
Head Massage Therapy More Efficacious Than Mechanical Helmet Massager to Stimulate Parasympathetic Cardiac Tone: A Randomized Cross-Over Trial
*Corresponding Author(s):
Ling GuanChina National Clinical Research Center For Neurological Diseases, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
Email:lguanm@hotmail.com
Jean-Paul Collet
British Columbia Children’s Hospital Research Institute, Vancouver, Canada
Tel:+1 6049996860,
Email:jcollet@bcchr.ca
Abstract
Objective: To compare the respective efficacy of head massage performed by Chinese head massage therapist and by mechanical helmet massager on Heart Rate Variability (HRV) and clinical parameters.
Design: A randomized crossover trial with random allocation of Head Massage Therapy (HMT), Mechanical Helmet Massager (MHM) and Relaxed Reading (RR), as control intervention: 10 minutes intervention and 15 minutes follow-up.
Setting: Beijing Tiantan Hospital.
Subjects: Fourteen healthy volunteers.
Intervention: HMT, MHM and Relaxed Reading.
Outcome measures: HRV parameters: Total Power, High and Low Frequency power (HF and LF) as well as HFnu (normalized unit) recorded at baseline, during the 10 minutes intervention, and 5 and 15 minutes post-intervention. We also assessed changes in heart rate (HR), blood pressure and body tension at baseline and 15 minutes after each intervention.
Results: The increase in HF and LF was differential among the 3 interventions with a dominant increased HF after HMT and a dominant increased LF after RR, while MHM produced changes intermediate between HMT and RR. During intervention, HMT induced a positive change of HFnu by +35% (IQR: +3 to +93) in contrast to +5% after MHM (p = 0.096) and -24% after RR (p = 0.011); this difference remained significant 15 minutes after the interventions (p = 0.048). HR decreased by -5.9% (IQR: -14 to +1.5) 15 minutes after HMT, in contrast to slight increase +0.3% after RR (p = 0.035) and slight decrease -1.3% after MHM (p = 0.074). Diastolic blood pressure and body tension decreased the most after HMT and we found correlations between increased HFnu and decrease of both diastolic pressure and body tension.
Conclusion: HMT shows a stronger effect on the parasympathetic nervous system as expressed by increase in HFnu with decrease in HR, diastolic blood pressure and body tension, compared with RR and also MHM. More studies are needed to understand how different relaxing interventions may modulate the autonomic nervous system.
Keywords
Autonomic Nervous System; Cross-over trial; Head Massage; HRV; Mechanical Helmet Massager; Parasympathetic; Vagus Nerve Stimulation
Clinical Trials Registration number
NCT04341649
Introduction
Body massage is integral part of complementary and alternative medicine for the care of many conditions such as asthma, chronic pain or Parkinson disease [1-6]. Nursing organizations recommend massage as having “Many Benefits, Little Risk” [7]. The effects of massage can be observed all along the life span from children [1,8] to elderly [6,9], triggering body relaxation, enhancing sleep quality [5,10] and reducing blood pressure [11,12] through stimulating the Parasympathetic Nervous System (PNS) and relaxing the Sympathetic Nervous System (SNS) [8].
From a functional perspective, the PNS effects on emotions, cognition, various physiological functions and health can be explained by the neurovisceral integration model presented by Thayer et al. in 2009 [13]. This model shows how prefrontal cortex and different subcortical regions communicate with each other to regulate PNS through a functional central autonomic network that links prefrontal cortex to the heart [14]. At heart level, Vagus tone decreases heart rate and increases beat to beat variability, leading to Heart Rate Variability (HRV) analyses [15, 16].
Among the different types of body massage techniques, Head Massage Therapy (HMT) has shown specific efficacy on stimulating the PNS [17]. HMT however, has several limitations related to the short effects’ duration of a single session, the need of a therapist, and the related cost. In this context, the use of mechanical Helmet Massager (MHM) may have some advantage to stimulate the Vagus nerve while offering convenience and flexibility at a fixed cost.
This cross-over trial was designed to compare the effectiveness of Chinese HMT and BREO inc., a commercial mechanical helmet massager. To our knowledge it is the first randomized trial comparing the effects of HMT and MHM on Autonomic Nervous System (ANS).
Materials And Methods
Study design
This cross-over trial recruited healthy volunteers to be randomly allocated to HMT and MHM interventions that may stimulate the Vagus nerve, compared to a controlled Relaxed Reading (RR) intervention. The study was approved by Tiantan Hospital Ethics Board affiliated to Capital Medical University, in Beijing, China (KY 2020-018-01).
Participants
Healthy volunteers aged 20 to 40 were invited to participate if they did not take drugs that affect the nervous system and did not have a chronic condition that required specific care. These volunteers, male or female, had to be non- or light smokers (
Laboratory setting for recording
Each volunteer was assigned to a random combination of the three interventions. All the sessions were performed in the same quiet room, at the same time of the day (+/- 1 hour) to decrease the possible effects of circadian variations on HRV parameters, and participants were assisted by the same examiner that followed the same protocol. Before starting, participants were told that the intervention would last about 30 minutes and they were invited to turn off their cellular phone, drink a bit of water or eat an apple if needed, or go to the washroom before starting.
