
How to Select Herbal Formulations that are Effective in Treating Hot Flashes: A Retrospective Study over 12 Years
*Corresponding Author(s):
Tetsuya IsobeMinatomirai Yume Clinic, Yokohama, Kanagawa, Japan
Email:iso12-7@blue.ocn.ne.jp
Abstract
In routine practice, selecting a Kampo treatment for hot flashes can be challenging. Subjects of this study were 890 cases out of 572 patients who received Kampo treatment for hot flashes by first author. Patients were asked if they had undergone bilateral oophorectomy/if they were receiving medication for pseudomenopause, if they were premenopausal, if they had “cold in the lower body,” and if they had irritability. Toki-shakuyaku-san, Keishi-bukuryo-gan, and Kami-shoyo-san have been selected as the 3 main herbal formulations as a Kampo extracts for hot flash. If patients failed to respond to these 3 medications, Oren-gedoku-to or Nyoshin-san was selected. In this study, formulations were prescribed based on a draft protocol the first author had prepared on his experience prior to the start of the study. Based on the results of this study, the protocol was improved to be more efficient. The most effective medication for patients who had undergone bilateral oophorectomy/who were receiving medication for pseudomenopause was Keishi-bukuryo-gan, the most effective medication for premenopausal patients was Toki-shakuyaku-san, the most effective medication for postmenopausal patient with irritability was Kami-shoyo-san., and the most effective medication for postmenopausal patient with “cold in the lower body” was Keishi-bukuryo-gan.
Keywords
Kami-shoyo-san; Oren-gedoku-to; Keishi-bukuryo-gan; Nyoshin-san; Toki-shakuyaku-san
Introduction
Hot flashes are a physical symptom typical of menopause and are thought to be caused by an autonomic imbalance due to decreased Estrogen (E) levels. The symptoms are flushing and a warm sensation from the neck up and sweating. Hormone Replacement Therapy (HRT), which supplements hormones like E, has been commonly used to treat hot flashes and is considered effective for menopausal symptoms [1-3]. For menopausal women who have had their uterus removed, E, the follicular hormone, is administered alone. For women who still have their uterus, a method has been established whereby Progesterone (P), the luteal hormone, is administered either cyclically or continuously in addition to E. The rationale for this is because research has found that administering E alone increases the risk of endometrial cancer, but adding progesterone reduces this risk. HRT was also previously thought to increase the risk of breast cancer. Other reported risks of HRT include an increased risk of myocardial infarction and cerebral infarction. A drawback of this therapy is that cyclic administration of E and P can cause withdrawal bleeding at regular intervals even in postmenopausal women causes and that continuous administration of E and P can cause occasional abnormal vaginal bleeding.
Women who have undergone bilateral oophorectomy or who are receiving pseudomenopause therapy with a GnRH agonist or antagonist are prone to hot flashes. Recently, nonhormonal therapy is developing such as Antidepressant [4-7]. It has been reported that exercise and Yoga are effective for hot flashes [8].
Several herbal formulations have long been known to be effective in treating hot flashes [9-22]. Many herbal formulations are used as a package called Kampo extracts in Japan. Adverse reactions as a result of taking these herbal formulations are rarely noted, so the number of patients wishing to receive Kampo treatment has increased over the past few years.
The 3 main herbal formulations prescribed for hot flashes are Toki-shakuyaku-san, Keishi-bukuryo-gan, and Kami-shoyo-san [11]. Other effective formulations include Oren-gedoku-to, Nyoshin-san [22] The efficacy of these 3 main herbal formulations in treating hot flashes has been found to be comparable to that of HRT. However, a definitive protocol for selecting which herbal formulation to prescribe first to patients with hot flashes has not been established. Based on the results of the current study, the author aims to determine whether a draft protocol that was used as the prescribing criteria in this study is valid or not and to devise an improved protocol that can more efficiently identify formulations that are effective at treating hot flashes.
Subjects And Methods
Subjects of this study were 890 cases out of 572 patients seen by first authors between May 2012 and September 2024. The number of cases is the number of patients who were initially prescribed a Kampo formulation for the first time. The Kampo formulations assessed in this study were Toki-shakuyaku-san, Keishi-bukuryo-gan, and Kami-shoyo-san, which were the 3 main herbal formulations prescribed, as well as Oren-gedoku-to and Nyoshin-san.
