Gastric Emptying Scintigraphy in the Management of Diabetic Gastroparesis: A Brief Review of Literature
*Corresponding Author(s):
Vandana K DhingraDepartment Of Nuclear Medicine, AIIMS Rishikesh, India
Email:Mmodisbanu@yahoo.com
Abstract
Diabetes Mellitus is one of the most common non communicable diseases, with rising incidence and prevalence. Several systemic complications like retinopathy are known to arise in long standing diabetes, gastroparesis is one such complication, and adds to morbidity of these patients. Early diagnosis of gastroparesis may be valuable in prompt management and thereby improving patient outcome. Various methods have been devised for diagnosis of gastroparesis but Gastric Emptying Scintigraphy (GES) stands out as the test of choice as it is physiological study which quantifies the gastric retention and can also be used for follow up of these patients after initiating treatment. Careful consideration of meal used, and adherence to standardized procedure minimizes the errors in the results and increases validity of the study. Several studies have been performed utilizing GES have helped in evaluating role of various disease related factors in diabetic gastroparesis. We review major studies done utilizing GES in the evaluation of diabetic gastroparesis. Larger multicentric studies will help in further standardizing the procedure especially with regards to the meal used in GES which is one of the main limitation restrictive to the popularity of this modality.
Keywords
Diabetes Mellitus; Diabetic Gastroparesis; Gastric emptying scintigraphy
INTRODUCTION
Diabetes is the modern age global epidemic producing significant morbidity and mortality affecting about 425 million people worldwide in 2017, and the projected figure of affected population by the year 2045 being as high as 693 million cases. The prevalence of Diabetes in India is about 72.9 million cases, which is currently second only to China and is estimated to rise to 119.8 million cases by the year 2045. Long standing diabetics are prone to develop varied complications including, but not limited to autonomic neuropathy, which may involve multiple systems including gastrointestinal, cardiovascular, genitourinary systems [1, 2].
Gastroparesis is defined as delayed gastric emptying in absence of gastric outlet obstruction. Although there are numerous causes of gastroparesis, Diabetes Mellitus remains the most common identifiable cause, overall most common cause being idiopathic. The term gastroparesis diabeticorum as given by Kassander translates to ‘stomach paralyses after incidental discovery of asymptomatic gastric retention in patients of moderate to severe diabetes. Delayed gastric emptying (GE) in Diabetes may arise due to antral hypomotility and/or pylorospasm which is attributed to either vagal neuropathy or enteric neuromuscular dysfunction. Cardinal symptoms of gastroparesis are nausea, vomiting, early satiety, upper abdominal pain, post prandial fullness, and bloating and weight loss. Diabetic Gastroparesis (DG) may significantly affect quality of life and also poses a risk of hypoglycemic and hyperglycemic fluctuations in these patients due to improper emptying of ingested food into the duodenum. Gastric emptying studies for solids is more sensitive for detecting gastroparesis than for liquids as liquid emptying remains normal till advanced stages of disease.Although, most of the focus has been on delayed GE, Diabetes may also result in rapid gastric emptying, which may also result from vagal neuropathy[3-5].
Diagnosis of gastroparesis
In addition to severity of symptoms and nutritional status of the patient, the magnitude of delayed Gastric emptying is pivotal in planning management of DG. Several diagnostic modalities have been utilized for objective evaluation of gastric emptying viz. Gastric emptying scintigraphy (GES), 13[C] Spirulina breath test, Ultrasonography, paracetamol absorption technique, wireless motility capsule, MRI, and gastroduodenal manometry. However, GES is considered the “gold standard” for evaluating gastric emptying as it is physiological, noninvasive, quantifiable study, which objectively quantifies the magnitude of gastric retention and aids in more precise assessment of gastric motility. Although 13[C] Spirulina breath test has shown strong correlation with results of simultaneously performed GES and is more popular with the gastroenterologists, its utility may be limited by faulty results/artefacts arising due to lung or lung diseases and intestinal malabsorption diseases. GES has been extensively used in clinical practice as well as in research[3, 6-9].
