Journal of Nephrology & Renal Therapy Category: Clinical
Type: Case Report
Gastroparesis Secondary to a Large Renal Cyst in a Patient with ADPKD: A Case Report
*Corresponding Author(s):
Theodore I SteinmanDivision Of Nephrology, Beth Israel Deaconess Medical Center, Boston, MA, United States
Tel:+1 6176675278,
Fax:+1 61797855595
Email:tsteinma@bidmc.harvard.edu
Received Date: Sep 08, 2017
Accepted Date: Oct 27, 2017
Published Date: Nov 10, 2017
Abstract
Autosomal Dominant Polycystic Kidney Disease (ADPKD) is characterized by cystic enlargement of the kidneys and has rarely been reported to cause mechanical bowel obstruction. Here, we document the first case of gastroparesis related to a kidney cyst. We describe a 60 year old female with a history of ADPKD who was referred with one year of intractable nausea and vomiting with oral intake, chronic right side abdominal pain, 25 pound weight loss and malnutrition. Multiple CT scans revealed a large cyst in the right kidney directly abutting, but not occluding, the gastric outlet. Upper endoscopy ruled out an anatomic lesion that could cause luminal obstruction. Two gastric emptying studies confirmed the diagnosis of gastroparesis, characterized by a clinically significant delay in gastric emptying. After thorough evaluation the approach taken was laparoscopic decortication of the large single cyst. At the three month follow-up, she is having an unrestricted diet without need for anti-emetic or analgesic medications. Four months post-procedure a repeat gastric emptying study demonstrated normal gastric motility. Decortications of the cyst have provided permanent relief of her symptoms over 18 months of follow up. We hypothesize the large renal cyst was an irritant to the nerve plexus responsible for gastric motility in the distal stomach.
Keywords
Renal Cyst; Gastroparesis
INTRODUCTION
Autosomal Dominant Polycystic Kidney Disease (ADPKD) is the most common inherited renal disorder and is characterized by progressive cystic enlargement of the kidneys that results in End Stage Renal Disease (ESRD) in about 50% of the affected population [1]. Common renal complications include nephrolithiasis and cyst hemorrhage/infection/rupture; all of which can cause varying pain patterns. Additionally, kidney size and liver involvement can cause abdominal distension, back pain and early satiety [2]. Rarely, cystic kidneys have been reported to cause mechanical obstruction of the bowel. Kakinoki et al., [3] reviewed 5 cases of bowel obstruction secondary to renal cysts. Patients in this series ranged from a neonate to 64 years old. Nephrectomy was performed in three of the five cases, a fourth patient died of ESRD without intervention and the fifth underwent ultrasound guided cyst aspiration with resolution of symptoms.
Gastroparesis is a clinical syndrome characterized by nausea, vomiting, early satiety, bloating and upper abdominal pain with objective evidence of delayed gastric emptying in the absence of mechanical obstruction. Most cases are due to diabetic autonomic neuropathy, surgical nerve injury or deemed idiopathic. Less common etiologies include viral infections, medications, autoimmune disorders and neurodegenerative disorders [4]. As described, ADPKD has been associated with small bowel obstruction, but an association with gastroparesis has never been previously reported. We report the first case of confirmed gastroparesis associated with a renal cyst in a patient with ADPKD.
Gastroparesis is a clinical syndrome characterized by nausea, vomiting, early satiety, bloating and upper abdominal pain with objective evidence of delayed gastric emptying in the absence of mechanical obstruction. Most cases are due to diabetic autonomic neuropathy, surgical nerve injury or deemed idiopathic. Less common etiologies include viral infections, medications, autoimmune disorders and neurodegenerative disorders [4]. As described, ADPKD has been associated with small bowel obstruction, but an association with gastroparesis has never been previously reported. We report the first case of confirmed gastroparesis associated with a renal cyst in a patient with ADPKD.
CASE REPORT
A 60 year old woman with a history of ADPKD was referred to our clinic for evaluation of intractable nausea and vomiting with oral intake, chronic right-sided abdominal pain, 25 pound weight loss and malnutrition of one year duration. A detailed history revealed her Gastrointestinal (GI) symptoms were frequently associated with a documented Urinary Tract Infection (UTI). Initial improvement of these symptoms was noted after treatment of her UTI, but a relapse of GI symptoms occurred usually within a few weeks. Over the next several months she evolved into a pattern of increased frequency of severe episodes of nausea and vomiting with any oral intake, unrelated to a recurrent UTI. Moderate intensity right sided abdominal and flank pain, not correlated with the continued nausea and vomiting with oral intake, occurred in a waxing and waning pattern. Her symptoms precipitated weekly emergency department evaluations, most often requiring Intravenous Fluid Volume expansion (IVF) and electrolyte repletion. Her symptoms would resolve with the volume/electrolyte repletion, bowel rest and symptomatic management. Empiric treatment of her symptoms was with opioid, anxiolytic and anti-emetic medications. Multiple abdominal CT scans were performed, without evidence of bowel or gastric obstruction, ileus, volvulus or other definable gastric pathology. A gastric emptying study, performed at an outside hospital, was abnormally delayed, leading to a diagnosis of gastroparesis.
