
Hospital Reconversion of the Gastrointestinal Endoscopy Service at The National Medical Center November 20 Issste During the Covid-19 Pandemic
*Corresponding Author(s):
Teresa De Jesús Galicia GómezGastrointestinal Endoscopy Service 1 Floor. National Medical Center November 20 ISSSTE. Avenida Félix Cuevas, Colonia Del Valle Sur, Benito Juárez, CP, Benito Juárez Delegation, CDMX, Mexico
Tel:5536567534,
Email:galiciateresa120@gmail.com
Keywords
Endoscopy Services; Recommendations; Reconversion; Reinstatement; SARS-CoV-2
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is a respiratory illness caused by the SARS-CoV-2 virus. It has spread from Wuhan City, China to many other countries around the world, including Mexico. It has been characterized as pandemic by the World Health Organization (WHO) [1].
Due to the intensity and severity of the COVID-19 outbreak, health authorities worldwide took measures to try to mitigate the impact of the pandemic; which included social distancing, more strict hygiene practices and important adaptations and modifications in healthcare services, among others.
In order to attend the sanitary contingency, several actions where adopted in the healthcare system of the country, such as the Reorganization, Reconversion and Expansion of hospital services, which involved the development and implementation of strategies to provide safer and better conditions to healthcare workers, patients and their families. [PAN AMERICAN HEALTH ORGANIZATION PAHO/WHO. Recommendations for Reorganization and expansion of hospital services in the response to COVID-19. Washington D.C. 2020] /// [Lineamientos de Reconversión Hospitalaria. Gobierno de México. Secretaría de Salud. Abril, 2020].
The reorganization of health services is a set of actions deployed at every level of care that enhaces the ability to manage increasing numbers and complexity of cases. This operation requires the development of strategies for clinical and surgical services to identify and minimize specific exposure risks, sources of exposure, transmission routes and other features that may faclitate SARS-Cov2 transmission; such as the adaptation of facilities and constant updating and training of personnel. This action must also guarantee the capacity of the hospital and staff to attend potencially exacerbated conditions of the outbreak [1].
In the gastrointestinal Endoscopy Service at the National Medical Center 20 de Noviembre; adaptation of facilities and internal guidelines and protocols were performed accordingly to the WHO, the National Health Department (SSA) and the Gastrointestinal Endoscopy Mexican Association (AMEG) guidelines and recommendations for the proper care of uninfected, suspected and confirmed COVID-19 patients. This allowed the service to remain providing equitable access of essential health services during the emergency situation and thus limiting direct mortality and avoid indirect mortality among healthcare professionals.
This internal regulations against COVID-19 were planned and developed based on the traditional guidelines of the Occupational Safety and Health Administration (OSHA) of industrial hygiene and infection prevention practices. Focused on the need for workplaces to implement controls of administrative procedures, work practices and the use of Personal Protective Equipment (PPE) as well as the considerations to do so [1].
OBJECTIVES
- To assure that the health services workers KNOW the proper use of the advisory and operational guides of the different national (federal General Labor Law, ISSSTE, SSA, Federal Government) and International (WHO, WEO, ASGE, ESGE, OSHA) organizations and authorities, as well additional guidelines that may appear as the conditions of the COVID-19 outbreak change; including new information about the virus, its transmission and impact.
- IDENTIFY the risk levels in the workplace environments in order to determine the control measures that must be implemented.
- To ESTABLISH and compliance effective health and safety rules, regulations and policies so to have a workplace free of recognized risks that could cause serious physical harm or death.
- To DEVELOP a strategic preparedness and response plan against infectious diseases to PROVIDE QUALITY HEALTH CARE to adult and pediatric patients who attend the Gastrointestinal Endoscopy Service of this medical center during the SARS-Cov-2 pandemic; through the implementation of correct practices for the utilization and disposal of PPE and medical supplies, as well as adequate medical practice measures to prevent contagion among patients and the personnel.
- CONSTANT UPDATING on the rules, health and safety compliance regulation policies and the clinical care through the analysis of the obtained results in short and medium term compared to the national and international literature reports.
