
False Positive or False Negative PET Scan?
*Corresponding Author(s):
Nasrin AzadEndocrinology Section, Edward Hines Jr Veterans Administration Hospital, Division Of Endocrinology And Metabolism, Stritch School Of Medicine, Chicago, United States
Tel:+1 7082028387,
Email:Nasrin.Azad@va.gov
Abstract
Background: Presentation of paraganglioma can be often very puzzling and localizing the site of extra catecholamine production can be very exhausting especially in a very unusual circumstance.
Case Presentation: This is case of 51 years old man with history of anxiety attacks, hyperhidrosis, flashing, palpitation, occasional hypertension and dizziness who had repeated elevated 24 hours’ urine normetanephrine and positive PET scan (Figure 1) then PET scan was negative after he took phenoxybenzamine for 8 weeks.
Conclusion: Based on the clinical and paraclinical data patient most probably had paraganglioma and the reason for the negative second PET scan was due to him taking phenoxybenzamine (for 8 weeks) which is an &alph; blocker and blocks or at least decreases cellular glucose uptake of the tumor cells.
Keywords
ABBREVIATIONS
AR: Adrenalin Receptor
CT: Computed Tomography
DM: Diabetes Mellitus
18F-FDG: 18F- Fluorodeoxyglucose
GLUTs: Glucose Transporters
5-HHIA: 5-Hydroxy Indoleacetic Acid
MRI: Magnetic Resonance Imaging
123I-MIBG: 123I-Metaiodobenzylguanidine
PET: Positron Emission Tomography
INTRODUCTION
Presentation of paraganglioma can be often very puzzling and localizing the site of extra adrenal gland catecholamine production can be very exhausting. The current available advance technology significantly improved the diagnosis of paraganglioma/pheochromocytoma, however, every test should be performed on an appropriate condition, otherwise may not be beneficial or even may become confusing.
CASE REPORT
A 51 years old man was referred to the endocrine clinic for further evaluation of episodic anxiety attacks accompanied with hyperhidrosis, flashing, palpitation and hypertension with systolic blood pressure that occasionally would increase up to 180s to 200s. He had history of grade 3A follicular lymphoma treated with chemotherapy 3 years prior to these events, he also has history of diet controlled Type 2 Diabetes Mellitus (T2DM), hypertension (sub optimally controlled with amlodipine and Lisinopril), bipolar, anxiety disorder (on cetirizine10 mg/day, fluoxetine 20mg/day and temazepam 30 mg at bed time) and hypogonadism (on testosterone cypionate 100mg/week, intramuscular). He demonstrated biochemical evidence of urinary normetanephrine hypersecretion on four separate occasions, in the absence of any interfering medication at least in couple occasions; 1174, 1719, 1562, 1541 (44 - 540mcg/24h). However, serum normetanephrines and serum and urine metanephrines levels, all were within normal levels. Chromogranin A level was 132ng/ml (1.9-15ng/mL) and urinary 5-HIAA and serum dopamine levels were within normal limit. MRI of the neck, chest, abdomen, pelvis and colonoscopy also did not yield more information. CT of chest and abdomen was negative for adrenal or extra-adrenal mass and 123I-MIBG were also negative. However, 18F-FDG whole body PET/CT scan showed focal uptake along a short length of the terminal ileum a few centimeters from the cecum, max SUV of 11 (Figure 1). Given the history of follicular lymphoma, oncology service was also consulted. Although follicular lymphoma is PET avid, oncology service deemed it would be very unusual for isolated lymphoma recurrence on the wall of small bowel and agreed with current working clinical diagnosis of paraganglioma. In addition, there were no signs of any inflammatory process or malignancy in the bowel based on the most recent colonoscopy. It is important to add that during these studies patient was on only cetirizine10mg/day and fluoxetine 20mg/day.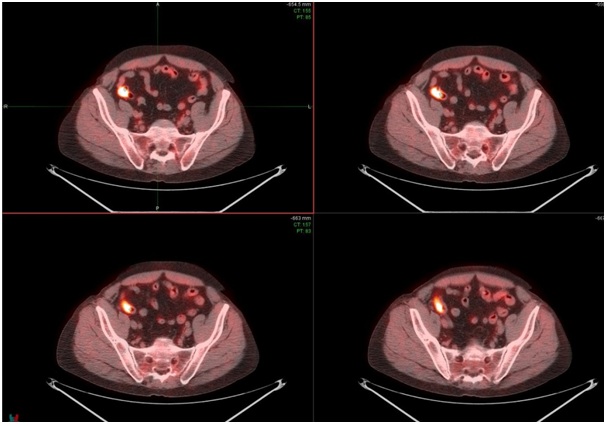
Figure 1: 18F FDG whole body PET scan shows a focal uptake along the short length of the terminal ileum a few centimeters from the cecum, Max SUV11.