Impact of gastroparesis
The available data indicates that hospitalizations related to gastroparesis (including that of diabetic etiology) has been rising since past 3 decades. Also, patients of Type 1 DM with gastroparesis need more hospitalizations compared to patients of idiopathic gastroparesis. Gastroparesis results in impairment of quality of life (QoL) as indicated by lower mental and physical components of SF-36 scoring compared to population norms and greater symptom severity is inversely related to QoL. The mental health and physical functioning in patients of DG is poorer compared to that of Idiopathic gastroparesis. The effect of gastroparesis on mental health is comparable to that of active inflammatory bowel disease and lower than that of rheumatoid arthritis. Gastroparesis also results in increased mortality with lower 5-year survival than the overall community population, among which survival was lower in patients of diabetic gastroparesis[10, 11].
Factors affecting Diabetic Gastroparesis
Several characteristics are thought to affect the gastric emptying in diabetics, like gender, glycemic control, duration of diabetes, type of diabetes, BMI, etc. but different studies conducted at different centres across the globe have revealed contrasting results about the effect of these characteristics on GE. Population based data for Gastroparesis is scarce and much of the available data is derived from hospital based studies.
In the population based studies conducted among Diabetics to evaluate gastroparesis by scintigraphy, women had higher incidence of gastroparesis than men, with incidence of 30-40%[11]. In a hospital based study by [12], investigators found delayed GE in 29% and rapid GE in 2% of the 140 patients of Type 2 Diabetes Mellitus. They concluded that presence and severity of clinical features do not predict delayed GE. HbA1c and BMI were independent predictors of delayed GE. In addition, delayed GE was also associated with microvascular and macrovascular complication of diabetes and increased risk of hypoglycemic episodes[12]. In their retrospective study which included 129 patients of type 1 and type 2 diabetes mellitus found 36% of the patients had delayed GE and 22% patients had rapid GE. However, delayed or rapid GE were not related to the type and duration of Diabetes, or HbA1c[13, 14]retrospectively reviewed 108 patients of type1 and 2 diabetes mellitus who underwent GES and found that 56% of the patients had abnormal findings in GE (rapid emptying in 37%, and delayed emptying in 19% of the patients). Also, UGI symptoms were associated with gastric motor dysfunction. No significant association was found between Diabetic triopathy, duration of diabetes, and glycemic control with abnormal GE[14]. [15] studied 19 patients of type 2 Diabetes Mellitus and 6 healthy volunteers, and the results of their study revealed that gender, age, and duration of Diabetes had no significant statistical correlation with GE, while HbA1c levels had positive correlation with GE time (p<0.05), also the gastric emptying time in the studied diabetic population was significantly slower than normal subjects(p<0.05)[15].[16] in their prospective study which included 78 patients of Type 1 DM, and 59 patients of type 2 DM found that Type 1 DM patients had slower gastric emptying, more hospitalizations, more gastric stimulator implantations, higher HbA1c and more anxiety than Type 2 DM patients. Moreover, the GI symptom scores decreased only in type 2 DM patients but not in type 1 DM patients on follow up at 48 weeks. This study also revealed that gastrointestinal symptoms at baseline and follow up at 48 weeks in both type 1 DM and type 2 DM were not associated with HbA1c, peripheral neuropathy, psychological factors, and Quality of Life [16]. [17]Studied 34 patients of Diabetes to find out the relationship between gastric emptying and other characteristics and complications of Diabetes. Their study revealed no significant difference between gastric emptying and gastrointestinal symptoms. However, the prevalence of autonomic neuropathy was found to be higher in the group with delayed T1/2 of the whole stomach emptying. They also concluded that intima-media thickness of the carotid bulb was significantly greater in the group of patients with delayed gastric emptying[17]. [18]Studied 82 normal subjects and 16 type 2 diabetes mellitus patients for relationship of early and late glycemic responses with gastric emptying during an oral glucose tolerance test with 75g glucose drink labeled with 99mTc-sulfur colloid. They found no difference in GE in the two groups [18]. [19] carried out a study involving 198 gastroparetic patients (134 of Idiopathic gastroparesis, 64 of Diabetic Gastroparesis) for assessing correlation between gastroparesis severity (by filling out questionnaires) and gastric emptying as assessed by scintigraphy. The study revealed that increasing severity of early satiety and post prandial fullness was associated with increased severity of gastroparesis and increased gastric retention of a solid meal[19] (Table 1).