- PLANNING the restart of activities of the Service. Taking as principle a series of practical recommendations regarding the management and progressive re-introduction of healthcare activity, according the following basic principles:
- a) Protect patients from the risk of infection from SARS-Cov-2 and provide them with quality care.
- b) Gradually restore the normal operation of the service with the proper security measures, within the continuous risk environment of infection, considering daily needs, material (PPE) availability, the accumulated incidence of SARS-Cov-2 in Mexico City and the capacity of the hospital.
Spread of COVID-19
Although the first human cases of COVID-19 were likely the result of exposure to an infected animal, infected people can spread SARS-CoV-2 to other people moistly by droplets when coughing, sneezing or even talking when people are in close contact with each other (within about 6 feet or less from each other).
It may also be possible for a person to get COVID-19 by touching a surface or object which contains the virus on it and then touching their own mouth, nose, or possibly their eyes, nevertheless this is not believed to be the main way in that the virus spreading.
People can be most contagious when their symptoms are on the rise (e.g. fever, cough, and / or shortness of breath). Spread is also possible before people show symptoms onset.
Although the Federal Government has implemented public health measures to limit the spread of the virus, it is likely that certain person-to-person transmission will continue to occur [1-10].
Considering the maximum capacity of each medical unit in the country, Mexico´s Federal Government stablished guidelines to optimize material and human resources in order to guarantee the access of medical care to an increasing demand of COVID-19 patients. This was accomplished by dividing hospital reorganization into phases that allowed better adaptation to the dynamics of the pandemic and thus, assuring the maximum capacity of attention of critical patients (Figure 1). [Lineamiento de Reconversión Hospitalaria. 2020. Gobierno de México. Secretaría de Salud]
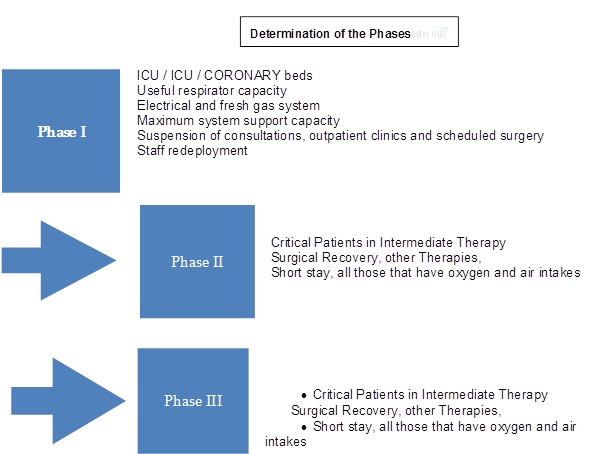 Figure 1: Determination of the Phases.
Figure 1: Determination of the Phases.
How the COVID-19 outbreak could affect economic activities
Similar to influenza viruses, SARS-CoV-2, which is the virus that causes COVID-19, has the potential to cause wide-ranging outbreaks. Under the condition person-to-person transmission, multiple areas of Latin America and other regions worldwide had simultaneously experience adverse conditions with multiple impacts in the daily activities of the countries [11,12].
Without a vaccine, this outbreak could be long-term event which can carry as a result many adverse consequences for workplaces, such as absenteeism due to sickness among workers or their families. This phenomenon may also be related to workers at high risk of complications or because of the necessity of taking care of elders’ relatives or children due to the closure of care-givers centers.
Companies and governments may also experience income decrease, interruptions of the supply/delivery chains and many other difficulties which can lead to negative effects for the financial situation of the people.
Among the many adversities of a pandemic, one of the special interests is the shortage of medical items due to the increasing demand of the people and health services, while the demand of other products significantly decreases. This is aggravated because of delaying or sudden cancelation of supply shipments from distant geographic areas that were severely affected by the coronavirus [13].
Strategy to reduce the risk of exposure of health personnel to SARS-CoV-2
Based on aerosol-generating procedures, the risk of exposure of staff activities was classified into low, medium, high and very high risk of exposure accordingly to the recommendations of the WHO, the Mexican Association of Gastrointestinal Endoscopy ¨AMEG¨, General Labor Law and (Institute of Security and Social Services for State Workers) ISSSTE´s statutes for health workers.