Her medical history was significant for her known ADPKD, hypertension and a hysterectomy at age 42 (complicated by an intra-abdominal infection and subsequent ventral hernia). Anti-hypertensive medications included Lisinopril, Torsemide, Nifedipine, and she used Lorazepam as needed. Our initial evaluation documented a blood pressure of 112/70 mmHg sitting, 106/74 mmHg standing, with a regular pulse of 100 bpm. She appeared chronically ill and in moderate distress from nausea. The examination of multiple palpable renal cysts and reproducible pinpoint tenderness to palpation in the upper-mid right abdomen region was significance. Laboratory studies revealed a BUN 8 mg/dL, Cr 0.7 mg/dL, K 3.5 mEq/L, Mg 1.4 mg/dL, PO4 1.8 mg/dL and albumin 2.9 g/dL. She had normal blood glucose and hemoglobin A1C values.
Two days after our initial evaluation, she attended the same hospital with recurrent nausea and vomiting. The first CT scan results revealed a 9.3cm x 6.5cm cyst in the upper pole of the right kidney directly abutting the gastric outlet, but not occluding it (Figure 1). Again, there was no evidence of gastric or bowel obstruction (that would explain her symptoms), and she was admitted for IVF, electrolyte repletion and symptomatic management. During NPO her symptoms resolved again. She refused a feeding tube because of her concern with recurrent/persistent GI symptoms precipitated by anything going in to her stomach. Because of her progressive malnutrition and inability to tolerate oral intake, Total Parenteral Nutrition (TPN) was initiated. Upper endoscopy (EGD) on day 5 was performed into the jejunum and revealed thickened antral folds, but no evidence of luminal obstruction, A 4 hour gastric emptying study, utilizing Tc-99m water labeled with sulfur colloid, was performed on day 10 after withdrawal of her calcium channel blocker for 10 days, and narcotics and anti-emetics for 48 hours. The test elicited her usual GI symptoms with only 300ml liquid intake and showed a half emptying time of 34.3 minutes (normal less than 19 minutes). An endoscopic ultrasound was performed on day 13 to evaluate the antral findings seen on prior EGD and was unrevealing (no intrinsic compression). A diagnosis of gastroparesis was thus confirmed. After review of imaging and interdisciplinary discussion between nephrology, urology and gastroenterology services, it was decided that the large right renal cyst was likely contributing to the patient’s symptoms. Laparoscopic decortication of the large right renal cyst and 6 to 8 smaller adjacent cysts was performed without complications. She was discharged the next day after overnight observation. After the laparoscopic decortication of her right upper pole kidney cysts, her diet was slowly advanced and she did not require analgesic or anti-emetic medications. Within one week after cysts decortication she was tolerating a bland, solid diet in small amounts. After one month, her right sided abdominal pain was decreased and her oral intake continued to improve. TPN was discontinued by 2 months (after full nutritional repletion and she was now tolerating full meals). After 3 months post-procedure she had a non-edematous weight gain of 15 lbs, albumin increasing to 4.4 g/dl and creatinine increasing to 1.2 mg/dl (reflecting her improved nutritional status). Approximately 4 months after surgery, a repeated 4 hour gastric emptying study was performed utilizing Tc-99m egg whites labelled with sulfur colloid and a standard egg white, toast, jelly and water meal. Resolution of her gastroparesis was demonstrated by: 1) A normal gastric emptying time; 2) A normal plateau period and 3) Followed by rapid gastric emptying with only 3% of ingested material remaining at 4 hours (a dramatic improvement when compared to her two studies performed before cyst decortication). All signs of malnutrition were completely resolved after cysts decortication procedure.