Therefore, based on clinical symptoms, elevated urinary normetanephrines on multiple occasions and positive whole body 18F-FDG PET/CT scan, patient was diagnosed of having paraganglioma possibly located on the bowel wall. Patient was started on phenoxybenzamine in preparation for surgery. Surgery service, however, later for the sake of more clear localization repeated 18F-FDGPET/CT while patient on cetirizine10mg/day and fluoxetine 20mg/dayand tramadol 25 mg 3-4 times/day in addition to phenoxybenzamine 10 mg every 6-8 hours (for almost 8 weeks). The second 18F-FDGPET/CT scan fails to show any uptake. Therefore, the surgery was cancelled and dose of phenoxybenzamine was gradually decreased and he was on a “maintenance” dose to keep his blood pressure under control. Unfortunately, he was found death in his restroom few weeks later and there was no autopsy performed and we will never know whether he had paraganglioma and/or the cause of his sudden death. Now, our question is; did he have paraganglioma? Was his first 18F-FDGPET/CT scan a false positive test or his second 18F-FDGPET/CT scan was a false negative test?
DISCUSSION
This case was suspected to have excess secretion of catecholamine’s based on his clinical symptoms of episodic anxiety attacks accompanied with hyperhidrosis, flashing, palpitation and hypertension. The clinical diagnosis of paraganglioma/pheochromocytoma was supported by finding of almost 3-fold increase on urinary normetanephrine (in every occasion that we have studied the urine). As per the reported study the measurements of urine fractionated met machines by mass spectrometry has sensitivity of 97% and specificity of 91% for diagnosis of paraganglioma [1]. Localization studies such as; CT, MRI and MIBG were negative, however, there was increased focal uptake along the short length of the terminal ileum of 18F-FDG in the initial whole body 18F-PET/CT scan (Figure 1) while second 18F-FDG /CT scan became negative. The only difference between these two scan studies was the fact that in the first study patient was taking only a reduced dose of cetirizine and fluoxetine, whereas he was on phenoxybenzamine 30-40 mg/day, cetirizine 10 mg/day, fluoxetine 20 mg/day and temazepam 30 mg at bed time for more than 8 weeks when the second 18F-FDG PET/CT scan was performed of note, this patient was clearly &alph;?blockade, based on his clinical symptoms.
To understand and possibly find some answer to our major dilemma or question that whether the first 18F-FDG PET/CT was a false positive or the second one was a false negative test we referred to the literature. It is accepted that pheochromocytoma/paraganglioma is a catecholamine producing tumor that arises from chromaffin cells of adrenal medulla or sympathetic ganglia. Paraganglioma derives from the parasympathetic nerves mainly located at the base of the skull however, those from sympathetic ganglia are mainly located in the abdomen and produces more nor epinephrine. Although any site containing paraganglionic tissue may develop paraganglioma. The most common extra-adrenal locations of catecholamine-secreting paragangliomas are the superior and inferior abdominal paraaortic areas (75% of extra-adrenal tumors), the urinary bladder (10%, the thorax (10%) and the skull base, neck and pelvis (5%) [2,3].
The size of this tumor is very small and often less than one centimeter and various radiographic means have been used to localize the site of catecholamine’s producing tumor. The sensitivity of CT, MRI and MIBG scintigraphy was 98%, 100% and 78%, and the specificity was 70%, 67% and 100% respectively [4]. The 18F-FDG uptake reflects glucose uptake and behaves as an analog of glucose, its distribution closely follows that of glucose-metabolizing cells and organs but with some differences. The 18F-FDG enters cells by membrane Glucose Transporters (GLUTs) then undergoes phosphorylation by hexokinase to form 18FDG-6-phosphate [5,6], unlike glucose, this undergoes further enzymatic reactions and is effectively trapped into the cell. Increased uptake of 18F-FDG is not specific to paragangliomas, however, most paragangliomas are avid for F18 FDG despite their relative indolence [5,6].
The key to successful PET imaging is adequate preparation of suspected patient to minimize the appearance of potential artefactual uptake patterns that may make interpretation difficult. It is important that the patient be relaxed at the time of injection since muscle uptake of 18F-FDG increases after exercise in the hours leading up to the scan. Chewing, talking and muscle tension are forbidden at least 30 minutes before 18FDG injection. This will keep circulating insulin levels low and minimize uptake of 18FDG into muscle, fat and the myocardium [7]. Diet-controlled diabetic individuals can be treated similarly to nondiabetics [7]. However, diabetic patient’s blood glucose should be normalized as much as possible since high glucose levels reduces 18F-FDG uptake [7]. The short acting insulin should be stopped at least 4 hours before the injection and long acting insulin dose should be safely decreased over the past few days while keeping blood sugar close to normal levels and metformin is preferred to be stopped few days before the test, since both insulin and metformin utilize GLUTs and decrease uptake of 18F-FDG [7,8]. Furthermore, fluoxetine increases mRNA of GLUTs 1&10 in the neuronal tissue and may also interfere with uptake of 18F-FDG [9] and he was taking fluoxetine during both tests however, he was on much smaller dose of fluoxetine on the first study. Our medical center observes all these criteria and this patient had diet control diabetes mellitus.
