
Health Literacy: The Most Neglected Essential Human Quality
*Corresponding Author(s):
Abdul Kader MohiuddinAlumnus, Faculty Of Pharmacy, Dhaka University, Bangladesh
Tel:+880 1706221174,
Email:trymohi@gmail.com
Abstract
People must have particular personality traits and social resources, also known as health literacy, in order to access, comprehend, and use information to make decisions about their health. Patients' ability to engage in complex disease management and self-care is strongly related to their level of health literacy. It can help us stay healthy by preventing illness and effectively managing existing illnesses. People with Low Health Literacy (LHL) may find it difficult to manage their condition and prevent illness, which may lead to increased use of healthcare services. Furthermore, LHL is associated with increased hospitalizations, increased use of emergency care, decreased use of preventative services, and a worsened ability to understand labels and health messages, a worsened state of health, higher mortality, and more expensive medical care.
Keywords
Avoidable Medical Costs; COVID-19 Vaccine Negligence; Global Health Burden; Healthcare; Medication Non-Adherence; Necessary Health Education; Parental Health Literacy; Understanding Treatment Guidelines
Abbreviations
ADHD: Attention Deficit Hyperactivity Disorder
ASD: Autism Spectrum Disorder
AUD: Alcohol Use Disorder
CDC: US Centers for Disease Control and Prevention
COVID-19: Coronavirus Disease 2019
ED: Emergency Department
MC: Medical Cannabis
SMBG: Self-Monitoring of Blood Glucose
SUD: Substance Use Disorder
UNODC: UN Office on Drugs and Crime
Introduction
Understanding common health care communications, such as prescription instructions, test results, and insurance forms, is referred to as health literacy. Health literacy improves a population's ability to care for them and aids in the reduction of health disparities. It has an impact on the use of health services, as well as on patient satisfaction and the physician-patient relationship. It is one of the major impediments to healthcare professionals adequately transmitting information to those under their care. Personal health literacy refers to a person's ability to locate, comprehend, and apply information and services to support health-related decisions and actions for themselves and others. Health literacy is recommended by the World Health Organization as a tool for achieving several important objectives outlined in the Sustainable Development Goals. Many factors can influence a person's health literacy, including knowledge of medical terminology; understanding of how the health care system operates; ability to communicate with health care providers; ability to locate health information, which may be associated with age, income, education, language skills, and culture; and physical or psychological limitations. Health literacy affects treatment adherence, which may have an impact on treatment outcomes. Despite the negative implications of LHL, physicians are typically unaware of their patients’ health literacy levels and their subsequent effects on their patients’ outcomes (Figure 1).
 Figure 1: Graphical Abstract Health Literacy.
Figure 1: Graphical Abstract Health Literacy.
Material And Methods
Prioritized databases for public health topics included PubMed, ALTAVISTA, Embase, Scopus, Web of Science, and the Cochrane Central Registers. Along with other online sources, journals from Elsevier, Springer, Willey Online Library, and Wolters Kluwer were thoroughly searched. The infographic was prepared by Canva Illustrator, and the citation work was done by citationmachine.net.
Literature Review
Many studies reveal that patients from high-income countries are not adequately adhering to medications as they are prescribed. Forgetfulness, confusion about the duration required for medication use, and mistrust about the overall efficacy of medication are among the reasons for non-adherence to diabetes management protocols in Middle Eastern countries [1]. Conversely, after World War II, Taiwan faced severe poverty, but it is now the 8th largest economy in Asia and also the home of type 2 diabetes patients with more than 80% health literacy [2]. LHL is a prevailing problem in Europe, Asia and Africa. Bulgaria, Lithuania and Latvia are the 3 European countries with lowest health literacy [3]. Around the globe, LHL prevails mostly with people living in rural areas and having a low education level. Surprisingly, LHL prevails among half of the population in both developing and developed countries [4].
Prevalence, Reasons and Global Burden with LHL
Health literacy is the result of both an individual's abilities and the demands and complexities of the healthcare system. Health literacy is heavily influenced by a country's medical practices, as well as individual and social factors present in interactions between people and the systemic demands of the healthcare system. LHL is most frequently linked to older people with chronic illnesses who have little education and are not necessarily from lower socioeconomic backgrounds. Also, socioeconomically disadvantaged people, those who belong to ethnic minorities, or people with higher psychological distress, physical limitations, poor social support, compromised mental health and quality of life are contributors of LHL. Furthermore, being literate in general does not imply being literate in health [5,6]. However, in this submission, a few more sensational facts in the form of an infographic model about LHL is shared (Figure 2):
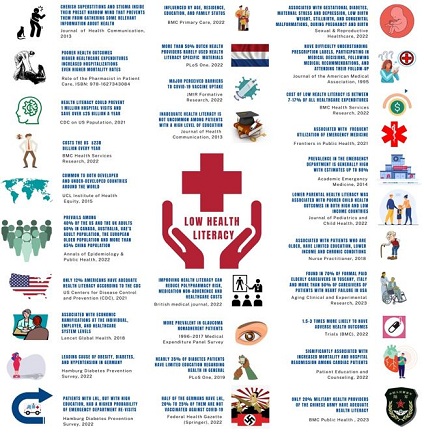 Figure 2: Low Health Literacy Facts.