Furthermore, a preparation and response plan were developed; focused on training the service´s personnel and the compliance of protocols for the attention of the patients in the Gastrointestinal Endoscopy Service during phase 3 of SARS-Cov-2 pandemic.
The specific plans of the Workplace to reduce associated risk of the service´s collaborators were based the most recent information and recommandations of the WHO, AMEG, ASGE, ESGE, which especifies the areas and work tasks that health workers can perform, as well as where, how and to what sources of SARS-Cov-2 the personnel could be exposed [14,15].
Occupational Health and Safety
The improvements to the Endoscopy Service were focused on avoiding the sustained transmission of SARS-Cov-2 among health workers due to unprotected exposure to confirmed or suspected COVIS-19 patients, considering the following factors:
• Non-occupational risk factors at home or in community settings.
• Individual risk factors (e.g. advanced age, chronic medical conditions, including compromised immune system, pregnancy, metabolic diseases, etc.).
• The controls necessary to address these risks.
• The observation of authorities´ recommandations regarding the development of contingency plans for risk situations, such as :
- Social distancing, staggered work shifts, reduction of operations, remote service provision, and other exposure-reducing measures.
- Options for conducting essential operations with a reduced workforce, including the training in multiple job areas to continue or increase operations services.
- Scheduling of endoscopic procedures.
Plans also consider and address further actions that employers can take to reduce the risk of exposure to the virus in their workplaces, described in the following sections [16].
GUIDELINES ON WORKPLACE PREPARATION AGAINST COVID-19
The most important action is to implement basic measures to prevent infections [1]
Although there is no OSHA, WHO, AMEG standard that specifically refers to SARS-CoV-2, some OSHA requirements may apply to prevent occupational exposure to the virus. Among the most relevant are:
- • OSHA standards for Respiratory Protective Equipment (PPE) which require the use of gloves, eye and face protection, and respiratory protection. See: osha.gov/laws-regs/ regulations / standard number / 1910 # 1910_Subpart_I.
- • The General Duty Clause, Section 5 (a) (1) of the Occupational Safety and Health Act of 1970, 29 USC 654 (a) (1), which requires employers to provide every worker with a job and workplace that is free from recognized hazards that are causing or likely to cause death or serious physical harm. osha.gov/laws-regs/oshact/completeoshact.
- • OSHA's Standard for Bloodborne Pathogens (29 CFR 1910.1030) applies to occupational exposure to human blood and other potentially infectious materials that typically do not include respiratory secretions that could transmit SARS-CoV-2. However, the provisions of the standard provide a working scheme that can help control some sources of the virus, including exposures to body fluids and secretions. osha.gov/laws-regs/ regulations / standard number / 1910 / 1910.1030.
- • For the preservation of records and criteria for the registration of injuries / illnesses and the applications of standards related to sanitation and risk communication related to chemical risks that could be present in common disinfectants and sterilizers. osha.gov/SLTC/covid-19/standards.html.
The level of risk depends on the need for contact within 2 meters of persons known or suspected to be infected with SARS-CoV-2, or the requirement for prolonged repeated contact with persons known or suspected to be infected [18,19,20].
The risk to workers from occupational exposure to SARS-COv-2 during an outbreak could range from very high, high, medium or low risk and proper measures shall be taken accordingly to OSHA, WHO, SSA and ISSSTE recommendations [21].
OSHA´s Occupational risk pyramid divides job tasks into four risk exposure levels as shown below (Figure 2)
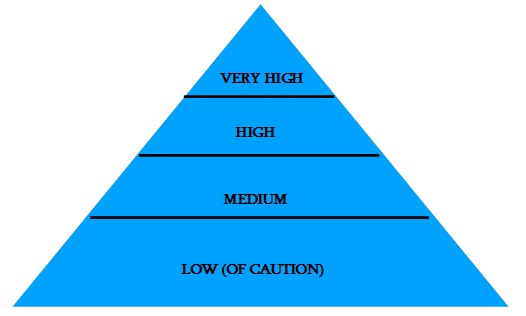 Figure 2: Occupational risk pyramid for COVID-19.
Figure 2: Occupational risk pyramid for COVID-19.
Very high risk of exposure
Jobs with a high potential for exposure to known or suspected sources of COVID-19 during specific medical, postmortem or laboratory procedures [22].