|
Study |
Participants |
Key findings |
|
Izzy M et al.2017 [20] |
299 patients of Type 1 and Type 2 DM |
· Poor glycemic control is associated with delayed gastric emptying. · No significant association of age, gender, or type of DM with 4h gastric retention values.
|
|
Anudeep V et al. 2016 (12) |
140 patients of Type 2 DM |
· HbA1c and BMI are independent predictors of delayed GE. · Presence and severity of symptoms of gastroparesis do not predict delayed GE. · Delayed GE associated with increased risk of hypoglycemic episodes. |
|
Bharucha et al.2008 (13) |
129 patients of Type 1 and Type 2 DM |
· Significant weight loss and neuropathy are risk factors for delayed and rapid GE respectively. · Type and duration of DM, HbA1c, extra intestinal complications not associated with delayed or rapid GE. |
|
Chedidet al.2019 (14) |
108 patients of Type 1 and Type 2 DM |
· Testing for gastric emptying and gastric accommodation aids in targeted individualized treatment. |
Table 1: Major Hospital based studies and their key findings utilizing GES in Diabetics
PROCEDURE OF GES
Patient Preparation
Patients planned for GES are advised for overnight fasting, however, if overnight fasting is not possible for any reason, fasting for at least 6 hours is recommended before the test. However, patients may take their medications with some water. After interviewing, examining, explaining the procedure, and obtaining informed consent, patient is administered radiolabeled meal followed by serial imaging. Patient is counseled not ingest any additional food and liquids and also refrain from smoking till the study is completed.
Meal
Consensus report from the American Neurogastroenterology and motility society and Society of Nuclear Medicine has proposed a standard method of procedure for GES, and meal described in this consensus report proposes a low fat meal for initial screening test for GE[6]. Egg-white sandwich(EWS) radio labeled with 99mTc is commonly used meal in the western countries. However, other radiolabeled meals have also been standardized and used for GES as EWS may not be an acceptable meal for all. Radiolabeled idli (savory cake) meal can be a good alternative to EWS as >96% of 99mTc sulfur colloid remains bound to the meal after 4 hours of suspension in simulated gastric fluid. This alternative is especially useful in patients who have specific dietary restrictions. [21]. RadiolabeledChapati (Indian round bread) has also been standardized and administered for GES with 90% of the radiolabel bound to meal at all pH levels up to 3 hours[21,22].
Acquisition and Interpretation:
Results of multiple studies show that imaging up to 4 hours post meal administration and quantifying gastric retention to be more appropriate than previously thought varied durations of 60 min to 2 hours, and T1/2(time taken for half emptying of meal from stomach)(Figure 1).Hence, the guidelines recommend optimal time of imaging after meal is immediately, 1h, 2h, and 4h. Gastric retention of >60% of the meal at 2 h and/or >10% of the meal at 4 h is outside the range of >95% of healthy individuals and these cut-off values are therefore used to confer a diagnosis of gastroparesis[6] (Figure. 2).