The intervention protocol started with 10 minutes resting in a comfortable chair without interaction. At the end of the resting period we measured heart rate (HR) and blood pressure (BP) using digital BP monitor (OMRONR); the participants were also asked the question “Presently: which score would you give to your perceived Body Tension (BT)?” using a visual analog scale from “0” (low) to “10” (high) as indicator of BT [18]. The operator started then to record HRV according to the protocol (Figure 1): 5 minutes of baseline; 10 minutes of intervention; and finally 15 minutes post-intervention resting time. At the end of the 15 minutes period we collected data regarding BT, BP and HR. In the results section we present 4 sequences of HRV analyses performed at baseline; during the 10 minutes intervention; during the first 5 minutes and the last 5 minutes segments of the post-intervention period.
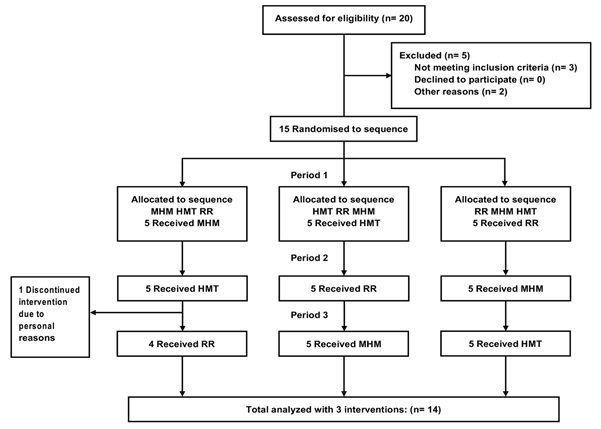 Figure 1: Timeline of the study.
Figure 1: Timeline of the study.
Interventions Procedures
Intervention 1: HMT A doctor of traditional Chinese medicine (TCM) performed a 10-minute head massage following a specific protocol involving gentle kneading and massaging of the scalp, forehead, orbital fissures, and cheeks while participants remained seated on a comfortable chair; head massage also included occipital area and part of the neck, excluding shoulders.
Intervention 2: MHM The mechanical helmet massager (USD763461-Patent BREO-Technology) was chosen by our research team as being the one that gave the strongest feeling of massaging the front head, the scalp, temporal and occipital regions, including upper neck. During the course of a massaging session, the intensity of pressure changes with alternance of deep and light pressure all over the head, with a rolling device that mimics the feeling of hand massage following muscles for relaxation. Finally, the device also provides music and a voice that guides people to relax. Although not being part of “massage” we decided to keep this element because it would be part of the device once acquired, and relaxation may also affects the ANS [18].
Intervention 3: Simple Relaxed Reading (RR) The RR intervention consisted of 10 minutes relaxation on the same chair in a quiet environment; if they wish, participants could read a local few days old newspaper.
HRV recording and analysis to assess sympathetic and parasympathetic activities
Data were collected with Biopac MP150 in segments of 5 minutes with signals sampled at 500 Hz throughout the testing. Recorded data were then reviewed manually by our HRV expert for ectopic beats or artifacts and analyzed using Acknowledge software, version 4.2 (Biopac Systems Inc.), following the recommendations from the Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology guidelines [16] and recent instructions from Laborde (2017) [19].
We assessed HRV through both the time-domain and frequency-domain analyses after fast Fourier transformation. Three frequency bands were obtained from the power-spectral analysis as follow: High Frequency Variability (HF) (0.15 to 0.4 Hz) is a marker of cardiac parasympathetic modulation, Low Frequency (LF) (0.04 – 0.15 Hz,) is under the influence of both sympathetic and parasympathetic but not fully understood regarding their respective contribution; Very Low Frequency Variability (VLF) (< 0.04 Hz) was not considered in the analysis because it is influenced by multiple factors not all identified. Total Power (TP), which represents the whole variability of RR intervals, was also calculated. Finally, we computed the normalized values of HF (HFnu) and LF (LFnu) that represent the relative values of each power component [16,20]. These values minimize the effect of changes in TP when comparing changes of HF and LF at different times, although their understanding is affected by the difficulty to interpret LF’s meaning [19,21-23].
The following time-domain parameters were computed: mean NN intervals, the Standard Deviation of mean NN intervals (SDNN), the Root-Mean-Square of Successive Differences (RMSSD), and the number of R–R intervals that differed by >50 ms from adjacent intervals divided by the total number of all R–R intervals (pNN50).
Statistical analysis
Descriptive statistics on baseline characteristics and intervention periods used medians and quartiles to report the results. Both differences from baseline to intervention and post-intervention periods and the relative percentage changes (%change) to control for the baseline differences among participants, were determined.
To compare the between-interventions changes from baseline to post-intervention, the non-parametric Wilcoxon signed-rank test was used after verification of the assumptions [24]. Finally, non-parametric Spearman’s correlation coefficient was used to assess the relationships between %change in HRV parameters and %change in clinical parameters.
In this exploratory study the main focus was to present the trends in %changes, expressed as median and Interquartile Ranges (IQR), rather than showing statistically significant results. Because of the exploratory nature and the fact that statistical tests were not independent, we did not adjust the p-values for the number of tests performed. Statistical analyses were performed using SPSS version 22.