Her medical history was significant for her known ADPKD, hypertension and a hysterectomy at age 42 (complicated by an intra-abdominal infection and subsequent ventral hernia). Anti-hypertensive medications included Lisinopril, Torsemide, Nifedipine, and she used Lorazepam as needed. Our initial evaluation documented a blood pressure of 112/70 mmHg sitting, 106/74 mmHg standing, with a regular pulse of 100 bpm. She appeared chronically ill and in moderate distress from nausea. The examination of multiple palpable renal cysts and reproducible pinpoint tenderness to palpation in the upper-mid right abdomen region was significance. Laboratory studies revealed a BUN 8 mg/dL, Cr 0.7 mg/dL, K 3.5 mEq/L, Mg 1.4 mg/dL, PO4 1.8 mg/dL and albumin 2.9 g/dL. She had normal blood glucose and hemoglobin A1C values.
Two days after our initial evaluation, she attended the same hospital with recurrent nausea and vomiting. The first CT scan results revealed a 9.3cm x 6.5cm cyst in the upper pole of the right kidney directly abutting the gastric outlet, but not occluding it (Figure 1). Again, there was no evidence of gastric or bowel obstruction (that would explain her symptoms), and she was admitted for IVF, electrolyte repletion and symptomatic management. During NPO her symptoms resolved again. She refused a feeding tube because of her concern with recurrent/persistent GI symptoms precipitated by anything going in to her stomach. Because of her progressive malnutrition and inability to tolerate oral intake, Total Parenteral Nutrition (TPN) was initiated. Upper endoscopy (EGD) on day 5 was performed into the jejunum and revealed thickened antral folds, but no evidence of luminal obstruction, A 4 hour gastric emptying study, utilizing Tc-99m water labeled with sulfur colloid, was performed on day 10 after withdrawal of her calcium channel blocker for 10 days, and narcotics and anti-emetics for 48 hours. The test elicited her usual GI symptoms with only 300ml liquid intake and showed a half emptying time of 34.3 minutes (normal less than 19 minutes). An endoscopic ultrasound was performed on day 13 to evaluate the antral findings seen on prior EGD and was unrevealing (no intrinsic compression). A diagnosis of gastroparesis was thus confirmed. After review of imaging and interdisciplinary discussion between nephrology, urology and gastroenterology services, it was decided that the large right renal cyst was likely contributing to the patient’s symptoms. Laparoscopic decortication of the large right renal cyst and 6 to 8 smaller adjacent cysts was performed without complications. She was discharged the next day after overnight observation. After the laparoscopic decortication of her right upper pole kidney cysts, her diet was slowly advanced and she did not require analgesic or anti-emetic medications. Within one week after cysts decortication she was tolerating a bland, solid diet in small amounts. After one month, her right sided abdominal pain was decreased and her oral intake continued to improve. TPN was discontinued by 2 months (after full nutritional repletion and she was now tolerating full meals). After 3 months post-procedure she had a non-edematous weight gain of 15 lbs, albumin increasing to 4.4 g/dl and creatinine increasing to 1.2 mg/dl (reflecting her improved nutritional status). Approximately 4 months after surgery, a repeated 4 hour gastric emptying study was performed utilizing Tc-99m egg whites labelled with sulfur colloid and a standard egg white, toast, jelly and water meal. Resolution of her gastroparesis was demonstrated by: 1) A normal gastric emptying time; 2) A normal plateau period and 3) Followed by rapid gastric emptying with only 3% of ingested material remaining at 4 hours (a dramatic improvement when compared to her two studies performed before cyst decortication). All signs of malnutrition were completely resolved after cysts decortication procedure.
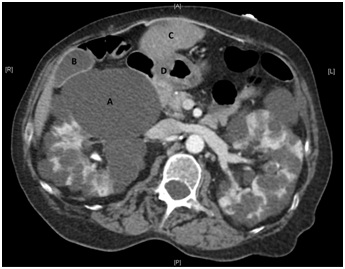
Figure 1: CT of Abdomen and Pelvis with Iodinated Contrast Coronal View.
A: Large right renal cyst measuring 9.3cm x 6.5cm in greatest dimension
B: Gallbladder
C: Liver
D: Pylorus
B: Gallbladder
C: Liver
D: Pylorus
DISCUSSION
ADPKD is the most common inherited form of progressive renal failure and associated with numerous complications. Here we describe the first documented case of gastroparesis related to ADPKD. On imaging and during laparoscopic surgery, the large right renal cyst was noted to be protruding from behind and under the gallbladder and abutting the gastric outlet. This is a tight anatomic area containing several arteries and nerves essential for the function of the stomach and duodenum.
