
Functional Outcomes in Patients with a Left Ventricular Assist Device
*Corresponding Author(s):
K Rao PoduriDepartment Of Physical Medicine And Rehabilitation, University Of Rochester Medical Center, Elmwood Avenue, Rochester, United States
Tel:+1 585 2753274,
Fax:+1 5854422949
Email:kr_poduri@urmc.rochester.edu
Abstract
Background: To evaluate functional outcomes of patients with a Left Ventricular Assist Device (LVAD) with cardiac failure by using Functional Independence Measure (FIM) and to determine whether age and co-morbid conditions impact their outcomes.
Methods: This was a retrospective study of patients with LVAD who underwent acute inpatient rehabilitation at a tertiary care hospital from 2010 to 2014. Their age, admission and discharge FIM, FIM gains, Length of Stay (LOS), Efficiency Ratios (ER), and comorbid conditions were gathered. Time from LVAD placement to rehabilitation admission is variable depending on patients’ ability to endure the acute rehabilitation process. Correlation coefficients for these characteristics were calculated and Student’s t-test conducted with p value set at
Results: The average age of patients was 62 years (range, 36-79 years). The mean admission and discharge FIM scores were 76.56 and 96.69 respectively. The mean FIM gain was 20 (range, - 8 to 39). The mean length of stay was 15 days (range, 6-23 days). The mean ER (FIM gain over LOS) was 1.5. The highest and lowest ERs were that of a 61 year old and a 43 year old, respectively. Comorbid conditions did not influence the functional gains, because most individuals had similar problems and did not lose any time during their rehabilitation due to their medical instability.
Conclusion: Overall, patients did well enough to be discharged home. Independent of age, admission FIM was significantly associated with LOS. Age and comorbidities did not appear to have a great impact on the FIM gains and/or ER in LVAD patients going through acute inpatient rehabilitation.
INTRODUCTION
Heart disease remains a leading cause of morbidity and mortality in the United States per Centers for Disease Control (CDC) [1]. However, overall heart disease has shown a fairly steady decline since 1980 (Morbidity and mortality report 2000) [2] possibly due to advances in cardiac interventions, both surgical and non-invasive methods. As patients with various forms of heart disease live longer due to these advances, the field of physiatry is increasingly managing these patients for their rehabilitation needs. In the rehabilitation field, functional outcomes directly relate to Quality of Life (QOL), which is defined within our field as the overall well-being of a person, including physical and mental health, recreation/leisure time, and social acceptance. LVAD patients, by the very nature of their disease, have a significantly reduced QOL. The task of improving QOL in this patient population is the goal of our rehabilitation.
The approach to managing heart disease continues to evolve. A brief description of the development of the LVAD is useful to put the management of heart failure into historical perspective. Before its development, those with New York Heart Association (NYHA) stage IV heart failure would be medically managed, then placed on a waiting list for a heart transplant. Additionally, many of these NYHA stage IV patients would not qualify for a heart transplant secondary to other medical comorbidities. In the early 1960s, Dr. Michael DeBakey developed the concept of a Ventricular Assist Device (VAD). By 1966, the first successful VAD was implanted (Lee S et al.,) [3].
An LVAD works by connecting the left ventricle to the descending thoracic aorta via a drive-line pump connected to an external battery, thereby creating an alternative bypass conduit around the left ventricle resulting in LV offloading [4]. The schematic description of the implantable LVAD is shown in figure 1. There are three generations of LVADs; for the purpose of this study, we will briefly discuss the third generation of continuous flow LVADs, as these are being currently implanted.
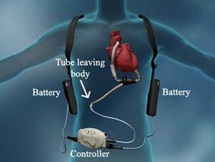
The third generation of LVADs, Heart Mate II (HMII), uses a centrifugal continuous-flow pump with a magnetically suspended rotor in the blood flow path; whereby, controlled electric currents running through coils contained in the pump housing apply centrifugal forces to the magnets, which in turn cause the rotors to spin. The VAD alters the flow dynamics, ultimately decreasing or eliminating the patient’s pulse. Continuous flow LVADs (Figure 1) are generally more compact and have been shown to be more durable [5].