Results
Figure 2 shows the flowchart of participants’ selection. Twenty individuals volunteered for the study. Review of the inclusion criteria excluded 5 of them for different reasons: stressful life situation (n=1), unusual workload in the emergency department (n=2), leaving Beijing (n=1) and lack of flexibility in the work schedule to be available at the same time every day (n=1). A total of 15 volunteers signed the consent form and were exposed to the different interventions. One of the participants dropped out during the study for personal reasons; related data were removed from the analysis. Finally, the study included 14 healthy individuals, with median age of 27 years, seven females and seven males, all exposed to the three interventions.
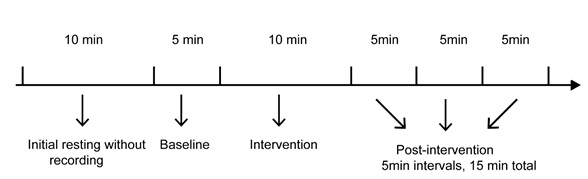 Figure 2: Timeline of the study.
Figure 2: Timeline of the study.
Within-individual changes of TP, LF and HF increased during and after each intervention (Table 1; Figure 3), with differences from baseline that were often statistically significant (p < 0.05). The largest LF absolute value was observed during the relaxed reading while HF values increased mostly during HMT. HMT increased HFnu during and after the intervention compared to baseline, while the MHM increased HFnu only during the intervention and RR showed a decrease at each time (Table 1). All three interventions were able to decrease BT, especially HMT. Table 1 also shows the consistency of changes between SDNN and TP, as well as between %p NN50 and HF.
|
Mechanical helmet massager (MHM) |
||||
|
Parameters |
Baseline
|
During intervention p-Value
|
5 minutes post intervention p-Value P-VALUEvalue
|
15 minutes post intervention p-Value P value
|
|
HF (ms2/Hz) |
43 (28 to 96) |
77 (49 to 99) P = 0.041 |
67 (45 to 92) P = 0.096 |
63 (35 to 103) P = 0.177 |
|
LF (ms2/Hz) |
74 (45 to 165) |
80 (49 to 139) P = 0.245 |
122 (74 to 211) P = 0.009 |
132 (78 to 207) P = 0.074 |
|
TP (ms2/Hz) |
215 (113 to 386) |
196 (134 to 316) P = 0.826 |
300 (169 to 369) P = 0.048 |
365 (193 to 543) P = 0.030 |
|
HFnu |
0.40 (0.24 to 0.58) |
0.43 (0.34 to 0.67) P = 0.245 |
0.33 (0.20 to 0.49) P = 0.048 |
0.31 (0.16 to 0.61) P = 0.096 |
|
MeanNN (ms) |
714 (684 to 851) |
745 (700 to 933) P = 0.011 |
726 (681 to 890) P = 0.074 |
734 (676 to 920) P = 0.056 |
|
SDNN (ms) |
23 (19 to 36) |
25 (21 to 32) P = 0.109 |
29 (24 to 36) P = 0.022 |
28 (22 to 37) P = 0.026 |
|
RMSSD (ms) |
23 (14 to 27) |
27 (19 to 32) P = 0.074 |
26 (19 to 32) P = 0.124 |
21 (18 to 32) P = 0.140 |
|
pNN50 (%) |
2 (0 to 4) |
5 (1 to 10) P = 0.046 |
2 (1 to 10) P = 0.084 |
2 (1 to 11) P = 0.055 |
|
Heart Rate (bpm) |
82 (70 to 90) |
NA |
NA |
79 (71 to 88) P = 0.875 |
|
SBP (mmHg) |
107 (100 to 117) |
NA |
NA |
105 (97 to 111) P = 0.099 |
|
DBP (mmHg) |
72 (68 to 77) |
NA |
NA |
70 (67 to 78) P = 0.262 |
|
Body Tension (Score value)
|
3.0 (2.0 to 4.3) |
NA |
NA |
2.0 (1.0 to 3.3) P = 0.007 |
|
Head massage therapy (HMT)
|
||||
|
Parameters |
Baseline
|
During intervention p-value
|
5 minutes post intervention p-value P-value
|
15 minutes post intervention p-value P value
|
|
HF (ms2/Hz) |
54 (19 to 105) |
108 (42 to 130) P = 0.005 |
66 (25 to 115) P = 0.124 |
110 (18 to 196) P = 0.030 |
|
LF (ms2/Hz) |
84 (59 to 134) |
110 (57 to 148) P = 0.925 |
135 (91 to 182) P = 0.363 |
117 (68 to 369) P = 0.074 |
|
TP (ms2/Hz) |
216 (151 to 337) |
336 (197 to 414) P = 0.022 |
329 (175 to 487) P = 0.026 |
335 (146 to 650) P = 0.158 |
|
HFnu |
0.26 (0.19 to 0.40) |