Patients’past medical history was reviewed to see whether or not they had undergone bilateral oophorectomy. The history of their present illness was reviewed to see if they were receiving a medication that causes pseudomenopause, such as a GnRH agonist/antagonist. Patients were interviewed regarding the status of the menstrual cycle. whether the patient was premenopausal or postmenopausal was determined by measuring follicle-stimulating hormone (FSH) and estrogen (E), whether they had chills or not and the site of those chills, and whether they were irritable or not were interviewed. A lack of menstruation for at least 2 years or FSH ≥40 mIU/ml and E ≤ 20 pg/ml in a blood hormone test was deemed to indicate menopause. Premenopause is a state in which a woman is not yet fully menopausal, and it includes the period of irregular menstruation leading up to menopause.
During the initial visit, patients were first prescribed 3 packets of an extract per day (7.5 g in total), divided into 3 doses (the standard dose of an extract from Tsumura), for one month. Upon the return visit a month later, the patient was asked about a reduction in hot flashes. If they had not decreased at all, the herbal formulation was switched to another medication prescribed. If the first medication prescribed reduced hot flashes but not sufficiently so, the dosage was increased to 4 packets per day (10 g in total), divided into 2 doses, and a new one-month supply was prescribed. The same procedure was followed during subsequent visits. The dosage was increased to 6 packets per day (15 g in total), divided into 3 doses in case that the effectiveness was incomplete with 4 packets per day.
The draft protocol used for prescribing in this study is shown in figure 1. The protocol was prepared by the first author based on his experience treating hot flashes. This study was conducted in accordance with the belief that the optimal Kampo treatment for individual patients with hot flashes could be provided by selecting the initial medication to prescribe based on this draft protocol. Data obtained over a period of 13 years were retrospectively analyzed. To determine the specific Kampo extract to prescribe first, the interview was emphasized, and Keishi-bukuryo-gan was prescribed for patients who had undergone bilateral oophorectomy or who were receiving pseudomenopause therapy. For other patients, the formulation was selected as follows: Toki-shakuyaku-san was prescribed for premenopausal patients, Keishi-bukuryo-gan was prescribed for postmenopausal patients with “cold in the lower body,” Kami-shoyo-san was prescribed for postmenopausal patients who were irritable, and Toki-shakuyaku-san was prescribed for postmenopausal patients with no cold in the lower body and who were not irritable. When there was uncertainty over whether to prescribe Keishi-bukuryo-gan or Kami-shoyo-san for postmenopausal patients who had “cold in the lower body” and who were irritable, Keishi-bukuryo-gan was prioritized. If the patient failed to respond to the first or second medication prescribed, the formulation that had not been used among the 3 main formulations prescribed for hot flashes was prescribed as the third medication. If the patient failed to respond to all 3 of the main prescriptions for hot flashes, Oren-gedoku-to was prescribed during the first half of this study (until the end of 2017) and Nyoshin-san was prescribed during the latter half (2018 and afterwards).
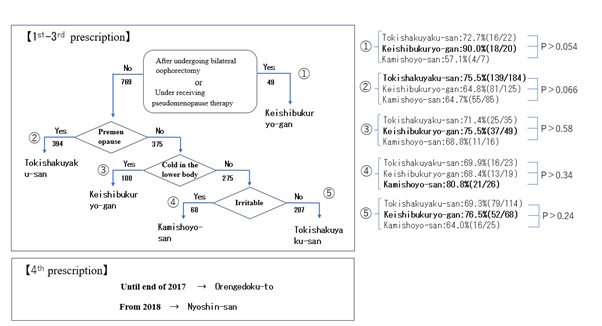
Figure 1: The draft protocol and flow diagram for selection of formulations for hot flashes.