Figure 2: Low Health Literacy Facts.
- LHL is associated with people who cherish superstitions and stigma within their preset narrow mind, which prevents them from gathering relevant health information from their surroundings [5].
- LHL has a significant impact on patients' treatment guideline compliance, or, more directly, medication adherence, which leads to poorer health outcomes, higher healthcare costs, increased hospitalizations, and even higher mortality rates [6].
- Only 12% of Americans have adequate health literacy, and improving health literacy could prevent nearly 1 million hospital visits and save more than $25 billion per year, according to the US Centers for Disease Control and Prevention (CDC) [7].
- The global economic cost of illiteracy is estimated to be $19 trillion, but LHL alone costs the US economy $238 billion per year [8].
- Both are found in both developed and developing countries around the world, and socioeconomic factors are not the only cause of LHL [9].
- Surprisingly, nearly 40% of US and UK adults have LHL, compared to around 50% of Europeans, 60% of adults in Canada, Australia, and the UAE, and nearly 70% of Chinese [10].
- In China, health literacy increased from 6.48% of the population in 2008 to 23.15% in 2020 [11]. However, only 1 in 5 military health providers of the Chinese People's liberation Army had adequate health literacy, found in a recent survey published in BMC Public Health [12].
- Evidence suggests that LHL has significant economic consequences at the individual, employer, and healthcare system levels [13].
- The authors of the Hamburg Diabetes Prevention Survey, a population-based cross-sectional study in Germany, concluded that LHL is a significant risk factor for the metabolic syndrome's three conditions: obesity, diabetes, and hypertension [14].
- Age, place of residence, education, and family status all have an impact on health literacy [15].
- More than half of Dutch health providers use health literacy-specific materials only infrequently [16].
- Mistrust and LHL perceptions were linked to high levels of vaccine hesitancy, providing evidential support for portraying these factors as perceived barriers to COVID-19 vaccine uptake [17].
- LHL is not uncommon among patients with a high level of education or with well-off patients. Moreover, patients with LHL, but with high education, had a higher probability of Emergency Department (ED) re-visits. Empirical research based on a conceptual model estimated that LHL costs between 7 and 17% of total healthcare expenditures [8].
- According to patient-centered interventions, improving health literacy can reduce the risk of polypharmacy, medication non-adherence, and healthcare costs [18].
- According to the 1996-2017 Medical Expenditure Panel Survey (Cheng & Tanna, 2022), LHL was more prevalent in glaucoma patients, and patients with LHL were prescribed more medications and had higher medication costs [19].
- Nearly 35% of diabetic patients worldwide have limited health-related education [20].
- LHL is linked to gestational diabetes, maternal stress and depression, low birth weight, stillbirth, and congenital malformations during pregnancy and birth, all of which have negative consequences for the woman and her child [21].
- Health literacy among the population is expected to rise over time in this era of modernization. According to a national survey conducted in the Czech Republic in 2015-16, nearly 60% of Czechs have LHL. Surprisingly, a 2018 survey revealed that health literacy in the Czech Republic was still declining [22].
- The prevalence of LHL in the ED varies greatly, with estimates as high as 88% depending on the patient mix and screening instruments used [23].
- In both low and high-income countries, low parental health literacy was linked to poorer child health outcomes [24].
- Patients who are older, have less education, a lower income, and have chronic conditions are more vulnerable [25].
- LHL was discovered in more than 70% of formal paid caregivers of non-self-supporting older adults in Tuscany, Italy, and in more than 50% of caregivers of heart failure patients in the United States [26].
- People with LHL may have 1.5-3 times the number of serious health outcomes, such as higher mortality, hospitalization rates, and disease management ability, as those with adequate health literacy [27].
- In cardiac patients, it has been linked to increased mortality, hospital readmission, and lower quality of life [28].
- LHL represents nearly 50% of Germans [29]. In Germany, every fourth to fifth person is not immunized against COVID-19 [30].
- According to a Waystar (Health Care Billing Software) report from 2019, nearly 40% of healthcare consumers were unaware that the cost of their healthcare varied across facilities [31].
Factors or Consequences Associated with LHL
Superstitions: An Elephant in The Room
Superstition is the non-scientific belief in magical connection. Aspects of certain religions and supernatural ideologies, such as astrology, omens, witchcraft, and prophecies, are examples of such beliefs. Even after all of the modernization and enlightenment, superstitious beliefs still exist in our societies. Most people are thought to have irrational, superstitious beliefs to some extent. Epilepsy and schizophrenia are still viewed in the majority of the world as an evil spirit. Although two-thirds of patients could become seizure-free with proper care, poor adherence to proper guidelines is a major problem for effective recovery [32,33]. In an Indian study, 60% of the participants thought that illnesses were the result of luck or superstition [34]. In Northern Germany, superstitions were also reported in nearly 40% of men and 70% of women [35]. 70% of people in Africa use folk remedies like charms and witchcraft to treat their illnesses [36]. Surprisingly, researchers found that 73% of addiction treatment programs in the USA include a spirituality-based element and that more than 40% of Americans believe in spiritual therapies [37,38]. According to a South Iranian study, 60% of diabetic patients refused insulin despite doctor recommendations due to phobia [39]. Menstruation is fraught with taboos, restrictions, and misconceptions in low- and middle-income countries, especially in India and sub-Saharan Africa [40]. In India, nearly 80% of menstruating girls and women use an old cloth that is frequently reused. Further, around 90% of women in India sometimes resort to using ashes, rags, sand, newspapers, dried leaves, wood shavings, hay, plastic and husk sand to aid absorption [41-43]. Additionally, these two areas are home to more than 90% of the world's open defecation practitioners [44,45]. Many superstitious Indians hold the view that defecation is an impure act that should only be performed outside the home and that toilets should only be used in inclement weather [46]. It is not surprising that at least 90% of Indian adults have poor health literacy [47].