0.43 (0.35 to 0.51) P = 0.011 |
0.31 (0.22 to 0.45) P = 0.875 |
0.36 (0.23 to 0.46) P = 0.875 |
|
MeanNN (ms) |
717 (665 to 835) |
787 (727 to 881) P = 0.001
|
769 (707 to 871) P = 0.002 |
750 (678 to 898) P = 0.124 |
|
SDNN (ms) |
23 (20 to 34) |
32 (23 to 35) P = 0.056 |
29 (23 to 37) P = 0.056 |
32 (20 to 46) P = 0.124 |
|
RMSSD (ms) |
21 (15 to 35) |
33 (21 to 37) P = 0.002 |
28 (17 to 37) P = 0.009 |
31 (16 to 43) P = 0.041 |
|
pNN50 (%) |
2 (0 to 13) |
9 (0 to 16) P = 0.013 |
6 (0 to 15) P = 0.101 |
6 (0 to 20) P = 0.064 |
|
Heart Rate (bpm) |
83 (67 to 92) |
NA |
NA |
74 (66 to 84) P = 0.013 |
|
SBP (mmHg) |
103 (100 to 117) |
NA |
NA |
105 (97 to 114) P = 0.271 |
|
DBP (mmHg) |
72 (68 to 77) |
NA |
NA |
70 (66 to 74) P = 0.063 |
|
Body Tension (Score value)
|
3.0 (2.0 to 3.3) |
NA |
NA |
1.0 (1.0 to 2.3) P = 0.003 |
|
Relaxed reading (RR)
|
||||
|
Parameters |
Baseline
|
During intervention p-value
|
5 minutes post intervention p-value P value
|
15 minutes post intervention p-value P value
|
|
HF (ms2/Hz) |
56 (31 to 79) |
69 (32 to 143) P = 0.035 |
65 (34 to 136) P = 0.109 |
74(24 to 115) P = 0.272 |
|
LF (ms2/Hz) |
77 (45 to 143) |
164 (78 to 274) P = 0.001 |
123 (62 to 234) P = 0.022 |
169 (67 to 326) P = 0.005 |
|
TP (ms2/Hz) |
193 (150 to 330) |
336 (185 to 603) P = 0.001 |
329 (158to 553) P = 0.008 |
380 (203 to 906) P = 0.006 |
|
HFnu |
0.38 (0.24 to 0.47) |
0.33 (0.19 to 0.42) P = 0.041 |
0.33 (0.19 to 0.55) P = 0.433 |
0.29 (0.14 to 0.44) P = 0.011 |
|
MeanNN (ms) |
786 (692 to 839) |
762 (703 to 831) P = 0.638 |
796 (699 to 861) P = 0.778 |
777 (700 to 875) P = 0.594 |
|
SDNN (ms) |
23 (20 to 29) |
31 (23 to 41) P = 0.002 |
31 (22 to 39) P = 0.013 |
29 (24 to 39) P = 0.048 |
|
RMSSD (ms) |
22 (18 to 27) |
27 (18 to 34) P = 0.035 |
23 (20 to 32) P = 0.096 |
25 (18 to 33) P = 0.064 |
|
pNN50 (%) |
2 (0 to 6) |
6 (1 to 11) P = 0.022 |
5 (1 to 13) P = 0.064 |
5 (1 to 15) P = 0.030 |
|
Heart Rate (bpm) |
76 (69 to 84) |
NA |
NA |
78 (73 to 83) P = 0.635 |
|
SBP (mmHg) |
108 (96 to 113) |
NA |
NA |
111 (99 to 106) P = 0.508 |
|
DBP (mmHg) |
73 (70 to 75) |
NA |
NA |
74 (65 to 79) P = 0.599 |
|
Body Tension (Score value)
|
3.0 (2.0 to 4.0) |
NA |
NA |
2.5 (1.0 to 3.3) P = 0.006 |
Table 1: values of the HRV parameters and clinical outcomes at different times (n = 14 participants).
P values represent the statistical significance of the changes from baseline during the three interventions.
Values are median (IQR). P values are reported using Wilcoxon signed-rank test.
Abbreviation: DBP, diastolic blood pressure; HF, high frequency; HFnu, high frequency normalized unit; HMT, head massage therapy; HR, heart rate; IQR, interquartile range; LF, low frequency; MHM, mechanical helmet massager; NA: not available; pNN50, percentage of R-R intervals that differ by >50 ms from adjacent interval, over by the total number of all R–R intervals; RMSSD, root-mean-square of successive differences; RR, relaxed reading; SBP, systolic blood pressure; SDNN, standard deviation of mean NN intervals; TP, total power.
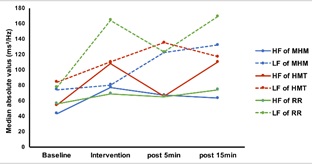 Figure 3: Changes of HF and LF median values (in ms2/Hz) during three different interventions.
Figure 3: Changes of HF and LF median values (in ms2/Hz) during three different interventions.
HF values increased during each intervention especially during HMT. Overall, LF values increased more than HF values, especially during relaxed reading.
Abbreviation: HF, High Frequency; LF, Low Frequency.