Workers in this category include:
• Healthcare and morgue workers performing aerosol-generating procedures on or collecting/handling specimens from potentially infectious patients or bodies of people known to have, or suspected of having COVID-19 at the time of death. The aforementioned activities are considered to be performed in our service.
High exposure risk
Jobs with a high potential for exposure to known or suspected sources of COVID-19. Workers in this category include:
- • Healthcare delivery, healthcare support, medical transport and mortuary workers exposed to known or suspected COVID-19 patients or bodies of people known to have, or suspected of having COVID-19 at time of death.
Medium exposure risk
Jobs that require frequent/close contact with people who may be infected, but who are not known or suspected patients. Workers in this category include :
- • Those who may have contact with the general public (e.g. schools, high-population-density work enviroments, some high-volume retail settings), including individuals returning from locations with widespread COVID-19 transmission.
Lower exposure risk
Jobs that do not require contact with people known to be, or suspected being infected.
- • Workers in this category have minimal occupational contact with the public and other coworkers.
OCCUPATIONAL HEALTH AND SAFETY ADMINISTRATION
Engineering controls on endoscopy, anesthesiology and monitor equipment.
Installing physical barriers such as clear plastic protective covers against aerosols and filters of high efficiency on the anesthesiology machine (Figure 3,4).
 Figure 3: Installation of physical barriers.
Figure 3: Installation of physical barriers.
 Figure 4: Engineering controls on endoscopy, anesthesiology and monitor equipment.
Figure 4: Engineering controls on endoscopy, anesthesiology and monitor equipment.
Administrative controls of the Gastrointestinal Endoscopy Service
- • Placement face masks to all members of the Service, Physicians from other services and patients in order to contain respiratory secretions until they leave the Service.
- • Only one patient will be attended at the service requesting another patient until the previous patient has leaved the service, in order to avoid cross-infection between patients.
- • The presence of family members and Physicians from other services is not allowed in the service during the endoscopic procedures and until the service disinfection.
- • Provide the treating physician with forms of informed consent of endoscopic and anesthesiology during the scheduling of the procedure.
- • Reception of patients with signed informed consent and nursing records, based on the electronic file of the unit.
- • Keep informed the patients informed about COVID-19 symptoms and ask sick patients to minimize contact with workers [10].
Preparing workplaces against COVID-19 virus
Placement of green indicators of ROUTE COVID for the reception and transfer of patients, and red indicators for route NO COVID and the movement of health personnel during the operation of the Service. (Figure 5,6,7)
 Figure 5: Workplaces against COVID-19 virus.
Figure 5: Workplaces against COVID-19 virus.
 Figure 6: Placement of green indicators of ROUTE COVID for the reception and transfer of patients, and red indicators for route NO COVID.
Figure 6: Placement of green indicators of ROUTE COVID for the reception and transfer of patients, and red indicators for route NO COVID.
 Figure 7: The movement of health personnel during the operation of the Service.
Figure 7: The movement of health personnel during the operation of the Service.
Personal protective equipment (PPE)
Jobs classified at Lower Exposure risk (caution)
Additional PPE is not recommended for workers in the lower exposure risk group. Workers should continue to use the PPE, if any, that they would ordinarily use for other job tasks. [Guidance on Preparing Workplaces for COVID-19. 2020. US Department of Labor. Occupational Safety and Health Administration].
Jobs classified at high or Very High risk of exposure:
Most workers at extremely high or high exposure risk may need to wear come combination of radiation protection equipment (Figure 8), gloves, gown, face mask and/or a face shield or goggles (Figure 9). PPE ensembles for workers in the medium exposure risks category will vary by work task, the results of the employer´s hazard assessment, and the types of exposures workers have on the job. (Figure 10,11).
 Figure 8: Workers at extremely high or high exposure risk may need to wear combination of radiation protection equipment.
Figure 8: Workers at extremely high or high exposure risk may need to wear combination of radiation protection equipment.
 Figure 9: Protection equipment’s; gloves, gown, face mask and/or a face shield or goggles.
Figure 9: Protection equipment’s; gloves, gown, face mask and/or a face shield or goggles.
 Figure 10: PPE ensembles for workers in the medium exposure risks category.