Medication or Treatment Guideline Non-compliance
Medication noncompliance accounts for more than half of the $500 billion in total avoidable costs associated with suboptimal medicine use worldwide each year [48]. LHL was linked to increased unintentional non-adherence and poor medication self-management in a variety of domains, including forgetting or having difficulty remembering to take medications. However, no relationship was found between health literacy and intentional non-adherence, which includes stopping medications when feeling better or worse [49]. Studies show that LHL is connected with poorer disease knowledge and symptom recognition, poor glycemic or dyslipidemia control, greater difficulty interpreting food labels and estimating portion sizes, lower self-efficacy, higher level of body mass index, information gap in the use of medical devices for Self-Monitoring of Blood Glucose (SMBG), poorer communication with their providers, higher doses of insulin, more medical expenses and hospitalization among diabetes patients [50-57]. LHL is more common in people with hypertension and is associated with hypertension prevalence in selected ethnic groups [58]. Among hypertensive patients, LHL was associated with higher dietary salt intake, poor knowledge of blood pressure control, lower systolic blood pressure control, current smoking or higher nicotine dependence, as well as established predictors of smoking relapse [59-62]. Apart from these, LHL was associated with higher addiction severity [63], medication errors, misinterpreting physician’s instructions and disease symptoms [64], a greater number of unreconciled medications [65], reason behind the medication discrepancy [66], preventable adverse drug reactions [67], inequity of access to the benefits of prescription medication [68].
Substance Use Disorder
Drug addiction kills approximately 8 million people each year, and the UN Office on Drugs and Crime (UNODC)’s World Drug Report 2022 estimates that approximately 284 million people aged 15-64 used drugs worldwide in 2020 [69,70]. According to University of Pennsylvania research, America has spent over a trillion dollars enforcing its drug policy since 1971 [71]. People who use alcohol (AUD) or have a Substance Use Disorder (SUD) are at risk of having lower health literacy due to a variety of negative health, psychosocial, and economic factors associated with substance use [72]. Another study confirms that both LHL and low academic performance have their role in tackling the disparities in substance use [73]. An Australian study with a mixed sample of people with AUD and SUD found that 90% of participants had LHL [74]. In people with alcohol and drug dependence, LHL is associated with worse depressive symptoms [63]. Patients with LHL poorly handle pain medications [75]. Around 300 metric tons of morphine-type painkillers are used (and/or abused) worldwide each year, more than 99% of which consumed by high income countries [76]. A study based on a mixed population of US citizens confirmed that LHL was strongly linked to opioid misuse among adult patients with chronic pain [77]. Use of cannabis for pain management has always been a controversial issue. Also, cannabis in the form of Medical Cannabis (MC) or recreational marijuana legalized or less restricted in Thailand, Canada, Uruguay, South Korea, Japan, India, Pakistan, Israel, Belgium, USA, UK, Germany, Italy, Singapore and Malaysia, probably among many others. However, Health literacy, social support, attitudes about MC, age, and duration of disease were significantly associated with demand for MC use among cancer patients in Thailand [78].
Poor COVID-19 or Contagious Disease Management and Vaccine Negligence
A cross-sectional study of 259 school leaders in Hong Kong carried out during the COVID-19 pandemic between April 2021 and February 2022 shows that more than 50% of participants had LHL, and their LHL was strongly associated with a negative attitude about vaccination, low information, and confusion about COVID-19-related information [79]. Although, an Oxford Academic study concluded that not health literacy directly but poor knowledge of selected diseases was associated with vaccine confidence index [80]. Thankfully, another study from Oxford University Press established health literacy as the “social vaccine” to combat against SARS-CoV-2 [81]. Even before Covid-19, WHO has listed vaccine hesitancy as one of the top ten global health threats in 2019 [82,83]. Also, a Swiss journal says that a percentage increase in vaccine hesitancy can lead to a decline in vaccination coverage by 30% [84]. Therefore, LHL was the major obstacle to create vaccine hesitancy in China, Africa [85], India [86], Europe [87] and USA [88,89]. As expected, in three different studies, close to 40% of Chinese participants (LHL persists among more than 70% of the population) [10,85], more than 60% of Bulgarians (the lowest health literacy among EU countries) [3,86] showed hesitancy, and above all, more than one-third of European adults are not fully vaccinated (LHL persists among half of the total population), says another Oxford University Press study [10,89]. Vaccinated people or people wearing masks, on the other hand, were careless about social distancing, believing that being vaccinated or wearing masks was sufficient and that other preventive measures, such as social distancing, were unnecessary. Even the CDC redeemed fully vaccinated people who wore a face mask or engaged in social distancing in most settings, whether outdoors or indoors, in updated public health guidance released on May 13, 2021. Also, conspiracy theories, rallies against masks/vaccines are vividly reported [90-97].