Comparisons of interventions, adjusted for baseline values, are presented in table 2 which shows the %change of the different parameters during the intervention, as well as 5 and 15 minutes after the intervention. When exposed to HMT, participants showed a positive %change of median HFnu by +35% (IQR: +3 to +93) during the intervention that lasted 15 minutes after intervention (+9%, IQR: -35 to +61); while during RR, the percentage change in HFnu decreased by -24% (IQR: -44 to +2); this difference was statistically significant (p = 0.011) and remained significant 15 minutes after the intervention (p = 0.048). Finally, exposure to MHM showed a slight increase of HFnu by only +5% (IQR: -10 to +50) during the intervention, followed by a decrease that reached -17% (IQR: -38 to +5) at 15 minutes.
|
Parameters |
Baseline & Percentage Change (median, IQR) % |
Between groups comparisons p-values |
||||
|
Comparison to baseline |
MHM |
HMT
|
RR |
MHM vs HMT |
MHM vs RR |
HMT vs RR |
|
LF baseline (ms2/Hz) |
74 (45 to 165) |
84 (59 to 134) |
77 (45 to 143) |
0.551 |
0.875 |
0.638 |
|
% change LF (intervention) |
+9% (-7 to 77) |
-3% (-17 to 81) |
+67% (+40 to 175) |
0.510 |
0.064 |
0.026 |
|
% change LF (5’ post Intervention) |
+81% (+22 to +144) |
+21% (-15 to +119) |
+65% (-3 to +108) |
0.221 |
0.300 |
0.363 |
|
% change LF (15’ post Intervention) |
+59% (-4 to +137) |
+18% (-19 to +184) |
+73% (+38 to +297) |
0.638 |
0.433 |
0.397 |
|
HF baseline (ms2/Hz) |
43 (28 to 96) |
54 (19 to 105) |
56 (31 to 79) |
0.975 |
0.730 |
0.638 |
|
% change HF (intervention) |
+42% (+14 to +124) |
+65% (-32 to +100) |
+28% (-4 to +114) |
0.975 |
0.778 |
0.470 |
|
% change HF (5’ post Intervention) |
+24% (-15 to +82) |
+39% (-6 to +103) |
+32% (-9 to +105) |
0.875 |
0.778 |
0.551 |
|
% change HF (15’ post Intervention) |
+31% (-16 to +71) |
+29% (-22 to +132) |
+35% (-29 to +128) |
0.778 |
0.638 |
0.875 |
|
HFnu baseline
|
0.40 (0.24 to 0.58) |
0.26 (0.19 to 0.40) |
0.38 (0.24 to 0.47) |
0.684 |
0.975 |
0.272 |
|
% change HFnu (intervention) |
+5% (-10 to +50) |
+35% (+3 to +93) |
-24% (-44 to +2) |
0.096 |
0.064 |
0.011 |
|
% change HFnu (5’ post Intervention) |
-21% (-32 to +10) |
+10% (-33 to +46) |
-12% (-27 to +102) |
0.124 |
0.551 |
0.594 |
|
% change HFnu (15’ post Intervention) |
-17% (-38 to +5) |
+9% (-35 to +61) |
-25% (-40 to -2) |
0.064 |
0.470 |
0.048 |
|
HF + LF baseline |
120 (71 to 267) |
147 (97 to 241) |
141 (87 to 208) |
0.826 |
0.683 |
0.397 |
|
% change (intervention) |
+30% (+8 to +62) |
+25% (-3 to +56) |
+51% (+26 to +126) |
0.510 |
0.245 |
0.177 |
|
% change (5’ post Intervention) |
+65% (+33 to +78) |
+24% (+3 to +67) |
+55% (+13 to +82) |
0.109 |
0.551 |
0.272 |
|
% change (15’ post Intervention) |
+56% (-5 to +121) |
+18% (-9 to +147) |
+74% (-4 to +185) |
0.875 |
0.470 |
0.594 |
|
TP baseline (ms2/Hz) |
215 (113 to 386) |
216 (151 to 337) |
193 (150 to 330) |
0.975 |
0.638 |
0.975 |
|
% change TP (intervention) |
+13% (-24 to +67) |
+26% (+3 to +54) |
+54% (+24 to +159) |
0.551 |
0.048 |
0.124 |
|
% change TP (5’ post Intervention) |
+28% (-3 to +92) |
+33% (+9 to +77) |
+39% (+1 to +111) |
0.730 |
0.875 |
0.397 |
|
% change TP (15’ post Intervention) |
+54% (-5 to +131) |
+12% (-12 to +121) |
+106% (+10 to +212) |
0.470 |
0.594 |
0.245 |
|
Heart Rate baseline (bpm) |
82 (70 to 90) |
83 (67 to 92) |
76 (69 to 84) |
0.730 |
0.450 |
0.272 |
|
% change HR (15’ post Intervention) |
-1.3% (-3.7 to +5.7) |
-5.9% (-14 to +1.5) |
0.3% (-3.9 to +5.2) |
0.074 |
0.300 |
0.035 |
|
SBP baseline (mmHg) |
107 (100 to 117) |
103 (100 to 117) |
108 (96 to 113) |
0.379 |
0.068 |
0.421 |
|
% change SBP (15’ post Intervention) |
-1.0% (-8.2 to +1.3) |
-1.7% (-6.2 to +2.3) |
+0.9% (-2.3 to +5.2) |
0.683 |
0.056 |
0.300 |
|
DBP baseline (mmHg) |
72 (68 to 77) |
72 (68 to 77) |
73 (70 to 75) |
0.649 |
0.529 |
0.969 |
|
% change DBP (15’ post Intervention) |
-1.4% (-7.0 to +3.1) |
-3.7% (-8.4 to +1.7) |
+0.7% (-6.7 to +9.0) |
0.683 |
0.397 |
0.084 |
|
Body tension baseline (Score value) |
3.0 (2.0 to 4.3) |
3.0 (2.0 to 3.3) |
3.0 (2.0 to 4.0) |
0.158 |
1.000 |
0.377 |
|
% change BT (15’ post Intervention) |
-33% (-50 to 0.0) |
-50% (-67 to -19) |
-29% (-50 to 0.0) |
0.021 |
0.844 |
0.252 |
Table 2: HRV parameters and clinical parameters at baseline and the relative changes from baseline to post-intervention in the three types of interventions (n = 14)
Values are median (IQR). P values are reported using Wilcoxon signed-rank test.