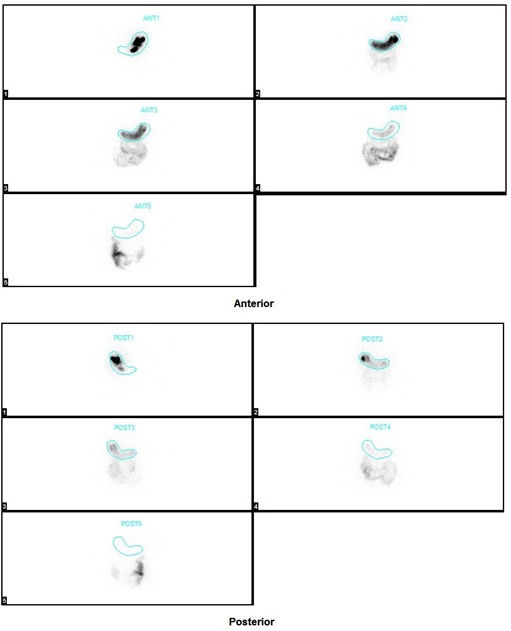
Figure 1: Anterior and Posterior images of Gastric Emptying Scintigraphy after administration of radiolabeled solid Idli meal in a 60 year old male patient of Type 2 Diabetes Mellitus of 27 years’ duration. After administration of radiolabeled meal, images were acquired immediately, at 30 minutes, 1 h, 2h, and 4 h. Entire tracer is seen in the stomach in the first image and is seen passing gradually into intestines. Images at 4 h reveal normal gastric emptying (retention ~1%).
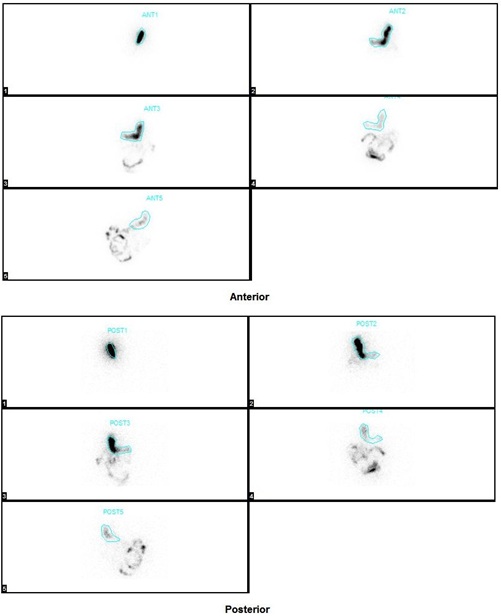
Figure 2: Anterior and Posterior images of Gastric Emptying Scintigraphy of 47 year old male patient of Type 2 Diabetes Mellitus of 10 years’ duration. After administration of radiolabeled meal, images were acquired immediately, at 30 minutes, 1 h, 2h, and 4 h. Entire tracer is seen in the stomach in the first image. Images at 4 h reveal delayed gastric emptying (retention ~ 29%).
LIMITATIONS:
It has been observed that acute hyperglycemia may alter gastric emptying, so it is appropriate to check Fasting Blood Glucose and ensure values of <275 mg/dl before beginning GES[3].Certain drugs may act as confounding factors in GES as they might alter gastric motility. These may GLP-1 analogues (e.g. exenatide), DPP-4 inhibitors (e.g. sitagliptin), prokinetic drugs (such as cisapride), other drugs like erythromycin, opiates, tricyclic antidepressants, calcium channel blokers, etc. Therefore, a detailed drug history is imperative before beginning the GES, and stopping these drugs for certain time period before GES is prudent for more accurate estimation of GE time, unless the drug is being prescribed for treatment of gastroparesis and GES is performed for response evaluation. Although having numerous advantages, lack of standardization of the meals used for GES, patient positioning, frequency and duration of imaging may limit the utility of this test making the results less comparable, and difficulty in interpretation across the institutions. However, these limitations can be largely overcome by performing the study by following the consensus recommendations published by an established agency or society[6, 23].
Radiation dose considerations:
The radiation dose delivered to the patient in 1 gastric emptying scintigraphy using 500microCi of 99mTc Sulfur colloid is 0.51mSv and 0.62mSv for males and females respectively the approximate effective radiation dose in one Chest X-ray is 0.1mSv.
Reproducibility of GES and its use in assessing treatment response
GES is a valuable tool in assessing response to treatment in gastroparesis. Although other indices based on symptom severity have been used widely, GES can provide deeper insight by quantifying the retention of meal in the stomach. Heckert et al.performed GES in their study of 34 patients with gastroparesis (29 idiopathic and 5 diabetic) for assessing improvement in symptoms on treatment with domeperidone at baseline and 6 weeks of treatment and found improvement in symptoms of gastroparesis[24].Studied reproducibility of GES in 60 patients with upper GI symptoms on two occasions at an average interval of 15 days and concluded that gastric emptying measured with scintigraphy is relatively reproducible[5].