Once the effectiveness of an herbal formulation plateaued, patients were asked about their level of satisfaction with the effectiveness of treatment, with 100% representing the highest level of satisfaction. Patients whose level of satisfaction was 60% or higher were deemed to be responders. Effective rate was defined as the proportion of responders, and efficacy was defined as the average level of satisfaction among responders. Methods using the level of satisfaction to assess the effectiveness of treatment have been reported in previous studies [23,24]. The definitions used here are based on a study in which 255 randomly selected patients were asked about their level of satisfaction with treatment while simultaneously having them select one of the following 6 levels of improvement levels indicated by the attending physician [25]. The 6 levels of improvement were: “ (1) Symptoms disappeared, (2) Symptoms almost disappeared, (3) Symptoms decreased considerably, (4) Symptoms decreased, (5) Symptoms decreased slightly, and (6) Symptoms have decreased.” As compared with these 6 levels of improvement and patient satisfaction, 86.7% (163/188) had a level of improvement of (1)-(2) which correlated with a level of satisfaction of 90-100%, 84.6% (132/156) had a level of improvement of (2)-(3) which correlated with a level of satisfaction of 80-90%, 94.7% (89/94) had a level of improvement of (3)-(4) which correlated with a level of satisfaction of 70-80%, 90.7% (68/75) had a level of improvement of (4)-(5) which correlated with a level of satisfaction of 60-70%, and 87.5% (14/16) had a level of improvement of (5)-(6) which correlated with a level of satisfaction of 50-60%.
A test for a difference in proportions (a Z-test) was used to examine effective rate. The Student’s t-test was used to examine efficacy. Both tests examined significant differences at a 5% level of significance (α error). Confidence intervals were set at 95%.
Informed consent for participation in this study was obtained verbally. Patient information was extracted from electronic medical records and included only treatment details and the patient’s initials to ensure that individuals could not be identified. The data were strictly managed and stored within the facility. Approval to conduct this study was obtained beforehand from the Institutional Review Board of the facility where the author works.
Results
Effective rate and efficacy in all patients are shown by formulation in table 1 for each of the 4 conditions asked about in the interview (had undergone bilateral oophorectomy/were receiving medication for pseudomenopause, being premenopausal, “cold in the lower body,” and being irritable). However, premenopausal patients excluded those who had undergone bilateral oophorectomy/those receiving medication for pseudomenopause. Among the 3 main formulations prescribed for hot flashes, the following formulations had a higher effective rate and efficacy for a given condition (asked about in the interview). In patients who had undergone bilateral oophorectomy/who were receiving medication for pseudomenopause, Keishi-bukuryo-gan had an effective rate of 90.0% and an efficacy of 86.1. In patients who were premenopausal, Toki-shakuyaku-san had an effective rate of 76.6% and an efficacy of 84.0. In patients with “cold in the lower body,” Keishi-bukuryo-gan had an effective rate of 76.3% and an efficacy of 81.2. In patients who were irritable, Kami-shoyo-san had an effective rate of 80.8% and an efficacy of 85.7. However, there was no significant difference in the effective rate and efficacy of pairs of formulations compared by a given condition (asked about in the interview). Similar results were obtained for effective rate as shown in the flow diagram in figure 1. In patients to whom none of the interview questions applied, Keishi-bukuryo-gan had higher effective rate. However, there was no significant difference in the effective rate of pairs of formulations compared by a given condition (asked about in the interview).
|
|
|
Bilateral oophorectomy |
Pre-menopause |
Cold in the lower body |
Irritable |
|
|
|
Pseudomenopause therapy |
|||
|
Tokishakuyaku-san |
Effective rate |
72.7%(16/22) |
76.6%(144/188) |
71.8%(56/78) |
67.5%(52/77) |
|
Efficacy |
80 |
84 |
80.9 |
80.7 |
|
|
Keishibukuryo-gan |
Effective rate |
90.0%(18/20) |
66.7%(84/126) |
76.3%(87/114) |
65.0%(39/60) |
|
Efficacy |
86.1 |
81.5 |
81.2 |
80 |
|
|
Kamishoyo-san |
Effective rate |
85.7%(6/7) |
66.3%(59/89) |
71.2%(37/52) |
80.8%(21/26) |
|
Efficacy |
78.3 |
81.9 |
73.9 |
85.7 |
|
|
|
|
|
|
|
|
|
Orengedoku-to |
Effective rate |
75.0(3/4) |
52.6%(10/19) |
46.2%(6/13) |
70.0%(7/10) |
|
Efficacy |
65 |
80.5 |
83.3 |
82.1 |
|
|
Nyoshin-san |
Effective rate |
57.1%(16/28) |
50.0%(6/12) |
72.7%(8/11) |
57.1%(4/7) |
|
Efficacy |
74.1 |
76.7 |
70.6 |
77 |
Table 1: Effective rate and efficacy by Kampo formulation in all patients with each of the 4 given conditions (asked about in the interview).
