
Fetal Death in Utero: Epidemiological Aspect, Etiological and Management at the National Hospital of Pikine
*Corresponding Author(s):
Moussa DialloDepartement Of Obstetrics And Gynecology, Pikine University Hospital, Thiaroye Pikine, Pikine, Senegal
Tel:+221 338530071,
Email:moussadiallo25@hotmail.com
Abstract
Objective: Develop the epidemiological profile of IUFD, identify its etiological factors and describe the management.
Patients and methods: This was a prospective, descriptive study from October 2016 to October 2017 at the National Hospital of Pikine (CHNP). The target population consisted of all patients received in the structure having an IUFD. The factors studied were age, parity, number of antenatal cunsultations, type of pregnancy, reasons for consultation and gestational age. The paraclinical aspect, the mode of delivery, the management as well as the maternal prognosis and etiological factors were taken into account.
Results: The main causes identified were vasculorenal syndromes and complications with 27.9% (pre-eclampsia, eclampsia, hypertension and placental abruption), followed by diabetes with 11.1% and 5.6% obstructed labor. Much of our case remains without causes largely due to a very incomplete etiological assessment. The majority of patients had vaginal delivery after spontaneous labor, 12.9% received an induction of labor and 14.8% received a caesarean section immediately.
Conclusion: The causes of IUFD are multiple, often multifactorial, dominated by vasculorenal syndromes and complications. Their supported go through an early and regular monitoring of at risk pregnancies. The causes not found are still important especially in our regions, hence the importance of performing an exhaustive etiological assessment including autopsy and placental histology.
Keywords
Birth; Fetal death in utero; Misoprostol; Stillbirth
INTRODUCTION
In utero fetal death refers by definition to the spontaneous cessation of fetal cardiac activity at a gestational stage greater than 14 week’s gestation. This termination of pregnancy can occur before labor (antepartum fetal death) or during labor (intrapartum fetal death) [1,2]. This is a common event that causes trauma for parents. Its prevalence differs across the world: 2% worldwide with 0.5% in high-income countries [2-4]. In less countries favored, this prevalence may reach 30 per 1000 births [5,6]. In Senegal the prevalence is estimated at 4.18% [3,7]. The most common causes of fetal death are placental causes followed secondarily by chromosomal, malformative and infectious causes [2]. However the occurrence of fetal death in utero remains unexplained in 12 to 50% of cases according to the series [8,9]. This study, conducted at the National Hospital Pikine, aimed to establish the epidemiological profile of IUFD, identify its etiological factors and to describe the management.
PATIENTS AND METHODS
This was a prospective, descriptive study from October 2016 to October 2017 at the National Hospital of Pikine (CHNP). The target population consisted of all patients received CHNP having an IUFD and whose support was made in the structure. Data collection was done using individual questionnaires (survey form) from the hospital records, partographs, the register of births and the register of neonatology. The variables studied were: the age of the parturient, parity, number of antenatal consultations, type of pregnancy, reasons for consultation, gestational age. The paraclinical, the mode of delivery, the management as well as the maternal prognosis and etiological factors were taken into account. The data were received on individual survey forms. The analysis program was achieved through the SPSS Version 23 (Statistical Package for Social Science) for Windows.
RESULTS
Sociodemographic characteristics
Age of patients
The age average of the patients was 28.8 years with extremes of 17 and 51 years. Women between 20 and 30 years were the most represented 55.6%.
Parity
The average rate was 2.2% with a range of 0 and 11. Primiparous were most affected 31.5%.
Clinical aspects
Pregnancy
The pregnancies were singleton in most cases is 94.4% while the twins were 5.6% of cases. The mean for gestational age was 33.3 SA with extremes of 19 and 43 weeks. The portion of 32-36 weeks was the most represented with 33.3% followed by the 37-41 with 27.8% (Table 1).
|
Gestational Age |
Actual (N) |
Percentage (%) |
|
04 |
3.7 |
|
|
22-26 weeks |
11 |
10.2 |
|
27-31 weeks |
22 |
20.4 |
|
32-36 weeks |
36 |
33.3 |
|
37-41 weeks |
30 |
27.8 |
|
>41 weeks |
5 |
4.6 |
|
Total |
108 |
100 |
Table 1: Distribution of patients according to gestational age.