DISCUSSION
Delayed gastric emptying is a known complication of Diabetes and associated with impaired quality of life and significant morbidity and mortality. Patients of DG may remain asymptomatic in presence of delayed GE. Objective measurement of GE is essential for planning management for better patient outcomes. GES is the gold standard test to evaluate DG by virtue of its simplicity and objectivity and other available diagnostic modalities either need further validation or provide only an estimate of gastric emptying. Much of the data available on gastroparesis is based on the hospital based studies. Major studies on gastroparesis and factors affecting gastroparesis have utilize GES with varied results. It is noteworthy that GES can also guide in the assessing response to therapy in patients of gastroparesis treated by pharmacological interventions or electrical stimulation, as well as screening patients for emptying who are being considered for management with certain medications (such as GLP-1 agonists) which may further delay gastric emptying as it can quantitate the emptying (and therefore retention). It is necessary to be aware of all factors which may affect the results of GES like drugs that alter gastric motility, smoking, history of gastrointestinal surgery, etc which mandates removing the avoidable confounding factors for accurate results. Similarly, meal used in the GES has been an area of debate for long and it should be kept in mind to use a validated and standardized meal to avoid any errors in estimating gastric emptying. Egg white based meal as mentioned in consensus recommendations may not be useful in all settings due to unavailability of ready-made marketed products like “Egg beaters”, and it becomes necessary to use meals which is acceptable to the participants belonging to a particular region. Many such meals including Idli, Chapati, Oatmeal, etc have been validated and used for GES. For obtaining best results, it is prudent to follow consensus recommendations/guidelines while performing GES. This ensures repeatability and validity of GES.
FUTURE DIRECTIONS
Diabetic Gastroparesis in a major problem worldwide and it can be effectively evaluated with scintigraphy techniques, major advantage being that the evaluation involves imaging in a physiological environment and is reproducible. However, larger multicentric studies are needed to evaluate various factors affecting GE in Diabetes as various existing studies examining different parameters have conflicting results in terms of various factors and their effect of GE. Various types of meals suited to regional dietary habits need to be validated on a larger population before using them as standard meal.
REFERENCES
- Federation ID(2017) IDF Diabetes Atlas Eighth edition. International Diabetes Federation. IDF Diabetes Atlas, 8th (edn.). Brussels, Belgium.
- Diabetes [Internet]. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes
- Parkman HP (2015)Yamada’s Textbook of Gastroenterology(6thedn.). Podolsky D, Camilleri M, Fitz GJ, Kalloo AN, Shanahan F, Wang TC (Eds). Wiley Blackwell; 1005–31.
- Brownlee M, Aiello LP, Cooper ME, Vinik AI, Plutzky J, Boulton AJM (2016) Complications of Diabetes Mellitus(13thedn.). Melmed S, Polonsky KS, Larson PR, Kronenberg HM(Eds.). Williams Textbook of Endocrinology. Philadelphia, PA. Elsevier 1484–1581.
- Desai A, O’Connor M, Neja B, Delaney K, Camilleri M, Zinsmeister AR, etal.(2018) Reproducibility of gastric emptying assessed with scintigraphy in patients with upper GI symptoms. Neurogastroenterol Motil10: 13365.
- Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, Maurer AH, etal.(2008) Consensus recommendations for gastric emptying scintigraphy: A joint report of the American neurogastroenterology and motility society and the society of nuclear medicine. In: American Journal of Gastroenterology 3: 753-63.
- Phillips LK, Rayner CK, Jones KL, Horowitz M (2014) Measurement of gastric emptying in diabetes. Journal of Diabetes and its Complications6: 894-903.
- Grover M, Farrugia G, Stanghellini V (2019) Gastroparesis: A turning point in understanding and treatment. Gut 12: 2238-2250.