The effective rate and efficacy of Keishi-bukuryo-gan were compared depending on whether or not patients had undergone bilateral oophorectomy/they were receiving medication for pseudomenopause. These of Toki-shakuyaku-san were compared depending on whether or not patients were premenopausal. These of Keishi-bukuryo-gan were compared depending on whether or not patients had “cold in the lower body.” These of Kami-shoyo-san were compared depending on whether or not patients were irritable. The results are shown in table 2. A comparison of effective rate revealed significant differences depending on whether or not patients were premenopausal or irritable (P=0.0054, 0.016). A comparison of efficacy revealed significant differences depending on whether or not patients had undergone bilateral oophorectomy/they were receiving medication for pseudomenopause and whether or not they were irritable (P=0.018, 0.044).
|
|
|
Effective rate |
P(Z test) |
Efficacy |
P(t test) |
|
Keishibukuryo-gan |
Bilateral oophorectomy or Pseudomenopause therapy |
90.0%(18/20) |
0.074 |
86.1 |
0.018 |
|
not above |
71.5%(201/281) |
81.8 |
|||
|
Tokishakuyaku-san |
Pre-menopause |
76.6%(144/188) |
0.0054 |
84 |
0.072 |
|
Post-menopause |
63.1%(106/168) |
78.9 |
|||
|
Keishibukuryo-gan |
Cold in the lower body(+) |
76.3%(87/114) |
0.12 |
83.3 |
0.29 |
|
Cold in the lower body(-) |
67.7%(113/167) |
82.4 |
|||
|
Kamishoyo-san |
Irritable(+) |
78.3%(72/92) |
0.016 |
80.9 |
0.044 |
|
Irritable(-) |
60.6%(40/66) |
79.8 |
Table 2: A comparison of effectiveness depending on whether or not Kampo formulations were most efficacious/effective in treating each of the 4 given conditions asked about in the interview.
Oren-gedoku-to or Nyoshin-san was the fourth medication prescribed to patients who failed to respond to the 3 main formulations prescribed, and the effective rate and efficacy of these two formulations are shown in table 1. Oren-gedoku-to had a higher effective rate in patients who had undergone bilateral oophorectomy/who were receiving medication for pseudomenopause (75.0%) and in patients who were irritable (70.0%). Nyoshin-san had a higher effective rate in patients with “cold in the lower body” (72.7%).
The effective rate and efficacy of all 5 of the formulations used in this study are shown in table 3 by formulation, along with the average number of packets of an extract required to maintain the level of satisfaction among responders to each prescription. Among the 5 formulations prescribed, Toki-shakuyaku-san had the highest effective rate and highest efficacy, followed by Kami-shoyo-san, and then others. When the effective rate of pairs of formulations was compared, significant differences were noted only between Toki-shakuyaku-san and Keishi-bukuryo-gan (P=0.0038), Toki-shakuyaku-san and Oren-gedoku-to (P=0.007), and Kami-shoyo-san and Oren-gedoku-to (P=0.011). When the efficacy of pairs of formulations was compared, significant differences were noted only between Toki-shakuyaku-san and Nyoshin-san (P=0.007) and Toki-shakuyaku-san and Oren-gedoku-to (P=0.034). The average number of packets required to maintain the level of satisfaction among responders was rounded off, resulted in 4 packets per day for all formulations.
|
|
5 formulations in the all patients |
the average number of packets needed of an extract |
|
|
Tokishakuyaku-san |
Effective rate |
74.3%(281/378) |
3.68 |
|
Efficacy |
82 |
||
|
Keishibukuryo-gan |
Effective rate |
63.7%(179/281) |
3.73 |
|
Efficacy |
81.8 |
||
|
Kamishoyo-san |
Effective rate |
70.4%(112/159) |
3.65 |
|
Efficacy |
80.5 |
||
|
Orengedoku-to |
Effective rate |
50.0%(22/44) |
3.46 |
|
Efficacy |
76.4 |
||
|
Nyoshin-san |
Effective rate |
64.3%(18/28) |
3.72 |
|
Efficacy |
73.9 |
||
Table 3: Effective rate and efficacy of the 5 formulations for hot flashes prescribed in this study in all patients by formulation, and the average number of packets of an extract from Tsumura that is required to maintain the level of satisfaction in responders.