Figure 10: PPE ensembles for workers in the medium exposure risks category.
 Figure 11: The types of exposures workers have on the job.
Figure 11: The types of exposures workers have on the job.
Recommendations to minimize the risk of infection
- • Periodic screening; at least two PCR Detections separated in time before the restart of activities.
- • All participants in the Endoscopy Service must always carry surgical mask, body protection with surgical clothing and closed shoes (specific for hospital use). This protect the personnel and prevents them from serving as transmission vectors inside and outside the hospital.
- • Healthcare personnel with respiratory symptoms and / or fever and / or with suspected recent contact without the proper protective equipment with a person infected with SARS-CoV-2 (patient, companion or professional) should notify the as soon as possible to the person responsible for the service and be evaluated by the unit's respiratory triage. In no case will go to the Endoscopy service with this suspicion.
- • Social distancing and other measures must be maintained recommended during this pandemic and the number of professionals in direct contact with patients should be limited as much as possible, both during hospitalization and at the time of performing diagnostic or therapeutic procedures.
- • Professionals under study for clinical suspicion or confirmed COVID-19 even with a negative PCR test should not present at work, until 14 days after the onset of symptoms. The repetition or not of a diagnostic test will be indicated by the preventive medicine service.
- • Minimize contact between health personnel. Only the essential personnel for the procedure (doctor, nurse, endoscopy equipment rental service personnel and anesthesiologist, if applicable) should remain in the endoscopy room [23].
Recommendations regarding the management of Outpatients
- • Patients must go alone, unaccompanied, except in the case of a dependent patient (disabled or in need of an interpreter). In no case, the patient must have more than one companion, ideally, under 50 years of age.
- • The patient must always wear a mask and wash their hands before entering the consultation with 70% alcohol-gel solution.
- • Examine only essential patients and do it in that case with all the adequate protection (gloves, hand washing with 70% alcohol-gel solution). Cleaning the stretcher with disinfectant after the examination and ensure a table as clear as possible, which facilitates adequate cleaning of exposed surfaces on a regular basis.
- • Until the FOURTH PHASE OF HEALTH EMERGENCY, including this one, the number of face-to-face appointments should be reduced, increasing the interval between them through telemedicine and telephone consultations to the service to avoid crowds in the waiting room.
- • Avoid prescribing the greater number of complementary examinations that are not strictly necessary and / or consider increasing the interval between such scans. (protocols for research, study and follow-up, scheduled review of portal hypertension, colon cancer screening)
- • Telemedicine and other valuable healthcare formats should be promoted to the patient and minimize the risks of contagion, both with patients directly and with Health centers.
Indications that cannot be postponed for endoscopy
- Unstable digestive bleeding and/or high transfusion requirement, in which it is possible perform endoscopic therapy
- Acute esophageal obstruction (foreign bodies, punctate stenosis, cancer where the prosthesis is necessary)
- Endoscopic therapy in perforations/leaks.
- ERCP (± EUS) in acute cholangitis/jaundice secondary to biliary obstruction malignant / benign
- ERCP (± EUS) in acute biliary pancreatitis and/or cholangitis with stones and jaundice
- Infected pancreatic collections/WON
- Nutritional support considered urgent in hospitalized patient (PEG SNY)
- Gastrointestinal obstruction for decompression and/or prosthesis placemen
a) The type of endoscopic procedure.
• It is key to be able to define the different types of endoscopic procedures depending on the different situations regarding to the pandemic due to the SARS-CoV-2 infection. Considering that the urgent procedures have remained in the most problematic phase.
• There are 3 different phases of endoscopic procedures to be performed, depending on the reactivation phase of the endoscopy units, and the circumstances of the SARS-CoV-2 infection [13]. The transition between the different phases will depend directly about the situation of each of the hospitals with respect to the situation.
- • Phase I: Unit that can initiate the recovery of the regulated activity. Part of this activity will be conditioned by the availability of beds for urgent hospitalization (complications) or regulated (ERCP, prosthesis placement, etc.) and by the activity of other services (surgery, oncology) not delayed.
- • Phase II: normalization of the regulated activity. In this it would be possible to enter regulated activity without programming urgency.