Antenatal
Only 36.1% of patients had performed more than 4 antenatal visits. The average number of antenatal visits was 3 with a range of 0 to 6. 4.6% of patients did not receive any follow-up. Those who benefited more than 4 antenal visit seem to be less affected with 9.3%. All patients had received iron supplementation. Intermittent preventive treatment was administered in 66.7% of patients. The referred accounted for 73.1% against 26.9% of spontaneous admissions. The references were dominated by vasculo-renal syndromes and complications. The absence of active fetal movement was the most frequent reason for consultation or 68% (Table 2). The Bishop score was assessed in all patients, 72.2% had a score greater than 6.
|
Reasons for Consultation |
Actual (N) |
Percentage (%) |
|
No fetal active movements |
53 |
49.1 |
|
Bleeding |
11 |
10.2 |
|
Abdominal pelvic pain |
22 |
20.4 |
|
Seizures |
04 |
3.7 |
|
Hypertension |
18 |
16.7 |
|
Total |
108 |
100 |
Table 2: Distribution of patients according to the reason for consultation.
Paraclinical aspects
Ultrasound
She had been performed in all patients, confirming the diagnosis of fetal death and helping the etiological diagnosis. Hidden etiological factors were dominated by Vascular and Renal Syndromes (SVR) and complications 56.6% (Figure 1).
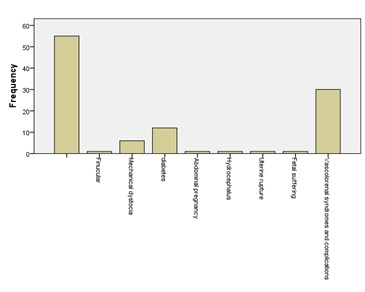 Figure1: Distribution of patients according to the causative factors.
Figure1: Distribution of patients according to the causative factors.
Biology
The blood count was performed in 81 patients or 75%. Blood typing was performed in 79.6% of patients, all were positive Rh and OO group was the most represented with 50%. Leukocytosis was found in 23% of patients. C-reactive protein was performed in 81 patients, it was positive in 6.1%.
Supported
Labor induction
The labor was spontaneous in 71.3% of cases, 16 patients had received a caesarean immediately, 14.8%. Thirteen patients had a Bishop score less than 6, they had an artificial labor trigger of 13.9%. The trigger was made by prostaglandins including misoprostol, the dose was based on gestational age and the vaginal route was the only one used.
Mode of delivery
The vaginal mode of delivery was the most common 70.4% (Figure 2).
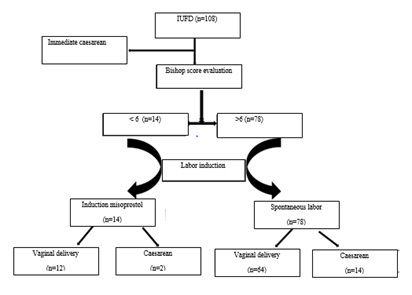 Figure 2: Distribution of patients according to the labor induction method and route of delivery.
Figure 2: Distribution of patients according to the labor induction method and route of delivery.
Fetal data
Sixty-five of the dead infants were male, 60.2%. They were macerated in 75% of cases, occurring more frequently in the SVR and complications (Figure 3). The average fetal weight was 1920grs with extremes of 100 to 4800grs.
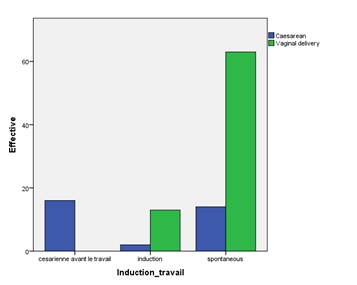 Figure 3: The ratio of induction of labor and mode of delivery.
Figure 3: The ratio of induction of labor and mode of delivery.