Discussion
When selecting an effective formulation from among the 3 main formulations prescribed for hot flashes based on the figure 1, tables 1-3, Keishi-bukuryo-gan is apparently a good first medication to prescribe for patients who had undergone bilateral oophorectomy/who were receiving medication for pseudomenopause. Toki-shakuyaku-san is apparently a good first medication to prescribe for premenopausal patients. Keishi-bukuryo-gan is a leading candidate as the first medication prescription for patients with “cold in the lower body”. Kami-shoyo-san is recommended as the first medication to prescribe for patients who were irritable. Previously, Toki-shakuyaku-san was selected as the first medication to prescribe for patients without “cold in the lower body” and who were not “irritable.” However, the current results indicated that the effective rate in Keishi-bukuryo-gan ranked highest for the patients who have no cold in the lower body and no irritability, so Keishi-bukuryo-gan should probably be the first medication chosen in that case. Toki-shakuyaku-san had a significantly higher efficacy in premenopausal patients than in postmenopausal patients, which can be explained by the fact that declining ovarian function and reduced E production as menopause approaches are considered to be causes of hot flashes, but Toki-shakuyaku-san is thought to limit the decline in E and to act to regulate hormones [26,27]. If patients failed to respond to the 3 main formulations prescribed in this study, a fourth medication was prescribed. However, there was a shift from Oren-gedoku-to to Nyoshin-san over the 13 years studied. A look at the results of this study over 12 years indicates that, as shown in Table 1, Oren-gedoku-to had a higher effective rate in patients who had undergone bilateral oophorectomy/who were receiving medication for pseudomenopause and in patients who were irritable while Nyoshin-san had a higher effective rate in patients with “cold in the lower body.” In patients who failed to respond to the 3 main formulations prescribed, results thus indicated that the improved protocol in figure 2 should be followed, with Oren-gedoku-to being selected for patients who had undergone bilateral oophorectomy/who were receiving medication for pseudomenopause or who presented with irritability and with Nyoshin-san being selected for those with “cold in the lower body.” In patients who had undergone bilateral oophorectomy/who were receiving medication for pseudomenopause, Keishi-bukuryo-gan should probably be selected as the first medication to prescribe and Oren-gedoku-to should probably be selected as the second medication to prescribe. The results of this study indicate that the medication selection protocol should be improved as shown in figure 2. By switching to the improved protocol in figure 2 and prescribing formulations based on it from now on may further improve the outcomes of Kampo treatment for hot flashes.
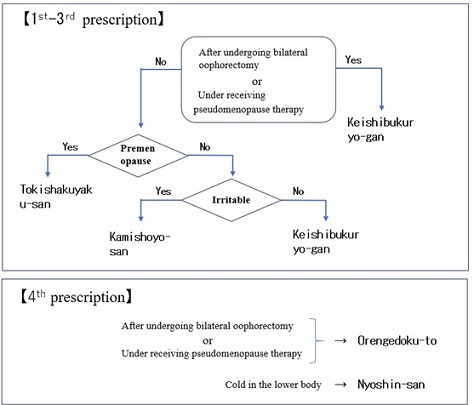
Figure 2: The improved protocol and flow diagram for selection of formulations for hot flashes
A total of 32 patients failed to respond by the fourth medication over a period of 12 years, so an average of 2.7 patients per years (32patients/12 years) failed to respond to Kampo treatment. Therefore, Kampo medicine using herbal formulations can be one of the non-hormonal treatments for hot flash.
Based on table 3, Toki-shakuyaku-san had the highest effective rate (over 74%) and the highest efficacy (80.0) overall of all the 5 formulations described in this study. Therefore, when one is having difficulty determining which formulation to prescribe, Toki-shakuyaku-san is thus likely to be efficacious.