- Knight LC (2012) Update on gastrointestinal radiopharmaceuticals and dosimetry estimates. Seminars in Nuclear Medicine 2: 138–144.
- Woodhouse S, Hebbard G, Knowles SR (2017) Psychological controversies in gastroparesis: A systematic review. World Journal of Gastroenterology7: 1298–309.
- Adil E. Bharucha, Yogish C. Kudva DOP (2019) Diabetic Gastroparesis. Endocr Rev 5:1318–52.
- Anudeep V, Vinod KV, Pandit N, Sharma VK, Dhanapathi H, Dutta TK, et al. (2016) Prevalence and predictors of delayed gastric emptying among Indian patients with long-standing type 2 diabetes mellitus. Indian J Gastroenterol5: 385-392.
- Bharucha AE, Camilleri M, Forstrom LA, Zinsmeister AR (2009) Relationship between clinical features and gastric emptying disturbances in diabetes mellitus. ClinEndocrinol (Oxf)3: 415–420.
- Chedid V, Brandler J, Vijayvargiya P, Park SY, Szarka LA, Camilleri M (2019) Characterization of Upper Gastrointestinal Symptoms, Gastric Motor Functions, and Associations in Patients with Diabetes at a Referral Center. Am J Gastroenterol1: 143-154.
- Javadi H, Bayani H, Mogharrabi M, Pashazadeh AM, Semnani S, Alipour Z, et al. (2015) Relation between clinical features and gastric emptying time in diabetic patients. Nucl Med Rev1:3-6
- Koch KL, Hasler WL, Yates KP, Parkman HP, Pasricha PJ, Calles-Escandon J, et al. (2016) Baseline features and differences in 48 week clinical outcomes in patients with gastroparesis and type 1 vs type 2 diabetes. Neurogastroenterol Motil 7: 1001-15.
- Kotani K, Kawabe J, Kawamura E, Kawano N, Emoto M, Yoshida A, et al. (2014) Clinical assessment of delayed gastric emptying and diabetic complications using gastric emptying scintigraphy: Involvement of vascular disorder. ClinPhysiolFunct Imaging 2: 151-8.
- Marathe CS, Horowitz M, Trahair LG, Wishart JM, Bound M, Lange K, et al. (2015) Relationships of early and late glycemic responses with gastric emptying during an oral glucose tolerance test. J ClinEndocrinolMetab9: 3565-71.
- Parkman HP, Hallinan EK, Hasler WL, Farrugia G, Koch KL, Nguyen L, et al. (2017) Early satiety and postprandial fullness in gastroparesis correlate with gastroparesis severity, gastric emptying, and water load testing. Neurogastroenterol Motil 4.
- Izzy M, Lee M, Johns-Keating K, Kargoli F, Beckoff S, Chun K, et al. (2018) Glycosylated hemoglobin level may predict the severity of gastroparesis in diabetic patients. Diabetes Res ClinPract 135:45-49.
- Somasundaram VH, Subramanyam P, Palaniswamy SS (2014)A gluten-free vegan meal for gastric emptying scintigraphy?: Establishment of reference values and its utilization in the evaluation of diabetic gastroparesis. Clin Nucl Med11: 960-5.
- AwasthiVD, Sewatkar AB, Gambhir S, Mittal B DB (1992) Gastric emptying in normal adult males: A radionuclide study. Indian J Pharmacol 24:238–40.
- Bharucha AE, Batey-Schaefer B, Cleary PA, Murray JA, Cowie C, Lorenzi G, et al. (2015) Delayed gastric emptying is associated with early and long-term hyperglycemia in type 1 diabetes mellitus. Gastroenterology. 2: 330-9.
- Heckert J, Parkman HP (2018) Therapeutic response to domeperidone in gastroparesis: A prospective study using the GCSI-daily diary. Neurogastroenterol Motil 1.
Citation: Vandana K Dhingra (2020) Gastric Emptying Scintigraphy in the Management of Diabetic Gastroparesis: A Brief Review of Literature. J Nucl Med Radiol Radiat Ther 5: 018.
Copyright: © 2020 Sanchay Jain, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.