Barriers to Autism Recovery and Progression
The social burden of autism can exceed $6 trillion in the US alone by 2060, and the WHO estimated that worldwide, about one in 100 children has autism [98,99]. The failure to recognize the first signs of autism can significantly postpone the age of diagnosis, the provision of informed supervision to families, and the execution of adapted initiatives during the critical period of early development. Parent health literacy may further contribute to autism services use for young children [100]. A misunderstanding of early signs as manifestations of a developmental condition may lead to increased stigma and non-conventional explanations [101-103]. Parents with LHL whose child has recently been diagnosed with Autism Spectrum Disorder (ASD) report an information gap and a lack of resource adaptation during diagnosis [104]. Above all, health literacy is linked to help-seeking behaviors among parents of Children with Special Health Care Needs (CSHCN), autism, and Attention Deficit Hyperactivity Disorder (ADHD); or people with Schizophrenia and Bipolar disorders [105-107].
Results and Discussion
LHL contributes significantly to the healthcare system's incompetent socioeconomic culture. Health issues are not only overlooked but also neglected. It reflects how much health and wellbeing are overlooked in a community or country. Economic conditions should not be condemned because they persist in developed countries as well. LHL has grown to unbearable proportions all over the world. Reading, listening, analytical, and decision-making skills, as well as the ability to apply them to health situations, are all components of health literacy. Literacy can only be improved through health education, which necessitates multifaceted approaches. Many members of the health care team lack health literacy training, are unaware of ways to improve communication, and forget to use effective communication practices on a regular basis when providing care. Health care professionals require assistance and training to better understand health literacy and how to address it through clear communication strategies. Customized patient education, on the other hand, engages, motivates, and strengthens patients to participate in their own health care and treatment decisions, resulting in better outcomes, fewer diagnostic tests, and significantly greater patient satisfaction.
Conclusion
Nonetheless, health literacy is clearly beneficial in addressing the healthcare needs of even the most marginalized and disadvantaged communities. Patients must clearly and appropriately recognize healthcare information related to their specific illness or disease in order to improve adherence. This understanding could be crucial in assisting patients in developing the motivation, beliefs, and appropriate health behaviors needed to improve overall adherence. LHL is a curse to be avoided. This effort should be supported by all healthcare providers, stakeholders, and even government and community leaders.
Acknowledgement
Dr. Rayhan A. Tariq, Drexel University College of Medicine for taking the time to review my paper and for his insightful comments. For lending me books, journals, and newsletters, the seminar library of the University of Dhaka's Faculty of Pharmacy and Bangladesh's BANSDOC Library are also to be thanked.
Declarations
The current research was carried out exclusively to look into problems associated with low health literacy. With time and the availability of newer investigation in the same field, the statistical evidence or variables presented here may transform.
Funding
The author has not received any fund from any authority.
Author Contributions
The corresponding author is the sole contributor and the only author.
Conflicts of Interest
The author declares that he has no competing interests.
References
- Mohiuddin AK (2022) Medication adherence: Fact or fictions?. Current Research in Public Health 2: 18-21.
- Lovric B, Placento H, Farcic N, Baligic ML, Miksic S, et al. (2022) Association between Health Literacy and Prevalence of Obesity, Arterial Hypertension, and Diabetes Mellitus. Int J Environ Res Public Health 19: 9002.
- Gatulyte I, Verdina V, Varpina Z, Lublóy Á (2022) Level of health literacy in Latvia and Lithuania: A population-based study. Arch Public Health 80: 166.
- Buawangpong N, Sirikul W, Anukhro C, Seesen M, La-Up A, et al. (2022) Health Information Sources Influencing Health Literacy in Different Social Contexts across Age Groups in Northern Thailand Citizens. Int J Environ Res Public Health 19: 6051.
- Heide IVD, Wang J, Droomers M, Spreeuwenberg P, Rademakers J, et al. (2013) The relationship between health, education, and health literacy: Results from the Dutch Adult Literacy and Life Skills Survey. Journal of Health Communication 18: 172-184.
- Mohiuddin AK (2020) The Enigma of Patient Behavior. The Role of the Pharmacist in Patient Care: Achieving High Quality, Cost-Effective and Accessible Healthcare Through a Team Based, Patient-Centered Approach, Universal-Publishers 189-210.
- US CDC Health Literacy Basics (2021) Talking points about health literacy. Centers for Disease Control and Prevention.
- Shahid R, Shoker M, Chu LM, Frehlick R, Ward H, et al. (2022) Impact of low health literacy on patients' health outcomes: A multicenter cohort study. BMC Health Services Research 22: 1148.