- • Phase III: normality is fully recovered. Low-risk screening and follow-up protocols are restarted.
b) Schedule readjustment strategy. An essential point is the adjustment of the scheduling of procedures, related to the times applied to endoscopic procedures.
Estimate the time needed to change clothes, cleaning equipment and the room, disinfection, avoiding accumulation of patients in the waiting room, etc. The proposal in this sense is the following, considering the risk of transmissibility and the need for cleaning and / or protection measures in case of having patients with high risk patients:
- • Phase I: try to achieve 50% of the usual activity of the endoscopy unit.
- • Phase II and III: try to reach 75% of the activity of the unit of endoscopy. In order to define the times between procedures, in case of performing a high-risk patient, a minimum of 45 minutes per patient should be added to what was established according to the EFICAD study [24].
C) Patient management:
Scheduling: patients will be called the day before the endoscopy, to make a risk checklist, which will be repeated the day they come to perform the procedure. Undoubtedly, the ideal scenario, which we must reach, is the practice of a SARS-CoV-2 test on all patients before the procedure.
Access to the endoscopy unit: upon admission to the endoscopy service, the patient will be fitted with a surgical mask, hands washing with alcohol-gel solution and their temperature will be taken.
|
Low Risk |
Patient cured of SARS Cov2 infection |
|
Intermediate Risk |
Anyone without respiratory symptoms or fever |
|
High risk |
Anyone with respiratory symptoms or fever with or without contact with people infected with Sars Cov2 Patient with a positive diagnosis of Sars Cov2 |
Table 1: Stratification of the risk of transmission of SARS-Cov2 infection in patients undergoing gastrointestinal endoscopy.
Safety during the Endoscopy
1) The type of endoscopic examination and the patient determines the risk of spreading the infection.
- • Type of patient. The risk of transmission by type of patient can be seen in Table 1.
- • Type of procedure. Two types of procedures should be distinguished based on the ability to generate aerosols:
- • Aerosol generators, which are those linked to upper endoscopy (ERCP, gastroscopy, upper endoscopic ultrasound, upper enteroscopy) are considered high risk. If possible, all high scans should be sedated to reduce the risk of aerosol generation.
- • Low-aerosol generators that are those linked to low endoscopy (colonoscopy, low enteroscopy, low endoscopic ultrasound) or by ostomies are considered low risk [3,2].
2) Level of protection.
- • A level of protection must be used from the access to the endoscopy unit, which includes the common areas (administrative area, corridor, living area, laundry area, recovery area). Protection of nose with a mask, body protection with surgical clothes and cover-up, and single-use hospital footwear are recommended. The continued use of gloves would not be necessary, but frequent hand washing.
- • Once in the room, the level of protection will vary depending on the risk assigned to patient and procedure. (32-34)
- • Low risk: a mask, face protection (goggles or face mask), disposable hat, body protection (pajamas + gown +/- waterproof gown), gloves, specific closed shoe would be required.
- • Intermediate risk: mask preferably N95 (FFP2 / FFP3), face protection (goggles or face mask), disposable cap, body protection (disposable surgical clothes + disposable cover-gown +/- waterproof gown), double glove, tights with specific closed shoes would be required.
- • High risk: mask type N95 / FFP2 / FFP3 would be required), face protection (glasses or face mask), disposable cap, body protection (disposable surgical clothes + disposable gown cover + waterproof gown), double glove, tights with specific closed shoes.
3) Place of performance of endoscopic procedures.
- • Endoscopic procedures of the Low and intermediate risk patients are performed in a manner routine in the Endoscopy Services area, taking the necessary precautions.
- • In case of requiring a procedure to be performed on a patient with a high risk (SARS-CoV-2 + confirmed or investigated), depending on the infrastructure and availability needed for the endoscopy procedure (e.g. fluoroscopy) we can:
- Carry out the endoscopic study in a room dedicated by the hospital usually in the COVID AREA or ICU.
- Carry out the endoscopic study in the endoscopy unit itself. In this case, it would be advisable to allocate a single room to these patients, the procedures being carried out in the spaces designated at the end of the agenda, and reserve time/resources for cleaning and disinfection of the room.
Cleaning and processing of rooms and equipment.