Abbreviation: BT, body tension; DBP, diastolic blood pressure; HF, high frequency; HFnu, high frequency normalized unit; HMT, head massage therapy; HR, heart rate; IQR, interquartile range; LF, low frequency; MHM, mechanical helmet massager; RR, relaxed reading; SBP, systolic blood pressure; TP, total power.
Table 2 also shows a median %change decrease of HR by -5.9% (IQR: -14 to +1.5) during HMT, in contrast to a slight increase of +0.3% (IQR: -3.9 to +5.2) during RR (p = 0.035) and a small decrease of -1.3% (IQR: -3.7 to +5.7) during MHM (p = 0.074). There is no important difference regarding the effects on systolic blood pressure but the %change in diastolic blood pressure (DBP) showed a decrease by -3.7% (IQR: -8.4 to +1.7) during HMT compared to a slight increase by +0.7% (IQR: -6.7 to +9.0) during RR and a mild decrease of -1.4% (IQR: -7.0 to +3.1) during MHM. Finally, we observed a higher effect of HMT on decreasing BT %change by -50% (IQR: -67 to -19), compared to both RR (-29%,) and MHM (-33%).
Correlation between %changes in HFnu during the HMT and %changes in clinical parameters 15 minutes later (Figure 4) shows that larger increase in HFnu is associated with higher decrease of both BT (p = -0.425; p = 0.130) and DBP (p = -0.323, p = 0.260). There is no correlation between HFnu and HR %changes.
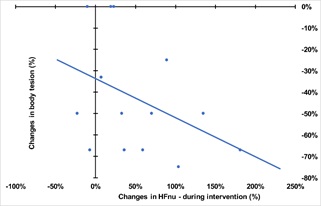
Figure 4: Correlation between changestable 1 in HFnu and changes in body tension score.
Individuals with higher %increase in HFnu tend to have a higher %decrease in BT.
Abbreviation: BT, body tension; HFnu, High Frequency normalized unit.
The analysis of HFnu %change at the individual level (Figure 5) shows that during HMT intervention most individuals (11/14) demonstrated a positive increase in HFnu, compared to only 8 during MHM and 3 during RR.
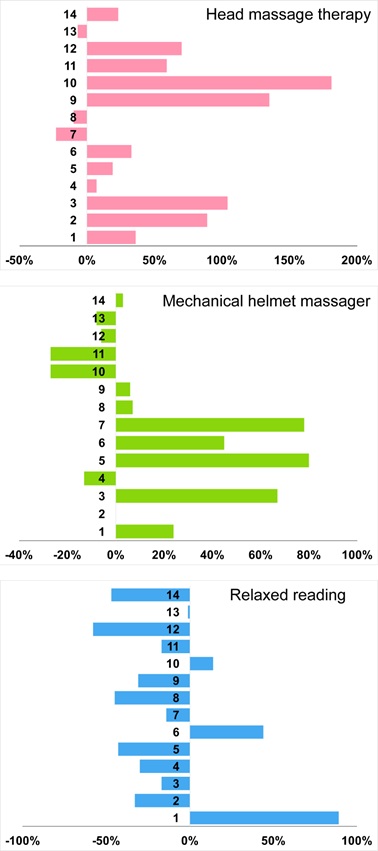 Figure 5: Individual percentage changes in HFnu of three different interventions.
Figure 5: Individual percentage changes in HFnu of three different interventions.
The majority of subjects responded positively to head massage therapy and mechanic helmet massager in comparison to relaxed reading.
Abbreviations: HFnu, High Frequency normalized unit.
Discussion
This is the first randomized crossover trial comparing the effects of HMT and MHM on the cardiac vagal control assessed by HRV. Because the three interventions have relaxing effects, the increased variability of heart rate, as illustrated by increased TP and SDNN during and after the interventions was expected, and is supported by scientific knowledge [8,11,25,26]. Among the three interventions HMT increased the most the HF values during interventions. Overall then, the PNS relative power (%changes of HFnu) increased most during HMT while it decreased after the two other interventions, especially RR.
The relationship between increased HFnu and changes in HR, DBP or BT is not surprising if we consider that the %increase in HFnu during HMT represents a relative increase of vagal tone over SNS. The relationship between increased PNS and decreased HR and BP has already been demonstrated in different contexts [17,25,27,28]. Several studies have shown in a convincing way the positive effects of massage to stimulate HF [8,17]. We may then explain the smaller effects of MHM and RR on clinical parameters by their smaller effect on PNS and HFnu.