- UCL Institute of Health Equity/Public Health England (2015) Local action on health inequalities-Improving health literacy to reduce health inequalities. UK Government Publishing Service: 1-16.
- Mohiuddin AK (2022) Low Health Literacy: Treacherous Foe of Patient Compliance in Developed Countries. A Epidemiol Public Health 5: 1097.
- Li Y, Lv X, Liang J, Dong H, Chen C (2022) The development and progress of health literacy in China. Front Public Health 10: 1034907.
- Rong H, Lu L, Wang L, Liu C, Zhang L, et al. (2023) Investigation of health literacy status and related influencing factors in military health providers of Chinese People's liberation Army, a cross-sectional study. BMC Public Health 23: 4.
- Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, et al. (2018) High-quality health systems in the Sustainable Development Goals Era: Time for a revolution. The Lancet Global Health 6: 1196-1252.
- Tajdar D, Schäfer I, Dagmar L, Fertmann R (2022) The Link Between Health Literacy and Three Conditions of Metabolic Syndrome: Obesity, Diabetes and Hypertension. Diabetes Metab Syndr Obes 15: 1639-1650.
- Šulinskaite K, Zagurskiene D, Blaževiciene A (2023) Patients' health literacy and health behaviour assessment in primary health care: evidence from a cross-sectional survey. BMC Prim Care 23: 223.
- Murugesu L, Heijmans M, Rademakers J, Fransen MP (2022) Challenges and solutions in communication with patients with low health literacy: Perspectives of healthcare providers. PLoS One 17: 0267782.
- Weerakoon SM, Henson-Garcia M, Valerio-Shewmaker MA, Messiah SE, Knell G (2022) Contributions of Trustworthiness, Health Literacy, and Self-Efficacy in Communicating With COVID-19 Vaccine-Hesitant Audiences: Web-Based Survey Study. JMIR Form Res 6: 38076.
- Shebehe J, Montgomery S, Hansson A, Hiyoshi A (2022) Low health literacy and multiple medications in community-dwelling older adults: A population-based cohort study. BMJ Open 12: 055117.
- Cheng BT, Tanna AP (2023) Association of Health Literacy and Healthcare Utilization Among Glaucoma Patients. J Glaucoma 32: 139-144.
- Abdullah A, Liew SM, Salim H, Ng CJ, Chinna K (2019) Prevalence of limited health literacy among patients with type 2 diabetes mellitus: A systematic review. PLoS One 14: 0216402.
- Meldgaard M, Gamborg M, Maindal HT (2022) Health literacy levels among women in the prenatal period: A systematic review. Sexual & Reproductive Healthcare 34: 100796.
- Rolova G, Gavurova B, Petruzelka B (2020) Exploring Health Literacy in Individuals with Alcohol Addiction: A Mixed Methods Clinical Study. Int J Environ Res Public Health 17: 6728.
- Griffey RT, Kennedy SK, McGownan LDG, Goodman MS, Kaphingst KA (2014) Is low health literacy associated with increased emergency department utilization and recidivism?. Academic Emergency Medicine 21: 1109-1115.
- Zaidman EA, Scott KM, Hahn D, Bennett P, Caldwell PH (2023) Impact of parental health literacy on the health outcomes of children with chronic disease globally: A systematic review. J Paediatr Child Health 59: 12-31.
- Hickey KT, Creber RMM, Reading M, Sciacca RR, Riga TC, et al. (2018) Low health literacy: Implications for managing cardiac patients in practice. Nurse Pract 43: 49-55.
- Lorini C, Buscemi P, Mossello E, Schirripa A, Giammarco B, et al. (2023) Health literacy of informal caregivers of older adults with dementia: Results from a cross-sectional study conducted in Florence (Italy). Aging Clinical and Experimental Research 35: 61-71.
- Gan W, Zhang Q, Yang D, Yin J, Wang Y, et al. (2022) A behavior change wheel-based interactive pictorial health education program for hypertensive patients with low blood pressure health literacy: Study protocol for a randomized controlled trial. Trials 23: 369.
- Kanejima Y, Shimogai T, Kitamura M, Ishihara K, Izawa KP (2022) Impact of health literacy in patients with cardiovascular diseases: A systematic review and meta-analysis. Patient Educ Couns 105: 1793-1800.
- Achstetter K, Köppen J, Haltaufderheide M, Hengel P, Blümel M, et al. (2022) Health Literacy of People with Substitutive Private Health Insurance in Germany and Their Assessment of the Health System Performance According to Health Literacy Levels: Results from a Survey. Int J Environ Res Public Health 19: 16711.
- Bosle C, Orth B, Reibling N, Merkel C, Muschalik C, et al. (2022) Health information behaviour and health literacy on COVID-19 vaccination of the general population in Germany-findings from the CoSiD study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 65: 1289-1298.
- O'Mara CS, Young JP, Winkelmann ZK (2022) Financial Health Literacy and the Shared Decision-Making Process in Healthcare. Int J Environ Res Public Health 19: 6510.
- Lossius MI, Alfstad KÅ, Aaberg KM, Nakken KO (2017) Discontinuation of antiepileptic drugs in seizure-free patients - when and how?. Tidsskr nor Laegeforen 137: 451-454.