LVADs now have three roles within clinical practice, all of which serve to improve patients QOL: a. Patients awaiting heart transplant or a “bridge to transplantation;†b. those on the road to recovery or “bridge to recovery;†and c. Patients managed with an LVAD for life or “destination therapyâ€. In all these settings, LVADs have become essential components in the management of heart failure. In this article we will focus on “destination therapyâ€, as these are the patients receiving inpatient rehabilitation services.
Regarding Quantitative Training Load (QTL), there is scant standardization when it comes to LVAD rehabilitation. Throughout the country, institutions have their own protocols, but studies relating to clinical outcomes of LVAD patients, as regards to age-related health factors and co-morbidities are severely limited. Although advanced age, female gender, and diabetes mellitus were reported as predictors of poor clinical outcomes (Dang N et al.,) [6].
There are limited studies that focused on outcomes of LVAD placement and acute inpatient rehabilitation. The purpose of our study is to assess functional outcomes using the functional independence measure and to determine whether age and co-morbid conditions have any impact on the outcomes of patients undergoing acute rehabilitation with LVADs.
METHODS
This is a retrospective study. The charts of 23 LVAD patients that underwent acute hospital based rehabilitation were collected. LVAD patients were screened and accepted for admission to go through inpatient rehabilitation when there was functional deficits and when medical stability was achieved. The records of those patients who were able to undergo three hours a day of therapies and completed rehabilitation were included in this study. Acute inpatient rehabilitation criteria require that patients participate in therapies for three hours a day. Patients underwent rehabilitation with a common goal as mentioned by the WHO, to restore optimal physical, medical, psychological and social status. Our patients underwent exercises and therapies focused on restoring all these aspects. First and foremost, patients were provided with psychological and social support. Patients’ therapies included Range of Motion (ROM) and stretching techniques to reestablish pain free movements, Activities of Daily Living (ADL) skill retraining, endurance exercises, and gait reeducation. Exercises also included proprioception, balance, coordination, and upper and lower body strengthening. They were taught compensatory techniques to further their independence when necessary, together with training in proper management and care of their LVAD system. In addition, our patients were provided with psychological and social support. The patients were not monitored for specific cardiac function with any particular protocols. They were treated similar to general rehabilitation patients focusing on improving their functional deficits. Complications after the LVAD placement prior to admission to the rehabilitation unit, patients’ ejection fractions, and medications were not studied.
Currently, in the United States, the scale, Functional Independence Measure is widely used as it is standardized and tested for its reliability and validity. The information collected via Electronic Medical Records (EMR) included data from a five year period. The study evaluated the functional outcomes of rehabilitation for cardiac patients with LVADs in an acute rehabilitation unit from a tertiary care hospital.
The data included demographics, past medical history, primary diagnosis, as well as data of the scores on Functional Independence Measure, co-morbid conditions, and length of stay in the rehabilitation unit, FIM efficiency ratio and disposition. The outcome of rehabilitation is evaluated through the FIM (Table 1) (Figure1), which contains 18 items to evaluate the patient’s functional self-care, sphincter control, transfers, locomotion, communication, and social cognition. The Functional Independence Measure is a reliable tool, which has been used for many years to measure patient progress in the inpatient rehabilitation settings (Ottenbacher KJ et al.,) [7]. Functional Independence Measure scores are indicators of the level of disability within cognitive and motor domains, based on the level of assistance that the patient requires to perform important functional tasks. Our patients received physical, occupational and speech therapies for a total of three hours a day in divided sessions. Our patient population did not have any deficits in the cognitive domain and hence the analysis included was mainly on the motor domains that impacted their self-care and mobility. Functional Independence Measure scores were measured upon Admission (Adm FIM) and at time of Discharge (D/C FIM).
| FIM Items | |
| Self-Care | |
| a. Eating | |
| b. Grooming | |
| c. Bathing | |
| d. Dressing - Upper body | |
| e. Dressing - Lower body | |
| f. Toileting | |
| Sphincter Control | |
| a. Bladder Management | |
| b. Bowel Management | |
| Transfers | |
| a. Transfer - Bed, chair, wheelchair | |
| b. Toilet | |
| c. Tub, Shower | |
| Locomotion | |
| a. Locomotion: Walk, Wheelchair | |
| b. Locomotion: Stairs | |
| Communication | |
| a. Comprehension | |
| b. Expression | |
| Social cognition | |
| a. Social Interaction | |
| b. Problem solving | |
| c. Memory | |
| The FIM Rating Scale | |
| No Helper | |
| 7. Complete: Independence | |
| 6. Modified: Independence (Device) | |
| Helper - Modified Independence | |
| 5. Supervision: (subject 100%) | |
| 4. Minimal Assistance: (Subject = 75%) | |
| 3. Moderate Assistance: (Subject = 50%) | |
| Helper - Complete Dependence | |
| 2. Maximal Assistance: (subject = 25%) | |
| 1. Total Assistance: (subject = less than 25% | |
Table 1: Functional Independence Measure (FIM).