- • The recommendation of scientific societies is that endoscopes and reusable consumables undergo a standardized reprocessing and disinfection procedure with bactericidal, mycobactericidal, fungicidal and virucidal properties, thereby minimizing the risk of transmission of any type of virus.
- • Channel cleaning brushes should be single-use and plastic connections to the suction should be discarded.
- • The endoscopes must go to the cleaning area leaving the room in a closed transport (for example, plastic bag), being carried out upon arrival at the disinfection room an immediate manual washing prior to its introduction into the automated washing system.
- • Cleaning and disinfection of the surfaces with which it has been contact the patient or their secretions and staff with bleach or sodium hypochlorite solution containing 1000 ppm of active chlorine and there must be a differentiated circuit for the waste generated will be eliminated and managed in accordance with regulations relevant laws [14-16].
|
Upper endoscopy: 30 minutes Therapeutic high endoscopy: 45 minutes Upper endoscopic ultrasound: 40 minutes Colonoscopy: 45 minutes Therapeutic Colonoscopy: 60 minutes ERCP, Therapeutic Endoscopy: 120 minutes |
Suggested times according to the type of endoscopic procedure.
Table 2: Table of Intervals between endoscopic procedures according to EFICAD.
CONCLUSIONS
Due to the speed and scale of transmission, COVID-19 appears to be much more infectious than other respiratory viruses (SARS) and it is known that between 5 to 85% of patients with positive tests for the Sars-Cov-2 virus will be asymptomatic, mainly children and young adults, appropriate health measures to the health systems were published to break the cycle of contagion In the Official Gazette of the Mexican Federation on March 17 of 2020, the measures in the search for a comprehensive approach appropriate to the circumstances that may eventually arise in the medical units, based on responsible and informed action that allows ISSSTE to align its resources throughout the country to the containment effort carried out by the health authorities of the country and the world.
The Institute of Security and Social Services for State Workers (ISSSTE) and the Endoscopy Service of the National Medical Center 20 de Noviembre must continue with the development of its essential functions, as well as with the inherent activities in order to ensure that the activities are carried out with the minimum essential personnel, through the implementation of face-to-face guards in cases to attend cases that by their nature are urgent and in other cases by carrying out the work through telemedicine, with the support of technological and communication tools.
From the healthcare point of view, the management of the Endoscopies are the most complex part of digestive services. It is obligatorily in person, implies a risk for patients and workers. For the return to normalization we must bear in mind that this is not due to the overcoming the pandemic situation but rather a situation of normalization of the rate of infection that decreases hospital saturation, which in turn can allow recover the regular hospital activity. We must remember in every time that the risk of infection could persist in patients and professionals and for this reason, we must be kept general measures as maintain the social distance and personal protective equipment. The implementation of face-to-face guards and the organization of work will be defined by the heads of the Executive Directorates, Technical Units and decentralized bodies that make up this Institute.
PLANNING OF THE RESTART OF ACTIVITIES
Having as a principle a series of practical recommendations regarding the management and the RETURN in a slow and progressive manner from the healthcare activity, which should follow the following basic principles:
1.- Protect patients from the risk of infection from SARS-Cov-2 and provide them with quality care.
2.- Restore slowly the normal operation of the Service in an environment of continuous risk due to SARS-Cov-2 virus based on: daily needs, material availability (PPE) and based on the accumulated incidence of COVID-19 in Mexico City and the burden that the epidemic has caused in the hospital.
It is crucial to consider the amount of resources allocated in the hospital to the care of COVID-19 patients and how the recovery of those spaces for non-COVID care is planned. When opening agendas in hospital's contingency plan must be considered to recover non-COVID areas as COVID areas in case of appearance of a new peak. On the other hand, the number of professionals available in the unit itself and the risk of infection for them. A key point is the need for endoscopy units have all the necessary material to increase the activity (at least 3 PPE for doctor, nurse and assistant per (or 4 if more staff is required: anesthesia, nursing, etc.) Without that adequate minimum material, endoscopic procedures should not be performed.
REFERENCES
- Guide on Preparing Workplaces for the COVID-19 virus. US Department of Labor Occupational Safety and Health Administration. OSHA 3992-03 2020.
- WEO COVID-19 Response Taskforce.