- Caqueo-Urízar A, Urzúa A, Mena-Chamorro P, Fuente JBDL (2021) Effects of Adherence to Pharmacological Treatment on the Recovery of Patients with Schizophrenia. Healthcare (Basel) 9: 1230.
- Banerjee S, Varma RP (2013) Factors affecting non-adherence among patients diagnosed with unipolar depression in a psychiatric department of a tertiary hospital in Kolkata, India. Depression Research and Treatment 2013: 809542.
- Graeupner D, Coman A (2017) The dark side of meaning-making:How social exclusion leads to superstitious thinking. Journal of Experimental Social Psychology 69: 218-222.
- Puckree T, Mkhize M, Mgobhozi Z, Lin J (2002) African traditional healers: what health care professionals need to know. International Journal of Rehabilitation Research 25: 247-251.
- Taher M, Pashaeypoor S, Cheraghi MA, Karimy M, Hoseini ASS (2020) Superstition in health beliefs: Concept exploration and development. Journal of Family Medicine and Primary Care 9: 1325-1330.
- Grim BJ, Grim ME (2019) Belief, Behavior, and Belonging: How Faith is Indispensable in Preventing and Recovering from Substance Abuse. Journal of Religion and Health 58: 1713-1750.
- Mirahmadizadeh A, Delam H, Seif M, Banihashemi SA, Tabatabaee H (2019) Factors Affecting Insulin Compliance in Patients with Type 2 Diabetes in South Iran, 2017: We Are Faced with Insulin Phobia. Iranian Journal of Medical Sciences 44: 204-213.
- Anbesu EW, Asgedom DK (2023) Menstrual hygiene practice and associated factors among adolescent girls in sub-Saharan Africa: A systematic review and meta-analysis. BMC Public Health 23: 33.
- Garg S, Anand T (2015) Menstruation related myths in India: Strategies for combating it. J Family Med Prim Care 4: 184-186.
- https://theprint.in/health/less-than-20-per-cent-menstruating-girls-women-in-india-use-pads/
- Webdesk (2017) Can a campaign to remove tax on sanitary pads help Indian women adopt better hygiene? Zee Business.
- Patwa J, Pandit N (2018) Open Defecation-Free India by 2019: How Villages are Progressing?. Indian Journal of Community Medicine 43: 246-247.
- Belay DG, Asratie MH, Aragaw FM, Tsega NT, Endalew M, et al. (2022) Open defecation practice and its determinants among households in sub-Saharan Africa: Pooled prevalence and multilevel analysis of 33 sub-Saharan Africa countries demographic and health survey. Tropical Medicine and Health 50: 28.
- Upadhyay A (2019) From a luxury to suffocating, here are some unusual myths regarding toilets debunked. NDTV.
- Cuthino FL, Sheilini M, Chandrababu R (2021) The comparison of health literacy between health science and non-health Science members-a cross sectional study of multifaceted Public Health Affair. Clinical Epidemiology and Global Health 12: 100893.
- Mohiuddin AK (2022) Medication adherence: Fact or fictions?. Current Research in Public Health 2: 18-21.
- Fan JH, Lyons SA, Goodman MS, Blanchard MS, Kaphingst KA (2016) Relationship Between Health Literacy and Unintentional and Intentional Medication Nonadherence in Medically Underserved Patients With Type 2 Diabetes. Diabetes Educ 42: 199-208.
- ALSharit BA, Alhalal EA (2022) Effects of health literacy on type 2 diabetic patients' glycemic control, self-management, and quality of life. Saudi Medical Journal 43: 465-472.
- Tefera YG, Gebresillassie BM, Emiru YK, Yilma R, Hafiz F, et al. (2020) Diabetic health literacy and its association with glycemic control among adult patients with type 2 diabetes mellitus attending the outpatient clinic of a university hospital in Ethiopia. PLoS One 15: 023129.
- Ziapour A, Azar FEF, Mahaki B, Mansourian M (2022) Factors affecting the health literacy status of patients with type 2 diabetes through demographic variables: A cross-sectional study. J Educ Health Promot 11: 306.
- Mogessie HM, Gebeyehu MA, Kenbaw MG, Tadesse TA (2022) Diabetic health literacy and associated factors among diabetes mellitus patients on follow up at public hospitals, Bale Zone, South East Ethiopia, 2021. PLoS One 17: 0270161.
- Chiou SJ, Chang YJ, Liao K, Chen CD (2022) Modest association between health literacy and risk for peripheral vascular disease in patients with type 2 diabetes. Front Public Health 10: 946889.
- White RO, Wolff K, Cavanaugh KL, Rothman RL (2010) Addressing Health Literacy and Numeracy to Improve Diabetes Education and Care. Diabetes Spectrum 23: 238-243.
- Osborn CY, Cavanaugh K, Wallston KA, Rothman RL (2010) Self-efficacy links health literacy and numeracy to glycemic control. Journal of Health Communication 15: 146-158.