Student’s t- test and correlation coefficient are the statistical methods used to analyze the data. The relationship between the two variables is examined by the Pearson correlation coefficient. Its significance is determined from Fisher’s Z-transformation to the correlation coefficient.
RESULTS
Of the 23 patients there were two females and 21 males with 15 under 65 years of age (age range 36 to 64) and eight of them 65 years and older (range 65 - 79). The demographics, FIM data, Length of Stays (LOS) in the rehabilitation unit, efficiency ratios (FIM gain/LOS) and the comparisons are described in table 2. Difference between the means of the two groups (65 yrs.) is evaluated by Student’s t - test (Table 1). We found no statistically significant difference regarding LOS, Adm-FIM, D/C-FIM, total FIM gain, and ER, between the two age groups.
| Mean Values |
Age <65 Years n = 15 |
Age >65 Years n =8 |
|
| Age (St.dev) | 55 (8.07) | 71 (4.62) | NS |
| Admission FIM*(St. dev) | 78.125 (5.59) | 78 (2.8) | NS |
| Discharge FIM(St. dev) | 99 (6.93) | 104.5 (10.2) | S*** |
| FIM Gain (St. dev) | 21 (10.98) | 26.375 (9.21) | NS |
| LOS** (St. dev) | 14 (9.63) | 14 (10.16) | NS |
|
Efficiency Ratio LOS/FIM (St. dev) |
2 (0.85) | 2 (0.81) | NS |
Table 2: Demographics.
*FIM: Functional Independence Measure
**LOS: Length of Stay
***S: Significant at p<0.05
Correlation coefficient through the Student’s t-test is also assessed between age, LOS, Adm FIM, D/CFIM, total FIM gain and ER. For all 23 patients age did not correlate with any of the functional outcomes assessed (Table 3). However, significantly positive correlations are found between (a). LOS and ER, (r=0.520 and p=0.011); (b). Adm FIM and D/C FIM (r=0.446 and p=0.033); (c). D/C FIM and FIM gain, (r=0.699 and p<0.00001); (d). D/C FIM (r=0.866 p<0.00001); and (e). FIM Gain (r=0.772 and ER p<0.00001) and ER. Significantly negative correlation is found only between Adm FIM and LOS (r=- 0582 and p=0.004).
| Age | LOS | Adm FIM* | D/C FIM | FIM Gain | |
| LOS | -0.065 | ||||
| Adm FIM | -0.056 | -0.582* | |||
| D/C FIM | 0.216 | -0.299 | 0.446* | ||
| FIM Gain | 0.273 | 0.149 | -0.328 | 0.699** | |
| Efficiency Ratio | 0.200 | 0.520* | 0.187 | 0.826** | 0.722** |
Table 3: Correlation coefficients for all patients (n=23).
a*p value <0.05
**p value <0.01
When age was further divided into groups, the patients less than 65 (Table 4), as well as 65 and greater than 65 years of age (Table 5), showed significantly negative correlations between LOS and Adm FIM (for 65 r=- 822 with p=0.012).
| Age | LOS | Adm FIM | D/C FIM | FIM Gain | |
| LOS | -0.147 | ||||
| Adm FIM | -0.026 | -0.586* | |||
| D/C FIM | 0.122 | -0.245 | 0.498 | ||
| FIM Gain | 0.158 | 0.14 | -0.147 | 0.784** | |
| ER | 0.235 | -0.582* | 0.347 | 0.812** | 0.678** |
Table 4: Correlation coefficients for
**p value <0.01
| Age | LOS | Adm FIM | D/C FIM | FIM Gain | |
| LOS | 0.583 | ||||
| Adm FIM | -0.191 | -0.822** | |||
| D/C FIM | -0.239 | -0.576 | 0.455 | ||
| FIM Gain | -0.025 | 0.303 | -0.591 | 0.449* | |
| ER | -0.364 | -0.345 | -0.02 | 0.845 | 0.785* |
**p value <0.01
Comorbid conditions found in these patients are described in table 6. Functional outcomes of patients were independent of their co-morbidities and also the number of co-morbid conditions present showed no differences in any of the areas analyzed. We reviewed the comorbidities and expected to have an influence on the functional outcome; however, we did not find any difference, perhaps due to selection of the patients for admission only after medical stability was attained. No adverse events occurred during their rehabilitation stay.