In contrast to RR and MHM, the stronger correlation between %increase in HFnu during HMT and the %decrease in BT at 15 minutes post-intervention (Figure 4) is worth considering as a sign of HMT having a more deeply relaxing effect than the two other interventions. This result coupled with significant effects of HMT on decreasing HR (p = 0.013) and DBP (p = 0.063) illustrates its more important effects on stress reduction, at least until 15 minutes after the intervention. Our results also show that RR or MHM can induce relaxation with increased HRV, and associated decreased body tension (Tables 1 and 2), without having positive effects on HFnu and the clinical parameters. If confirmed, such a result could lead to guiding the different types of relaxation and massage practices to go beyond the participants’ feeling of relaxation, to reach a state of increased relative PNS, as expressed by increased HFnu. This contrast between different types of relaxing methods with different effects on HFnu requires more studies to better understand what triggers HFnu’s increase in different contexts, and how to interpret the changes.
The reason for HMT's higher efficiency over MHM to increase HFnu and improve a few clinical outcomes may find several possible explanations that are consistent with the neurovisceral integration model [13,14]. The head skin innervation is different from one region to the other with regard to vagus stimulation; it is possible that massage therapist already knows by experience the key places that need stimulation to reach deep relaxation. This therapist’s “hand touch” refers to the professional’s experience to adapt the intervention to the specific needs of the participant [29], which is impossible with a standard mechanical stimulation. Another possible reason may be the different emotional feelings and physiological reaction of the participants when receiving HMT or MHM, with higher level of comfort and trust, hence deeper relaxation when receiving professional care. This comparison warrants more studies to understand the mechanism of actions of the two types of head massaging approaches that may explain the differential effects observed.
Another important result is the inter-individual variability with regard to HRV’s response (Figure 5). Such results raise the question of a possible stressful effect of massage for some individuals, for instance when the participants do not feel comfortable to be touched or because the massage is painful. More studies are needed to better understand how participants perceive massage interventions and the possible effects of this emotional reception on physiological outcomes. Studying this opposite direction of effects among participants would also benefit from MRI imaging to understand the mechanism in the central autonomic network.
Duration of effects is generally short after HMT, which raises questions regarding a possible “therapeutic effect”. Repeated sessions or self-administration of massage may represent solutions [8,30]. Using MHM device is another possible solution as its effects, although less intense than HMT, seem real compared to RR. More generally, MHM elicited results that followed the same trend as HMT, but less intense and persistent. More studies are needed to better understand the effects of MHM, in particular in context of repeated sessions over days or weeks, that this device permits.
One strength of our study is the comparison of the participants with themselves in a randomized crossover design conducted at approximately the same time of the day to control the effect of the circadian rhythm on the ANS. Using %change of the different parameters is a way to control for baseline values, that vary among participants. We also used a state-of-the-art head massage therapist and the BREO helmet massager that was considered as one of the best in this category.
There are several limitations of the study. The sample size is small with a selected group of healthy volunteers, which is compatible with a descriptive exploratory study, but prevents the generalization of findings to other groups. Another limitation is the absence of psychometric data regarding the BT scale, that has been used with success in another study [18]. Although not well known, the BT scale showed a good sensitivity to change in both our study and the Reibel’s study [18]. Finally, the MHM device offered music and a peaceful relaxing voice, which may represent a co-intervention that affects PNS and the different outcomes independently; we cannot exclude that another mechanical head massager may generate different results.
Conclusion
Overall, this study shows that the three interventions have a relaxing effect leading to an increase of HR variability. Only Chinese HMT however, could trigger a %change in HFnu that was larger than the ones after MHM or RR, which may explain the observed effects on several clinical parameters after HMT. MHM triggered the HRV %changes in the same direction as HMT, but of a smaller magnitude. More studies are needed to explain the differences of effects between HMT and MHM and also to understand which factors affect the direction of the changes among individuals, in light of the neurovisceral integration and the multiple parameters involved. Finally, this study shows the possible use of HRV parameters to guide the development of more efficient relaxing interventions.
Acknowledgement
We gratefully acknowledge the dedicated work of Dr. Donghua Wang, TCM doctor at Tiantan hospital, for conducting the head massage interventions, Ms Ji Qi to organize the study time management for the intervention and collecting baseline information, and Ms Zheng Song who conducted HRV recording for all the participants.
Author Contribution Statement
Chen Zhang: acquisition of data, analysis and interpretation of data, drafting of the manuscript. Ling Guan: Interpretation of data. Donghua Wang and Shangrong Han: acquisition of data. Yilong Wang and Yongjun Wang: Study supervision. Jean-Paul Collet: Study concept and design, critical revision of the manuscript.
Author Disclosure Statement
No competing financial interests exist.
Funding Statements
The study received grants from the Advanced Innovation Center For Human Brain Protection, Capital Medical University, Beijing, China (3500-11920125); The National Natural Science Foundation of China (81801187). National Natural Science Foundation of China (81825007); Ministry of Science and Technology of the People’s Republic of China (2017YFC1307900); Scientific technology innovation service construction (3500-119209); Beijing Municipal Science and Technology Commission (D171100003017001 and 2016000021223TD0.
References
- Fattah MA, Hamdy B (2011) Pulmonary functions of children with asthma improve following massage therapy. J Altern Complement Med 17: 1065-1068.
- Karagozoglu S, Kahve E (2013) Effects of back massage on chemotherapy-related fatigue and anxiety: supportive care and therapeutic touch in cancer nursing. Appl Nurs Res 26: 210-217.