- Brockmeyer M, Wies E, Joerges J, Sommer J, Borgmann SO, et al. (2022) Knowledge of HbA1c and LDL-C treatment goals, subjective level of disease-related information and information needs in patients with atherosclerotic cardiovascular disease. Clinical Cardiology 46: 223-231.
- Miranda R, Meeks KAC, Snijder MB, Born BJVD, Fransen MP, et al. (2020) Health literacy and hypertension outcomes in a multi-ethnic population: the HELIUS study. Eur J Public Health 30: 545-550.
- Isa DM, Shahar S, He FJ, Majid HA (2021) Associations of Health Literacy with Blood Pressure and Dietary Salt Intake among Adults: A Systematic Review. Nutrients 13: 4534.
- Du S, Zhou Y, Fu C, Wang Y, Du X, et al. (2018) Health literacy and health outcomes in hypertension: An integrative review. International Journal of Nursing Sciences 5: 301-309.
- Halladay JR, Donahue KE, Cené CW, Li Q, Cummings DM, et al. (2017) The association of health literacy and blood pressure reduction in a cohort of patients with hypertension: The heart healthy lenoir trial. Patient Educ Couns 100: 542-549.
- Hoover DS, Vidrine JI, Shete S, Spears CA, Cano MA, et al. (2015) Health Literacy, Smoking, and Health Indicators in African American Adults. Journal of Health Communication 20: 24-33.
- Lincoln A, Paasche-Orlow MK, Cheng DM, Lloyd-Travaglini C, Caruso C, et al. (2006) Impact of health literacy on depressive symptoms and mental health-related: Quality of life among adults with addiction. J Gen Intern Med 21: 818-822.
- Rahman FI, Aziz F, Huque S, Ether SA (2020) Medication understanding and health literacy among patients with multiple chronic conditions: A study conducted in Bangladesh. J Public Health Res 9: 1792.
- Persell SD, Osborn CY, Richard R, Skripkauskas S, Wolf MS (2007) Limited health literacy is a barrier to medication reconciliation in ambulatory care. Journal of General Internal Medicine 22: 1523-1526.
- Lindquist LA, Go L, Fleisher J, Jain N, Friesema E, et al. (2012) Relationship of health literacy to intentional and unintentional non-adherence of hospital discharge medications. Journal of General Internal Medicine 27: 173-178.
- Kim M, Suh D, Barone JA, Jung SY, Wu W, et al. (2022) Health Literacy Level and Comprehension of Prescription and Nonprescription Drug Information. Int J Environ Res Public Health 19: 6665.
- Protheroe J, Nutbeam D, Rowlands G (2009) Health literacy: A necessity for increasing participation in health care. British Journal of General Practice 59: 721-723.
- Dalal PK (2020) Changing scenario of addiction psychiatry: Challenges and opportunities. Indian Journal of Psychiatry 62: 235-241.
- United Nations (2022) UNODC World Drug Report 2022 highlights trends on cannabis post-legalization, environmental impacts of illicit drugs, and drug use among women and Youth. United Nations.
- Lee J (2021) America has spent over a trillion dollars fighting the war on drugs. 50 years later, drug use in the U.S. is climbing again. CNBC United States.
- Rolova G, Gavurova B, Petruzelka B (2021) Health Literacy, Self-Perceived Health, and Substance Use Behavior among Young People with Alcohol and Substance Use Disorders. Int J Environ Res Public Health 18: 4337.
- Kinnunen JM, Paakkari L, Rimpelä AH, Kulmala M, Richter M, et al. (2022) The role of health literacy in the association between academic performance and substance use. Eur J Public Health 32: 182-187.
- Degan TJ, Kelly PJ, Robinson LD, Deane FP (2019) Health literacy in substance use disorder treatment: A latent profile analysis. J Subst Abuse Treat 96: 46-52.
- Devraj R, Herndon CM, Griffin J (2013) Pain awareness and medication knowledge: A health literacy evaluation. J Pain Palliat Care Pharmacother 27: 19-27.
- Mohiuddin AK (2022) Rational use of medications: Eccentric or non-existent? Mathews Journal of Pharmaceutical Science 6: 1-4.
- Rogers AH, Bakhshaie J, Orr MF, Ditre JW, Zvolensky MJ (2020) Health Literacy, Opioid Misuse, and Pain Experience Among Adults with Chronic Pain. Pain Medicine 21: 670-676.
- Sukrueangkul A, Panomai N, Laohasiriwong W, Sakphisutthikul C, Phimha S (2022) Factors Influencing Demand for Medical Cannabis Use among Cancer Patients in the North of Thailand. Asian Pac J Cancer Prev 23: 319-325.
- Lau SSS, Shum ENY, Man JOT, Cheung ETH, Amoah PA, et al. (2022) COVID-19-Related Health Literacy of School Leaders in Hong Kong: A Cross-Sectional Study. Int J Environ Res Public Health 19: 12790.
- Casigliani V, Arzilli G, Menicagli D, Scardina G, Lopalco PL (2020) Vaccine hesitancy and health literacy: We need to change our paradigm. European Journal of Public Health 30.
- Okan O, Messer M, Levin-Zamir D, Paakkari L, Sørensen K (2022) Health literacy as a social vaccine in the COVID-19 pandemic. Health Promot Int.