| No of patients | Comorbid conditions
|
| 1 | Anemia |
| 1 | Aorto-coronary bypass |
| 1 | Artificial heart replacement |
| 1 | Atherosclerosis |
| 1 | Deep Vein Thrombosis |
| 1 | Sleep apnea |
| 1 | Below knee amputation |
| 2 | Acute kidney failure |
| 2 | Alcohol abuse |
| 2 | Acute Myocardial infarction |
| 2 | Anxiety state |
| 2 | Cardiogenic shock |
| 2 | Chronic ischemic heart disease |
| 3 | Primary cardiomyopathy |
| 2 | Pressure sores |
| 2 | Chronic renal failure |
| 3 | Chronic airway obstruction |
| 3 | Chronic kidney disease |
| 3 | Atrial fibrillation |
| 4 | Congestive heart failure |
| 7 | Depressive disorder |
| 7 | Dysphagia |
| 7 | Hyperlipidemia |
| 11 | Diabetes Mellitus type II |
| 13 | Hypertension |
On follow up, it was noted that with our patient population, seven out of 23 have since passed away. Of those deceased, time of implant to death ranged from one year to four years.
DISCUSSION
Early rehabilitation after LVAD placement is an important and often necessary step to functional independence. In order to be discharged home, post LVAD implant care requires the patient and/or caregivers are able to independently and safely perform ADLs, ambulate, and, in addition, manage drivelines and battery packs. Acute rehabilitation promotes early mobilization, which is paramount for long term, active, and healthy living. Studies have shown that LVADs promote cardiac recovery, by allowing the native heart to rest while the VAD does the work. With the bridge to recovery, the LVAD offloading and early exercise help restore the patient’s native ventricular output. As per Loyaga-Rendon et al., [8], patients show improvements in exercise capacity after LVAD implantation, but the effect is noted to be less than predicted.
In our retrospective study, patients with LVADs demonstrated an improvement in their functional status regardless of their comorbidities. Patients tolerated three hours of therapies a day, five days a week: physical and occupational therapies and if indicated speech therapy. Functional Independence Measure gain averaged about 20-points, which compared favorably to benchmarks for mean FIM gains nationally for patients admitted to acute inpatient rehabilitation units with cardiac diagnoses. The mean FIM efficiency was low at 1.5 for LVAD patients compared to 2.88, which is the national average of all cardiac diagnoses. A higher rate of post-op complications for LVAD patients is noted in comparison to patients with heart failure without an LVAD. Our group of patients had minor complications during their rehab stay, which did not interfere with their rehabilitation. Acute inpatient rehabilitation after LVAD placement has not been studied extensively. Prior studies, by Nguyen and Stein [9] and Chu et al., [10] and English and Speed [11] have evaluated FIM scores and LOS, which demonstrated similar results as our study. However, no study has gone deeper into the complications that could impact the length of stay which, in turn, affects the functional gains. Nguyen’s study demonstrated a length of stay averaging 17.5 days, which is comparable to our study, which averaged 15 days of acute rehabilitation, whereas the national average is 10.7 days. However, national statistics account for all cardiac diseases, which may tend to shorten the LOS, as compared to post-op LVAD patients. In addition, 83% of our patients were discharged to home rather than a skilled nursing facility, as compared to the national average of 75% who were discharged home. It would be important to assess long term functional gains and ability to retain them after discharge as they relate to quality of life.