- Billhult A, Bergbom I, Victorin ES (2007) Massage relieves nausea in women with breast cancer who are undergoing chemotherapy. J Altern Complement Med 13: 53-57.
- Adams R, White B, Beckett C (2010) The effects of massage therapy on pain management in the acute care setting. Int J Ther Massage Bodywork 3: 4-11.
- Sturgeon M, Hall RW, Hart T, Good M, Dakhil S (2009) Effects of therapeutic massage on the quality of life among patients with breast cancer during treatment. J Altern Complement Med 15: 373-380.
- Donoyama N, Ohkoshi N (2012) Effects of traditional Japanese massage therapy on various symptoms in patients with Parkinson's disease: a case-series study. J Altern Complement Med 18: 294-299.
- Westman KF, Blaisdell C (2016) Many Benefits, Little Risk: The Use of Massage in Nursing Practice. Am J Nurs 116: 34-39.
- Guan L, Collet JP, Yuskiv N, Skippen P, Bran R, et al. (2014) The effect of massage therapy on autonomic activity in critically ill children. Evidence-based complementary and alternative medicine 2014: 656750.
- Suzuki M, Tatsumi A, Otsuka T, Kikuchi K, Mizuta A, et al. (2010) Physical and psychological effects of 6-week tactile massage on elderly patients with severe dementia. American journal of Alzheimer's disease and other dementias 25: 680-686.
- Hellstrom A, Willman A (2011) Promoting sleep by nursing interventions in health care settings: a systematic review. Worldviews Evid Based Nurs 8: 128-142.
- Aourell M, Skoog M, Carleson J (2005) Effects of Swedish massage on blood pressure. Complement Ther Clin Pract 11: 242-246.
- Xiong XJ, Li SJ, Zhang YQ (2015) Massage therapy for essential hypertension: a systematic review. J Hum Hypertens 29: 143-151.
- Thayer JF, Hansen AL, Rose ES, Johnsen BH (2009) Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaptation, and health. Ann Behav Med 37: 141-153.
- Smith R, Thayer JF, Khalsa SS, Lane RD (2017) The hierarchical basis of neurovisceral integration. Neurosci Biobehav Rev 75: 274-296.
- Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, et al. (1981) Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science 213: 220-222.
- Eur Heart J (1996) Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J 17: 354-381.
- Fazeli MS, Pourrahmat MM, Liu M, Guan L, Collet JP (2016) The Effect of Head Massage on the Regulation of the Cardiac Autonomic Nervous System: A Pilot Randomized Crossover Trial. J Altern Complement Med 22: 75-80.
- Reibel DK, Greeson JM, Brainard GC, Rosenzweig S (2001) Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. General hospital psychiatry 23: 183-192.
- Laborde S, Mosley E, Thayer JF (2017) Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological Research - Recommendations for Experiment Planning, Data Analysis, and Data Reporting. Front Psychol 8: 213.
- Malliani A, Pagani M, Lombardi F, Cerutti S (1991) Cardiovascular neural regulation explored in the frequency domain. Circulation 84: 482-492.
- Pumprla J, Howorka K, Groves D, Chester M, Nolan J (2002) Functional assessment of heart rate variability: physiological basis and practical applications. International journal of cardiology 84: 1-14.
- Rahman F, Pechnik S, Gross D, Sewell LT, Goldstein DS (2011) Low frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation. Clin Auton Res 21: 133-141.
- Goldstein DS, Bentho O, Park MY, Sharabi Y (2011) Low-frequency power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflexes. Experimental physiology 96: 1255-1261.
- Armitage P, Berry G, Matthews JNS (1994) Statistical methods in medical research. Blackwell Scientific Publications, Oxford, UK.
- Moraska A, Pollini RA, Boulanger K, Brooks MZ, Teitlebaum L (2010) Physiological adjustments to stress measures following massage therapy: a review of the literature. Evidence-based complementary and alternative medicine 7: 409-418.
- Diego MA, Field T, Sanders C, Reif MH (2004) Massage therapy of moderate and light pressure and vibrator effects on EEG and heart rate. The International journal of neuroscience 114: 31-44.
- Buttagat V, Eungpinichpong W, Chatchawan U, Kharmwan S (2011) The immediate effects of traditional Thai massage on heart rate variability and stress-related parameters in patients with back pain associated with myofascial trigger points. J Bodyw Mov Ther 15: 15-23.
- Moyer CA, Rounds J, Hannum JW (2004) A meta-analysis of massage therapy research. Psychol Bull 130: 3-18.
- Cancelli A, Cottone C, Giordani A, Asta G, Lupoi D (2018) MRI-Guided Regional Personalized Electrical Stimulation in Multisession and Home Treatments. Front Neurosci 12: 284.
- Fan YL, Fan YL, Flaws B (1997) Chinese Self-Massage Therapy. SATAS, Belgium.
Citation: Zhang C, Guan L, Wang D, Han S, Wang Y, et al. (2021) Head Massage Therapy More Efficacious Than Mechanical Helmet Massager to Stimulate Parasympathetic Cardiac Tone: A Randomized Cross-Over Trial. J Altern Complement Integr Med 7: 205.
Copyright: © 2021 Chen Zhang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