- Singh P, Dhalaria P, Kashyap S, Soni GK, Nandi P, et al. (2022) Strategies to overcome vaccine hesitancy: A systematic review. Syst Rev 11: 78.
- Lazarus JV, Wyka K, White TM, Picchio CA, Rabin K, et al. (2022) Revisiting covid-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nature Communications 13: 3801.
- Dhalaria P, Arora H, Singh AK, Mathur M, Singh AK (2022) COVID-19 Vaccine Hesitancy and Vaccination Coverage in India: An Exploratory Analysis. Vaccines (Basel) 10: 739.
- Zhang H, Li Y, Peng S, Jiang Y, Jin H, et al. (2022) The effect of health literacy on COVID-19 vaccine hesitancy among community population in China: The moderating role of stress. Vaccine 40: 4473-4478.
- Steinert JI, Sternberg H, Prince H, Fasolo B, Galizzi MM, et al. (2022) COVID-19 vaccine hesitancy in eight European countries: Prevalence, determinants, and heterogeneity. Sci Adv 8: 9825.
- Nguyen QC, Yardi I, Gutierrez FXM, Mane H, Yue X (2022) Leveraging 13 million responses to the U.S. COVID-19 Trends and Impact Survey to examine vaccine hesitancy, vaccination, and mask wearing, January 2021-February 2022. BMC Public Health 22: 1911.
- Becerra MB, Becerra BJ (2022) COVID-19 Vaccine Hesitancy among Behavioral Risk Takers. Vaccines (Basel) 10: 767.
- Kouvari K, Hadjikou A, Heraclidou I, Heraclides A (2022) Health literacy, consciousness, and locus of control in relation to vaccine hesitancy and refusal. European Journal of Public Health 32.
- Lin C, Tu P, Beitsch LM (2020) Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines (Basel) 9: 16.
- Khanna M (2020) Face masks makes people more careless with social distancing, reveals study. IndiaTimes.
- Mohiuddin AK (2020) Covid-19 and 20 resolutions for Bangladesh. European Journal of Sustainable Development Research 4: 0139.
- Esmaeilzadeh P (2022) Public concerns and burdens associated with face mask-wearing: Lessons learned from the COVID-19 pandemic. Progress in Disaster Science 13:100215.
- Lovelace B (2021) CDC says fully vaccinated people don't need to wear face masks indoors or outdoors in most settings. CNBC.
- Taylor S, Asmundson GJG (2021) Negative attitudes about facemasks during the COVID-19 pandemic: The dual importance of perceived ineffectiveness and psychological reactance. PLoS One 16: 0246317.
- Lewandowsky S, Holford D, Schmid P (2022) Public policy and conspiracies: The case of mandates. Curr Opin Psychol 47: 101427.
- Ray E (2023) Truckers protesting Covid mandates are amassing outside the capital. The New York Times. United States.
- Blaxill M, Rogers T, Nevison C (2022) Autism Tsunami: The Impact of Rising Prevalence on the Societal Cost of Autism in the United States. J Autism Dev Disord 52: 2627-2643.
- World Health Organization (2022) Autism. WHO.
- Lindly OJ, Cabral J, Mohammed R, Garber I, Mistry KB, et al. (2022) "I Don't Do Much Without Researching Things Myself": A Mixed Methods Study Exploring the Role of Parent Health Literacy in Autism Services Use for Young Children. J Autism Dev Disord 52: 3598-3611.
- Ozonoff S, Young GS, Steinfeld MB, Hill MM, Cook L, et al. (2009) How early do parent concerns predict later autism diagnosis?. J Dev Behav Pediatr 30: 367-375.
- Buffle P, Gentaz E, Vivanti G (2022) Perception, Beliefs, and Causal Attribution of Autism Early Signs in Ecuadorian General Population. Frontiers in Psychology 13: 915817.
- Chen YH, Chen Q, Kong L, Liu G (2022) Early detection of autism spectrum disorder in young children with machine learning using medical claims data. BMJ Health & Care Informatics 29: 100544.
- Valderrama A, Courcy I, Weis-Heitner L, Forgeot d'Arc B (2020) Health Literacy Issues of Parents Seeking Information on Autism Spectrum Disorder around Time of Diagnosis (Article in French). Sante Ment Que 45: 127-145.
- Vovou F, Hull L, Petrides KV (2021) Mental health literacy of ADHD, autism, schizophrenia, and bipolar disorder: a cross-cultural investigation. J Ment Health 30: 470-480.
- Hansen TM, Qureshi S, Gele A, Hauge LJ, Biele GP, et al. (2023) Developmental disorders among Norwegian-born children with immigrant parents. Child and Adolescent Psychiatry and Mental Health 17: 3.
- Keim-Malpass J, Letzkus LC, Kennedy C (2015) Parent/caregiver health literacy among children with special health care needs: A systematic review of the literature. BMC Pediatr 15:92.
Citation: Mohiuddin AK (2023) Health Literacy: The Most Neglected Essential Human Quality. J Community Med Public Health Care 10: 124.
Copyright: © 2023 Abdul Kader Mohiuddin, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

