVC flow and right ventricular stroke volume at birth [12]. Renal perfusion is one of the most important indicators of circulatory functions. It has been reported that volume loading with UCM is important in increasing urination, and urination in the first 72 hours increases significantly [13]. Although the urine volume was higher in the first 24 hours in patients who underwent UCM, no significant difference was found in the present study.
The mean number of transfusions in preterm infants was reported to be between 3.3, 5.7 and VLBW infants require erythrocyte transfusion in the first six weeks of life with an approximately 80 % probability [14]. It was found in the Cochrane review that DCC and other placental transfusion enhancing procedures reduce the need for transfusion resulting from premature anemia, provide higher blood pressure and reduce the incidence of IVH [7]. In a study conducted on preterm infants, it was found that UCM provided blood pressure stabilization, decreased the transfusion frequency by increasing the Hb level, decreased mortality and IVH, NEC risk, and did not cause any difference in Apgar scores [4]. In another randomized controlled study conducted on infants born under 32 gestational weeks, it was found, similar to the present study, that in the UCM group, the Hb levels were significantly higher in the 48th hour. However, hemoglobin elevation was not observed in the 6th week [3].
In preterm infants, neutropenia is common in the first week of life and its incidence increases up to 50 %. In premature infants, the risk of sepsis and mortality increases when neutropenia is severe and prolonged [15]. The umbilical cord blood of infants born before the 31st gestation week is rich in hematopoietic stem cells. In the study by Kiliçdag et. al [16], in which they investigated the effects of UCM on ANS and neutropenia incidence in preterm infants, it was found that ANS values were lower in the UCM group and the incidence of neutropenia was higher. They have linked this phenomenon to the rapid migration of hematopoietic cells of the cord blood, which are high in number and are immature during birth, into the bone marrow, which therefore caused ANS to be detected at low levels in the peripheral blood shortly after birth [16]. In the present study, the ANS value was identified to be lower on the 1st and 3rd day in the UCM group, but this difference was not considered to be significant.
In studies which have investigated the effects of UCM on morbidities in premature infants, no difference has been found in the incidences of BPD, PDA, NEC, ROP and IVH between the groups who underwent UCM and those who did not [14,17]. In a recent review, it has been pointed out that UCM procedure decreases IVH, NEC and mortality [10]. In the present study, there was no difference between the groups with and without UCM in terms of the frequency of these morbidities due to prematurity. However, the low number of patients at the 29th gestational week may have contributed to the fact that the morbidities did not differ between the groups.
In studies evaluating the effect of DCC on the frequency of nosocomial infection in premature infants, the frequency of nosocomial infection was found to be lower in the DCC group [12,14,18]. Although there was no difference in the frequency of nosocomial sepsis in the present study, the likelihood of two or more sepsis episodes was found to be lower in the UCM group.
Theoretically, it is thought that UCM treatment will increase the need for hyperbilirubinemia and phototherapy. However, in the related literature, besides the studies reporting there is no difference in the elevation of hyperbilirubinemia and phototherapy need in VLBW infants with UCM, there are also studies reporting high number of patients who need phototherapy and / or patients who have long total phototherapy durations [19-22]. In the present study, the 2nd day bilirubin value, peak bilirubin value, hyperbilirubinemia ratio and total phototherapy duration were identified to be higher in the UCM group. This might have been due to the high Hb values, which causes the erythrocyte cycle and bilirubin productions to be high.
In a randomized controlled study evaluating the relationship between nutrition and milking of the umbilical cord, it was found that in newborn infants with fast cord clamping, the realization of 100 ml / kg feeding and reaching the birth weight was slower compared to the UCM group, and that in the non - UCM group, the digestive system perfusion may have been weaker due to lower blood volume in the circulatory system and lower blood pressure [23]. In the present study, the time they started feeding and its amount, the day of transition to whole feeding, and the duration they received TPN were found to be similar in both groups, but the daily weight gain until discharge from the hospital was significantly higher in the UCM group.
CONCLUSION
Umbilical cord milking is a safe placental transfusion method in preterm infants. With the umbilical cord milking method, Hb values are higher in preterm infants in the first three days, and it facilitates adaptation to life in the transition period. Although bilirubin levels were high and phototherapy duration was long in these infants, no blood change was required in any of the patients in the present study. It has been shown in our study that weight gain is higher in infants who are applied umbilical cord milking. Further studies with higher number of patients in which the long term effects of umbilical cord milking in preterm infants will be evaluated need to be conducted.
DECLERATIONS
Author contributions
Fahri Aydin contributed to data collection, data analysis and interpretation. M. Kurthan Mert contributed to study design, data collection, data analysis and interpretation.
Selvi Gülasi contributed to data analysis, interpretation and manuscript drafting. Hüseyin Avni Solgun contributed to data analysis, interpretation and manuscript drafting.
Ümit Çelik contributed to critical revision of the manuscript. All authors approved the final version of the manuscript.
FUNDING
No funding to be declared.
COMPLIANCE WITH ETHICAL STANDARDS
No declared.
ETHICAL APPROVAL
The trial was approved by local Human Research Ethics Committee of Adana Numune Training and Research Hospital, Turkey.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Carroll PD (2015) Umbilical cord blood-an untapped resource: Strategies to decrease early red blood cell transfusions and improve neonatal outcomes. Clin Perinatol 42: 541-556.