The innervation of the stomach, pyloric region and duodenum derives ultimately from the vagus nerve distribution. Cadaveric dissection has demonstrated the innervations of the pyloric area and antrum arrives via three main routes [5]. First, a plexus originating from the hepatic vagal plexus and ultimately the anterior vagal trunk arrive via the right gastric artery and superior pyloric artery, which innervates the superior portion of the pylorus and antrum. Second, nerves also originating from the anterior hepatic plexus arrived via the gastroduodenal and infrapyloric artery, supplying the inferior and posterior portions of the pylorus and antrum. The third route is the anterior and posterior gastric nerves coursing along the lesser curvature of the stomach.
The large right renal cyst, located under the liver and gallbladder, was abutting the duodenum. The gastric outlet may have been gradually impeded by the enlarging cyst, but the gastric outlet was not totally occluded by either intrinsic or extrinsic compression. An offered hypothesis is that irritation of nerves supplying the duodenum, pylorus and gastric antrum, which arrive via the right gastric and gastroduodenal arteries, and course through the hepatoduodenal and hepatogastric ligaments, was the pathophysiologic cause of her problem. Dysfunctional peristalsis with delayed gastric emptying was the cause for gastroparesis, not mechanical obstruction of the bowel lumen. As we did not perform manometry, autonomic testing or electrogastrogram, we cannot definitively state the ultimate etiology of the gastroparesis. However, given the rapid and dramatic clinical improvement following cyst decortication, supported by definitive lab testing and normalization of the gastric emptying study, the above proposed consequences of her large right renal cyst(s) are implicated as the cause of her gastroparesis.
This case demonstrates that unexplained symptoms, even if not typical of ADPKD, should be fully and carefully evaluated for relation to renal cystic disease, especially as they may be amenable to procedural cure.
The innervation of the stomach, pyloric region and duodenum derives ultimately from the vagus nerve distribution. Cadaveric dissection has demonstrated the innervations of the pyloric area and antrum arrives via three main routes [5]. First, a plexus originating from the hepatic vagal plexus and ultimately the anterior vagal trunk arrive via the right gastric artery and superior pyloric artery, which innervates the superior portion of the pylorus and antrum. Second, nerves also originating from the anterior hepatic plexus arrived via the gastroduodenal and infrapyloric artery, supplying the inferior and posterior portions of the pylorus and antrum. The third route is the anterior and posterior gastric nerves coursing along the lesser curvature of the stomach.
The large right renal cyst, located under the liver and gallbladder, was abutting the duodenum. The gastric outlet may have been gradually impeded by the enlarging cyst, but the gastric outlet was not totally occluded by either intrinsic or extrinsic compression. An offered hypothesis is that irritation of nerves supplying the duodenum, pylorus and gastric antrum, which arrive via the right gastric and gastroduodenal arteries, and course through the hepatoduodenal and hepatogastric ligaments, was the pathophysiologic cause of her problem. Dysfunctional peristalsis with delayed gastric emptying was the cause for gastroparesis, not mechanical obstruction of the bowel lumen. As we did not perform manometry, autonomic testing or electrogastrogram, we cannot definitively state the ultimate etiology of the gastroparesis. However, given the rapid and dramatic clinical improvement following cyst decortication, supported by definitive lab testing and normalization of the gastric emptying study, the above proposed consequences of her large right renal cyst(s) are implicated as the cause of her gastroparesis.
This case demonstrates that unexplained symptoms, even if not typical of ADPKD, should be fully and carefully evaluated for relation to renal cystic disease, especially as they may be amenable to procedural cure.
REFERENCES
- Torres VE, Harris PC, Pirson Y (2007) Autosomal dominant polycystic kidney disease. Lancet 369: 1287-1301.
- Bajwa ZH, Gupta S, Warfield CA, Steinman TI (2001) Pain management in polycystic kidney disease. Kidney Int 60: 1631-1644.
- Kakinoki K, Noda Y, Takaeda M, Kubo M, Mizuhashi K, et al., (2002) Intestinal obstruction in autosomal dominant polycystic kidney disease. Intern Med 41: 441-444.
- Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L (2013) Clinical guideline: management of gastroparesis. Am J Gastroenterol 108: 18-37.
- Yi SQ, Ru F, Ohta T, Terayama H, Naito M, et al., (2006) Surgical anatomy of the innervation of pylorus in human and Suncus murinus, in relation to surgical technique for pylorus-preserving pancreaticoduodenectomy. World J Gastroenterol 12: 2209-2216.
Citation: DeWolfe D, Raman V, Wagner A, Rabb J, Steinman TI (2017) Gastroparesis Secondary to a Large Renal Cyst in a Patient with ADPKD: A Case Report. J Nephrol Renal Ther 3: 015.
Copyright: © 2017 Theodore I Steinman, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Journal Highlights
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!