Although no adverse events occurred during the rehabilitation stay, the potential post-LVAD implant complications are quite significant and common, including bleeding (especially GI bleeds), infections (especially pocket wound/incisional), arrhythmias, pump thrombosis, thromboembolism, stroke, depression, and device failure. An earlier study, the REMATCH trial by Rose EA et al., [12], also demonstrated that patients with an LVAD had higher rates of complications; but, even with complications, QOL and survival improved. Slaughter et al., [13] compared continuous-flow left ventricular assist device with a pulsatile device for advanced heart failure and reported that the former improved survival free from stroke and device failure at two years but both devices significantly improved the quality of life and functional capacity.
Long term survival is dependent on the stage of disease, comorbidities, and functional status. Data on long-term survival rates in patients with an LVAD are limited with only a few studies investigating survival rate. At this time, there are studies only addressing short term follow-up. As mentioned earlier, it was noted that with our patient population, seven out of 23 have since passed away with the time of implant to death ranging from one year to four years. At this time, the remaining patients from our institution had their LVADs for up to five years. It is likely that life expectancy will continue to increase with placement of LVADs given the improvement in care and pump design. Quality of life will need to be investigated to better help define the benefits of the LVAD. One preliminary randomized control study by Hayes et al., studied on a small sample of patients using the 36-Item Short Form Health Survey (SF-36) reported greater improvement in peak oxygen consumption and QOL in the exercised group compared to the control group (Hayes K et al.,) [14].
STUDY LIMITATIONS
CONCLUSION
REFERENCES
- Centers for Disease Control and Prevention (2015) About Underlying Cause of Death 1999-2013. CDC Wonder, National Center for Health Statistics, Hyattsville, Maryland, USA.
- NIH: National Heart, Lung, and Blood Institute Morbidity and Mortality (2012) NHLBI Morbidity and Mortality Chart Book. Bethesda, Maryland, USA.
- Lee S, Fukamachi K, Golding L, Moazami N, Starling RC (2013) Left ventricular assist devices: from the bench to the clinic. Cardiology 125: 1-12.
- Norman JC (2004) An Abdominal Left Ventricular Assist Device (ALVAD): perspectives and prospects. 1974. Tex Heart Inst J 31: 289-302.
- Slaughter MS, Pagani FD, Rogers JG, Miller LW, Sun B, et al. (2010) Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J Heart Lung Transplant 29: 1-39.
- Dang NC, Topkara VK, Kim BT, Mercando ML, Kay J, et al. (2005) Clinical outcomes in patients with chronic congestive heart failure who undergo left ventricular assist device implantation. J Thorac Cardiovasc Surg 130: 1302-1309.
- Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC (1996) The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil 77: 1226-1232.
- Loyaga-Rendon RY, Plaisance EP, Arena R, Shah K (2015) Exercise physiology, testing, and training in patients supported by a left ventricular assist device. J Heart Lung Transplant 34: 1005-1016.
- Nguyen E, Stein J (2013) Functional outcomes of adults with left ventricular assist devices receiving inpatient rehabilitation. PM R 5: 99-103.
- Chu SK, McCormick Z, Hwang S, Sliwa JA, Rydberg L (2014) Outcomes of acute inpatient rehabilitation of patients with left ventricular assist devices. PM R 6: 1008-1012.
- English ML, Speed J (2013) Effectiveness of acute inpatient rehabilitation after left ventricular assist device placement. Am J Phys Med Rehabil 92: 621-626.
- Rose EA, Moskowitz AJ, Packer M, Sollano JA, Williams DL, et al. (1999) The REMATCH trial: Rationale, design, and end points. Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure. Ann Thorac Surg 67: 723-730.
- Slaughter MS, Rogers JG, Milano CA, Russell SD, Conte JV, et al. (2009) Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med 361: 2241-2251.
- Hayes K, Leet AS, Bradley SJ, Holland AE (2012) Effects of exercise training on exercise capacity and quality of life in patients with a left ventricular assist device: a preliminary randomized controlled trial. J Heart Lung Transplant 31: 729-734.
- Kugler C, Malehsa D, Schrader E, Tegtbur U, Guetzlaff E, et al. (2012) A multi-modal intervention in management of left ventricular assist device outpatients: dietary counselling, controlled exercise and psychosocial support. Eur J Cardiothorac Surg 42: 1026-1032.
Citation: Norton D, Kuhar S, Poduri KR (2015) Functional Outcomes in Patients with a Left Ventricular Assist Device. J Phys Med Rehabil Disabil 1: 007.
Copyright: © 2015 Denise Norton, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