- Gralnek IM, Hassan C, Beilenhoff U, Antonelli G, Ebigbo A, et al. (2020) ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID-19 pandemic. ESGE.
- Zhang Y, Zhang X, Liu L, Wang H, Zhao Q (2020) Suggestions of infection prevention and control in digestive endoscopy during current 2019-nCoV pneumonia outbreak in Wuhan, Hubei Province, China. Endoscopy 52: 312-314.
- Repici A, Maselli R, Colombo M, Gabbiadini R, Spadaccini M, et al. (2020) Coronoavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc 92: 192-197.
- Luo S, Zhang X, XU H (2020) Don’t overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19). Clin Gastroenterol Hepatol 18: 1636-1637.
- Soetikno R, Teoh AYB, Kaltenbach T, Lau JYW, Asokkumar R, et al. (2020) Considerations in performing endoscopy during the COVID-19 pandemic. Gastrointest Endosc 92: 176-183.
- Kahi Charles J (2020) Endoscopy during the COVID-19 pandemic. Gastrointest Endosc.
- Infection Prevention Process for people with Covid-19 (SARS-CoV-2 disease), contacts and health personnel.
- CDC / NIOSH Guide to Optimizing Respirator Supplies. CDC.
- General of the National Electoral Institute, which determines as an extraordinary measure the suspension of deadlines inherent to the activities of the electoral function, due to the health contingency derived from the coronavirus pandemic, COVID-19.
- Health Safety Guidelines in the Work Environment. Government of Mexico.
- Crespo J, Andrade R, de Las Parras FA, Balaguer F, Acosta MB, et al. (2020) Restoration of activity in the digestive services. Recommendations of the SEPD, AEEH, GETECCU and AEG. Rev Esp Enferm Dig 112: 397-411.
- BSG expanded consensus advice for the management of IBD during the COVID-19 pandemic. British Society of Gastroenterology.
- Calvet X, Panés J, Alfaro N, Hinojosa J, Sicilia B, et al. (2014) Delphi consensus statement: Quality Indicators for Inflammatory Bowel Disease Comprehensive Care Units. J Crohns Colitis 8: 240-251.
- Han J, Wang Y, Zhu L, Cui Y, Li L, et al. (2020) Preventing the spread of COVID-19 in digestive endoscopy during the resuming period: meticulous execution of screening procedures. Gastrointest Endosc 92: 445-447.
- Cheung KS, Hung IF, Chan PP, Lung KC, Tso E, et al. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples from the Hong Kong Cohort and Systematic Review and Meta-analysis. Gastroenterology 159: 81-95.
- Sociedad Española de Patología Digestiva; Asociación Española de Gastroenterología. (2020) Recommendations by the SEPD and AEG, both in general and on the operation of gastrointestinal endoscopy and gastroenterology units, concerning the current SARS-CoV-2 pandemic (March, 18). Rev Esp Enferm Dig 112: 319-322.
- Beilenhoff U, Biering H, Blum R, Brljak J, Cimbro M, et al. (2018) Reprocessing of flexible endoscopes and endoscopic accessories used in gastrointestinal endoscopy: Position Statement of the European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastroenterology Nurses and Associates (ESGENA) - Update 2018. Endoscopy 50: 1205-1234.
- Zhang C, Shi L, Wang FS (2020) Liver injury in COVID-19: Management and challenges. Lancet Gastroenterol Hepatol 5: 428-430.
- AASLD (2020) Clinical insights for hepatology and liver transplant providers.
- National Transplant Organization.
- D’Antiga L. Coronaviruses and immunosuppressed patients. The facts during the third epidemic. Liver Transpl 26: 832-834.
- Recommendations for the programming of surgery under safe conditions during the transition period of the covid-19 pandemic.
Citation: Galicia-Gómez TJ, Suárez-Cuenca JA, Araujo-Gutiérrez EC, Rodríguez-Izaguirre R and Díaz-Juárez G (2020) Hospital Reconversion of the Gastrointestinal Endoscopy Service at The National Medical Center November 20 Issste During the Covid-19 Pandemic. J Gastroenterol Hepatology Res 5: 030.
Copyright: © 2020 Teresa de Jesús Galicia Gómez, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