That said, all 5 formulations of extracts from Tsumura needed to be prescribed in a dose of 4 packets per day in order to achieve a sufficient level of satisfaction. If, therefore, signs of the alleviation of hot flashes are noted with 3 packets per day (the standard dose for a Tsumura extract), then the dose should promptly be increased to 4 packets per day (divided into 2 doses). Having the divided into 2 also improves medication compliance.
In this study, Oren-gedoku-to and Nyoshin-san were prescribed less often than the 3 main formulations. Therefore, the medication selection protocol should be further improved by gaining experience prescribing other formulation such as Tsudo-san, Go-shaku-san and assembling more patients.
Conclusion
Based on the results of this study, an improved protocol (Figure 2) was devised as a way to allow the efficient selection of Kampo extracts that would be effective in treating hot flashes. The improved protocol that resulted can serve as a guideline for selecting formulations that are effective in treating hot flashes.
If a patient has undergone bilateral oophorectomy or is receiving pseudomenopause therapy, Keishi-bukuryo-gan should be prescribed. For other patients, Toki-shakuyaku-san should be prescribed for premenopausal patients, Kami-shoyo-san should be prescribed for postmenopausal patients who are irritable, and Keishi-bukuryo-gan should be prescribed for postmenopausal patients with cold in the lower body or none of these criteria apply. In case that the 3 main formulations were invalid, Oren-gedoku-to should be prescribed for patients who have undergone bilateral oophorectomy/who are receiving pseudomenopause therapy or who is irritable as the fourth medication. Nyoshin-san should be prescribed for those with cold in the lower body.
References
- Bansal R, Aggarwal N (2019) Menopausal Hot Flashes: A Concise Review. J Midlife Health 10: 6-13.
- Balakrishnan D, Garg R (2024) Emerging Trends in Treatment of Hot Flashes at Menopause: A Review. J South Asian Fede Obstet Gyn 16: 595-601.
- Madsen TE, Sobel T, Negash S, Shrout Allen T, Stefanick ML, et al. (2023). A Review of Hormone and Non-Hormonal Therapy Options for the Treatment of Menopause. Int J Womens Health 15: 825-836.
- Loprinzi CL, Stearns V, Barton D (2005) Centrally active nonhormonal hot flash therapies. The American Journal of medicine 118: 118-123.
- Oakley AE, Steiner RA, Chavkin C, Clifton DK, Ferrara LK, et al. (2016) KappaAgonists as a Novel Therapy for Menopausal Hot Flashes. Menopause 22: 1328-1334.
- Sahni S, Lobo-Romero A, Smith T (2021) Contemporary Non-hormonal Therapies for the Management of Vasomotor Symptoms Associated with Menopause: A Literature Review. Touch REVIEWS in Endocrinology 17: 133-137.
- Fait T (2019) Menopause hormone therapy: latest developments and clinical practice. Drugs Context 8: 212551.
- Morrow PK, Mattair DN, Hortobagyi GN (2011) Hot Flashes: A Review of Pathophysiology and Treatment Modalities. The Oncologist 16: 1658-1664.
- Scheid V (2006) Traditional Chinese medicine -What are we investigating? The case of menopause Complementary Therapies in Med 15: 54-68.
- Ushiroyama T (2013) The role of traditional Japanese medicine (Kampo) in the practice of psychosomatic medicine: the usefulness of Kampo in the treatment of the stress-related symptoms of women, especially those with peri-menopausal disorder. Biopsychosoc Med 7: 16.
- Terauchi M (2016) Menopausal symptoms and the Kampo medicine: Tokishakuyakusan, Kamishoyosan, and Keishibukuryogan. Sanfujinnka Kampo kennkyu no Ayumi No 33: 23-30.
- Yoshimura A, Sawada K, Sasano T, Kuroda H, Kozasa K, et al. (2017) Effect of Japanese Kampo Medicine Therapy for Menopausal Symptoms after Treatment of Gynecological Malignancy. Obset Gyn Int 9475919: 6.