- Dang D, Zhang C, Shi S, Mu X, Lv X, et al. (2015) Umbilical cord milking reduces need for red cell transfusions and improves neonatal adaptation in preterm infants: Meta-analysis. J Obstet Gynaecol Res 41: 890-895.
- Katheria AC, Lakshminrusimha S, Rabe H, McAdams R, Mercer JS (2017) Placental transfusion: A review. J Perinatol 37: 105-111.
- Oh W, Fanaroff AA, Carlo WA, Donovan EF, McDonald SA, et al. (2011) Effects of delayed cord clamping in very-low-birth-weight infants. J Perinatol 31: 68-71.
- Çelik HT, Portakal O, Yigit S, Hasçelik G, Korkmaz A, et al. (2016) Efficacy of new leukocyte parameters versus serum C-reactive protein, procalcitonin, and interleukin-6 in the diagnosis of neonatal sepsis. Pediatr Int 58: 119-125.
- Sommers R, Stonestreet BS, Oh W, Laptook A, Yanowitz TD, et al. (2012) Hemodynamic effects of delayed cord clamping in premature infants. Pediatrics 129: 667-672.
- Rabe H, Diaz-Rossello JL, Duley L, Dowswell T (2012) Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev 15: 003248.
- Rabe H, Reynolds G, Diaz-Rossello J (2008) A systematic review and meta-analysis of a brief delay in clamping the umbilical cord of preterm infants. Neonatology 93: 138-144.
- Aladangady N, McHugh S, Aitchison TC, Wardrop CA, Holland BM (2006) Infant’s blood volume in a controlled trial of placental transfusion at preterm delivery. Pediatrics 117: 93-98.
- Committee on Obstetric Practice, American College of Obstetricians and Gynecologists (2012) Committee opinion no.543: Timing of umbilical cord clamping after birth. Obstet Gynecol 120: 1522-1526.
- Al-Wassia H, Shah PS (2015) Efficacy and safety of umbilical cord milking at birth: A systematic review and meta-analysis. Jama Pediatr 169: 18-25.
- Katheria AC, Truong G, Cousins L, Oshiro B, Finer NN (2015) Umbilical cord milking versus delayed cord clamping in Preterm Infants. Pediatrics 136: 61-69.
- Hosono S, Mugishima H, Fujita H, Hosono A, Okada T, et al. (2009) Blood pressure and urine output during the first 120 h of life in infants born at less than 29 weeks’ gestation related to umbilical cord milking. Arch Dis Child Fetal Neonatal Ed 94: 328-331.
- Alan S, Arsan S, Okulu E, Akin IM, Kilic A, et al. (2014) Effects of umbilical cord milking on the need for packed red blood cell transfusions and early neonatal hemodynamic adaptation in preterm infants born ≤1500 g: a prospective, randomized, controlled trial. J Pediatr Hematol Oncol 36: 493-498.
- Christensen RD, Calhoun DA, Rimsza LM (2000) A practical approach to evaluating and treating neutropenia in the neonatal intensive care unit. Clin Perinatol 27: 577-601.
- Kilicdag H, Gulcan H, Hanta D, Torer B, Gokmen Z, et al. (2016) Is umbilical cord milking always an advantage? Matern Fetal Neonatal Med 29: 615-618.
- Katheria AC, Leone TA, Woelkers D, Garey DM, Rich W, et al. (2014) The effects of umbilical cord milking on hemodynamics and neonatal outcomes in premature neonates. J Pediatr 164: 1045-1050.
- Mercer JS, Vohr BR, McGrath MM, Padbury JF, Wallach M, et al. (2006) Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late-onset sepsis: A randomized, controlled trial. Pediatrics 117: 1235-1242.
- March MI, Hacker MR, Parson AW, Modest AM, de Veciana M (2013) The effects of umbilical cord milking in extremely preterm infants: A randomized controlled trial. J Perinatol 33: 763-767.
- Upadhyay A, Gothwal S, Parihar R, Garg A, Gupta A, et al. (2013) Effect of umbilical cord milking in term and near term infants: Randomized control trial. Am J Obstet Gynecol 208: 120-126.
- Kumar B, Upadhyay A, Gothwal S, Jaiswal V, Joshi P, et al. (2015) Umbilical cord milking and hematological parameters in moderate to late preterm neonates: A randomized controlled trial. Indian Pediatr 52: 753-757.
- Ranjit T, Nesargi S, Rao PN, Sahoo JP, Ashok C, et al. (2015) Effect of early versus delayed cord clamping on hematological status of preterm infants at 6 wk of age. Indian J Pediatr 82: 29-34.
- Hosono S, Mugishima H, Fujita H, Hosono A, Minato M, et al. (2008) Umbilical cord milking reduces the need for red cell transfusions and improves neonatal adaptation in infants born at less than 29 weeks’ gestation: A randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 93: 14-19.
Citation: Aydin F, Solgun HA, Mert K, Gülasi S, Çelik Ü (2020) Evaluation of the Effect of Umbilical Cord Milking on Prognosis in Preterm Infants. J Neonatol Clin Pediatr 7: 048.
Copyright: © 2020 Fahri Aydin, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