DISCUSSION
Maternal age greater than 35 years increases the risk of fetal death in utero intrapartum and antepartum [2]. This was demonstrated in our study. Indeed IUFD coast in over 35 years was 20.4% in our study. We find similar frequencies in several other studies. The risk of fetal death in the over 35 years is mostly associated with chromosomal abnormalities due to an alteration of the intrinsic quality of gametes with time [10]. Primiparity is associated with an increased risk of fetal death of 42%. Indeed primiparas are more vulnerable to certain diseases such as preeclampsia source IUFD. We found a prevalence of 31.5% in primiparous. Our results are similar to those of Diallo et al., Andriamandimbison and Z. However, some studies found a relationship between multiparity and IUFD. Indeed, these are often elderly patients, at risk of pre-eclampsia, diabetes, intrauterine growth retardation, placental abruption or placenta previa behind the IUFD [11,12].
The risk of fetal death in utero decreases with the number of prenatal consultations. Indeed, we found that patients who have more than 4 prenatal visits were less exposed with a frequency of 9.3%. Mohsin had found an increased risk of 1.12 (95% CI 1.01 to 1.26) for patients where the first contact to motherhood was held after the first quarter. Vintzileos et al., showed a risk tripled if the pregnant woman had never consulted during pregnancy [13,14]. The causes of fetal death are many and well codified. Nevertheless, 15 to 50% of them remain unexplained despite a thorough etiological assessment [5,9,15]. We find in our study 50.9% of undetermined causes. This rate, however, could be explained by the insufficiency of our paraclinical data including the absence of placental histology. Among the etiologies found, vasculo-renal syndromes and complications were more frequent at 27.9%. The incidence of fetal death is both higher in hypertensive disease, this risk is increased in case of complications [10]. The IUFD occurring by the gradual or sudden deline in placental perfusion due to the lack of remodeling of the spiral arteries.
The second etiology found was diabetes with a rate of 11.1%. It is a recognized risk factor for fetal death. Its pathophysiology is however complex and appears to be multifactorial. The meta-analysis published in the Lancet by Flenady et al., estimated that the risk of fetal death was three times higher in women with pre-existing diabetes compared to women who did not [16]. Each year about 2194 IUFD may be assigned to it in developed countries. The third group of etiology found in our study was mechanical dystocia. They are not usually cited as a cause of fetal death. However, in the absence of early and appropriate management they can have dramatic consequences, namely an intrapartum death or even a maternal death. We found 5.6% of cases of dystocia. The other etiologies found in our study are, at equal frequency, funicular, malformative, haemorrhagic and abdominal pregnancies.
After IUFD, labor began spontaneously in place within three (3) weeks of the diagnosis in 85% of cases [17,18]. However, this expectation is not without risk. Indeed the prolonged retention can be the cause of disseminated intravascular coagulation due to release of fetal or placental thromboplastin and. It is therefore necessary to conduct an induction of labor to avoid this complication. The latter will be based on several factors namely maternal condition, obstetric history and cervical conditions. 71.3% of patients were entered spontaneously into labor and a trigger was performed in 13.9%. Misoprostol is a synthetic prostaglandin, similar to natural PGE1, it is used in the induction of labor especially in cases of fetal death and whatever the age of the pregnancy. Several routes of administration are possible, but the vaginal is the most common. All our trips were made by vaginally every 6 hours and doses were administered according to gestational age. It is proved that the vaginal administration reduces the induction-expulsion period and the rate of patients who have not given birth within the first 24 hours of release [17]. 70.4% of the patients who had started had delivered vaginally (Figure 2), rate close to that found in the study of Abediasl et al., [19].
CONCLUSION
The causes of IUFD are multiple, often multifactorial, dominated by vasculorenal syndromes and complications. Their supported go through an early and regular monitoring of at risk pregnancies. The unexplained causes are still important especially in our regions, hence the importance of performing an exhaustive etiological assessment including autopsy and placental histology. Treatment involves rapid evacuation of the uterine contents. The route of delivery will depend on maternal status and cervical conditions.