As we have stated earlier paraganglioma cells has neuronal origin and it is well accepted that glucose is almost the main source of energy for neuronal cells/paraganglioma cells. Glucose enters neuronal cells via various Glucose Transporters (GLUTs) that mediate the sodium-independent facilitated transport of glucose to the cells [9]. Receptors for catecholamine’s (Adrenalin receptor= AR) are widely distributed on neuronal cells [10-12]. ARs are classified into 3 main subgroups &alph;l, &alph;2 and ? all are distributed on the cells membrane, these ARs are functional receptors and are stimulated or blocked by ARs agonist or antagonist. Moreover, it has been shown that adrenaline and noradrenalin mediate the entry of the glucose to the neuronal cells [13], therefore, it is conceivable that administration of AR blocker can decrease neuronal cell glucose uptake [13]. Consequently, administration of phenoxybenzamine that blocks &alph;l and ?&alph;2 AR scan also block the entry of glucose as well as 18F-FDG to the paraganglioma cells. Based on this information blocking the ARs may result into converting a positive 18F-FDGPET/CT to a negative test. This patient was taking phenoxybenzamine 30-40mg for 8 weeks prior to the second test which could have blocked the entry of 18F-FDG to the paraganglioma cells and converted a positive test to a negative test as it had probably occurred in this case.
In summary, it is plausible to assume the first PET/CT was positive and the second PET scan was negative due to patient taking rather large dose of phenoxybenzamine for 8 weeks which had blocked glucose uptake by the tumor cells and converted a positive scan to a negative scan. However, this is only a hypothesis and we do not have a clinical data in this case to prove that.
AUTHOR’S CONTRIBUTION
Nasrin Azad studied Patient’s data, studied the literature and prepared this manuscript.
COMPETING INTERESTS
The author declares that they have no competing interests.
REFERENCES
- Perry CG, Sawka AM, Singh R, Thabane L, Bajnarek J, et al. (2007) The diagnostic efficacy of urinary fractionated metanephrines measured by tandem mass spectrometry in detection of pheochromocytoma. Clin Endocrinol (Oxf) 66: 703-708.
- Erickson D, Kudva CY, Ebersold JM, Thompson BJ, Grant JC, et al. (2001). Benign Paragangliomas: Clinical presentation and treatment outcomes in 236 patients. J Clin Endocrinol Metab 86: 5210-5216.
- Lee JA, Duh QY (2008) Sporadic paraganglioma. World Journal of Surgery 32: 683-687.
- Bravo EI (1991) Pheochromocytoma: New concepts and future trends. Kidney Int 40: 544-556.
- Timmers HJ, Kozupa A, Chen CC, Carrasquillo JA, Ling A, et al. (2007) Superiority of fluorodeoxyglucose positron emission tomography to other functional imaging techniques in the evaluation of metastatic SDHB-associated pheochromocytoma and paraganglioma. J Clin Oncol 25: 2262-2269.
- Timmers HJ. Chen CC, Carrasquillo JA, Whatley M, Ling A, et al. (2012) Staging and Functional Characterization of Pheochromocytoma and Paraganglioma by 18F-Fluorodeoxyglucose (18F-FDG) Positron Emission Tomography. J Natl Cancer Inst 104: 700-708.
- Surasi DS, Bhambhvani P, Baldwin JA, Almodovar SE, O’Malley JP (2014) 18F-FDG PET and PET/CT Patient’s Preparation: A Review of Literature. J Nucl Med Technol 42: 5-13.
- Brewer PD, Habtemichael EN, Romenskaia I, Mastick CC, Costar AC (2014) Insulin-regulated Glut4 Transportation: Membrane Protein Trafficking with Six Distinctive Steps. J Biol Chem 289: 17289-17298.
- Negai K, Inoue T, Konishi H (2014) Increased Gene Expression of Glucose Transporters in the Mouse Brain after Treatment with Fluoxetine and Pergolide. Drug Res (Stuttg) 64: 389-391.
- Benarroch EE (2014) Brain Glucose Transporters: Implications for Neurologic Disease. Neurology 82: 1374-1379.
- Yu AS, Hirayama BA, Timbol G, Liu J, Basarah E, et al. ( 2010) Functional Expression of SGLTs in Rat Brain. Am J Physiol Cell Physiol 299: 1277-1284.
- Kelly SD, Harrell CS, Neigha GN (2014) Chronic Stress Modulates Regional Cerebral Glucose Transporter Expression in an Age-Specific and Sexually-Dimorphic Manner. Physiol Behav 126: 39-49.
- Hutchinsona DS, Summersa RJ, Gibbs ME (2008) Energy Metabolism and Memory Processing: Role of Glucose Transport and Glycogen in Responses to Adrenoceptor Activation in the Chicken. Brain Res Bull 76: 224-234.
Citation: Azad Z (2017) False Positive or False Negative PET Scan? J Clin Stud Med Case Rep 4: 047.
Copyright: © 2017 Nasrin Azad, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