- Takamatsu K, Ogawa M, Higuchi T, Takeda T, Hayashi K, et al. (2020). Effects of Kamishoyosan, a Tradishonal Japanese Medicine, on Menopausal Symptoms: A Randomised, Placebo-Controlled, Double-Blind Clinical Trial. Evid Based Complement Alternat Med 2020: 9285317.
- Takamatsu K, Ogawa M, Obayashi S, Takeda T, Terauchi M, et al. (2021). A Multicenter, Randomized, Double-Blind, Placebo-Controlled Trial to Investigate the Effects of Kamishoyosan, a Traditional Japanese Medicine, on Menopausal Symptoms: The KOSMOS Study. Evid Based Complement Alternat Med 2021: 8856149.
- Shigehara K, Izumi K, Nakashima K, Kawaguchi S, Nohara T, et al. (2023). Efficacy of Keishibukuryogan for hot flashes in prostate cancer patients receiving androgen deprivation therapy: a sub-analysis focusing on hormonal and cytokine levels. Transl Androl Urol 12: 1273-1282.
- Plotnikoff GA, Watanabe K, Torkelson C, Valleur JL, Radosevich DM (2011). The TU-025 Keishibukuryogan for Hot Flash Management in Postmenopausal Women: Results and Lessons for Future Research. Menopause 18: 886-892.
- Hayashi S, Shibutani S, Okubo H, Shimogawara T, Ichinose T, et al. (2014) Examination of Clinical Efficacy of Keishibukuryogan on Non-Specific Complaints Associated with Varicose Veins of the Lower Extremity. Ann Vasc Dis 7: 266-273.
- Shigehara K, Izumi K, Nakashima K, Kawaguchi S, Nohara T, et al. (2020). Efficacy and safety of keishibukuryogan, a traditional Japanese Kampo medicine, for hot flashes in prostate cancer patients receiving androgen deprivation therapy. Transl Androl Urol 9: 2533-2540.
- Satomi H, Mori Y, Makino B, Nakai Y, Takeda S, et al. (2010) Clustering Analysis of Keishibukuryogan Formulas by Use of Self-Organizing Maps. Chem Pharm Bull 58: 1497-1501.
- Liu Y, Kobayashi S, Wang L, Ren Y, Song P (2025) Kampo medicine in the management of menopausal symptoms: A narrative review of therapeutic potential. Drug Discoveries Therapeutics 19: 136-147.
- Kubota S, Yamamoto Y, Kimura K (2022) A Chinese Medicine, Tokishakuyakusan, Increase Bovine Oviductal Tonus via G Protein-Coupled Estrogen Receptor 1. Biol Pharma Bull 45: 1133-1141.
- Itoh T, Senda S, Inoue H, Saitoh Y, Kagami M, et al. (2006). Clinical effect of orengedokuto for patients with climacteric disorder-Comparison with symptoms in kamishoyosan-responders-. J Traditional Med 23: 37-41.
- Revicki DA (2004). Patient assessment of treatment satisfaction: methods and practical issues. Gut 53: 40-44.
- Desta H, Berhe T, Hintsa S (2018). Assessment of patients’ satisfaction and associated factors among outpatients received mental health services at public hospitals of Mekelle Town, northern Ethiopia. Int J Ment Health Syst 12: 1-7.
- Isobe T (2023) Comparison of Effectiveness of Acupuncture at Different Patterns of Fixed Points by Only Tapping Technique. J Altern Complement Integr Med 9: 1-8.
- Noda T, Shiga H, Yamada K, Harita M, Nakamura Y, et al. (2019). Effects of Tokishakuyakusan on Regeneration of Murine Olfactory Neurons In Vivo and In Vitro. Chemical Senses 44 : 327-338.
- Toriizuka K, Hou P, Yabe T, Iijima K, Hanawa T, et al. (2000) Effects of Kampo medicine, Toki-shakuyaku-san, on choline acetyltransfetase activity and norepinephrine contents in brain regions, and mitogenic activity of splenic lymphocytes in ovariectomized mice. J Ethnopharma 71: 133-143.
Citation: Isobe T, Kaijima M, Kaijima H (2025) How to Select Herbal Formulations that are Effective in Treating Hot Flashes: A Retrospective Study over 12 Years. HSOA J Altern Complement Integr Med 11: 638.
Copyright: © 2025 Tetsuya Isobe, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