REFERENCES
- Mercuzot A (2015) fetal death case analysis in utero chu of Amiens between 2011 and 2014: Proposal of a relevant etiologic in 2015. University of Picardie Jules Verne, France.
- Quibel T, Bultez T, Nizard J, Subtil D, Huchon C, et al. (2014) [In utero fetal death]. J Gynecol Obstet Biol Reprod (Paris) 43: 883-907.
- Diallo MH, Barry M, Balde MD, N Keita (2016) Intrauterine fetal death (fetal death): Demographic aspect, management and prognosis for Maternal Maternity of Mamou Regional Hospital.
- Kangulu IB, A'Nkoy AM, Lumbule JN, Umba EK, Nzaji M, et al. (2016) [Frequency and Maternals risk factors of fœtal intra uterin death at Kamina, Democratic Republic of Congo]. Pan Afr Med J 23: 114.
- Martinek IE, Hohlfeld PJ (2006) Supports death in utero: What results suggest? Obstet Gynecol 35: 594-606.
- Stanton C, Lawn JE, Rahman H, Wilczynska-Ketende K, Hill K (2006) Stillbirth rates: Delivering estimates in 190 countries. Lancet 367: 1487-1494.
- globalEDGE (2019) Senegal: National Agency of Statistics and Demography (ANSD). globalEDGE, Michigan, USA.
- Man J, Hutchinson JC, Heazell AE, Ashworth M, Levine S, et al. (2016) Stillbirth and intrauterine fetal death: Factors affecting determination of cause of death at autopsy. Ultrasound Obstet Gynecol 48: 566-573.
- Husband EC (2014) Intrauterine fetal death: Is there an interest in repeating of haemostasis to detect coagulopathy? Université François-Rabelais, Faculty of Medicine towers, France.
- Andriamandimbison Z, Randriambololona DM, Rasoanandrianina BS, Hery RA (2013) [Causes of in utero fetal deaths: 225 cases at Befelatanana Hospital, Madagascar]. Med Sante Trop 23: 78-82.
- Cabrol D, Goffinet F (2003) Fetal death in utero. Treaty of' trique Obste. Flammarion me'decine-Science: 353-358.
- Conde-Agudelo A, Belizán JM, Díaz-Rossello JL (2000) Epidemiology of fetal death in Latin America. Acta Obstet Gynecol Scand 79: 371-378.
- Mohsin M, Bauman AE, Jalaludin B (2006) The influence of antenatal and maternal factors on stillbirths and neonatal deaths in New South Wales, Australia. J Biosoc Sci 38: 643-657.
- Vintzileos AM, Ananth CV, Smulian JC, Scorza WE, Knuppel RA (2002) The impact of prenatal care in the United States on preterm births in the presence and absence of antenatal high-risk conditions. Am J Obstet Gynecol 187: 1254-1257.
- Belhomme N (2015) Fetal deaths in utero seen by the internist: Challenges and difficulties illustrated through a series of 53 cases. Internal Medicine Journal 36: 62-63.
- Siddiqui F, Kean L (2009) Intrauterine fetal death. Obstetrics, Gynecology and Reproductive Medicine 19: 1-6.
- Beucher G, Dolley P, Stewart Z, Carles G, Grossetti E, et al. (2015) [Fetal death beyond 14 weeks of gestation: Induction of labor and obtaining of uterine vacuity]. Gynecol Obstet Fertil 43: 56-65.
- Abediasl Z, Sheikh M, Pooransari P, Farahani Z, Kalani F (2016) Vaginal misoprostol versus intravenous oxytocin for the management of second-trimester pregnancies with intrauterine fetal death: A randomized clinical trial. J Obstet Gynaecol Res 42: 246-251.
Citation: Diallo M, Daff HMB, Diouf AA, Diallo CAN, Touré Y, et al. (2019) Fetal Death in Utero: Epidemiological Aspect, Etiological and Management at the National Hospital of Pikine. J Reprod Med Gynecol Obstet 4: 033.
Copyright: © 2019 Moussa Diallo, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

