Hypokalemia-Induced Ventricular Tachycardia in a Patient with Anorexia Nervosa: A Case Report
*Corresponding Author(s):
Yu-Wei FangDivision Of Nephrology, Department Of Internal Medicine, Shin Kong Wu Ho Se Memorial Hospital, Taipei, Taiwan
Tel:+886 228332211,
Email:m005916@gmail.com
Abstract
Introduction: Sudden death is the main cause of mortality in patients with anorexia nervosa. Contribution form Life-threatening arrhythmia was highly suspected. Herein, we describe the case of a 20-year-old female who presented to the emergency department with general weakness and vertigo followed by sudden change in consciousness and syncope. Electrocardiogram revealed ventricular tachycardia, which progressed to asystole. Immediate cardiopulmonary and cerebral resuscitation and electrical defibrillation were initiated. Laboratory data showed severe hypokalemia (1.7mmol/l) with metabolic alkalosis. Aggressive potassium chloride supplementation reversed her cardiac rhythm to sinus. Her clinical features and subsequent laboratory findings were consistent with anorexia nervosa.
Conclusion: Therefore, it is noteworthy that hypokalemia due to anorexia nervosa is potentially life threatening; regular maintenance of normal serum potassium levels is important in such settings.
Keywords
Anorexia nervosa; Arrhythmia; Cardiac arrest; Hypokalemia; Paralysis
Abbreviations
AN = Anorexia Nervosa
ED = Emergency Department
BMI = Body Mass Index
CPCR = Cardiopulmonary Cerebral Resuscitation
K+ = Potassium
TTKG = Transtubular Potassium Gradient
UK+/Cr = Urine Potassium-Creatinine Ratio
KCl = Potassium Chloride
Introduction
Anorexia Nervosa (AN) is a type of eating disorder in which patients usually present with extracellular volume depletion and disturbances in acid–base and electrolyte balance, including metabolic alkalosis, hypokalemia, hypophosphatemia, and hyperreninemic hyperaldosteronism [1]. Among these presenting symptoms, hypokalemia is the most common and may be due to potassium deficiency from diet restriction, repeated vomiting, and excessive renal loss. In patients with AN, studies have shown an estimated hypokalemia prevalence of 19%-20% [2].
The most life-threatening conditions resulting from hypokalemia are cardiac arrhythmia and respiratory insufficiency [3]. Prompt diagnosis and appropriate management are necessary to minimize hypokalemia-associated mortality. Most commonly, patients suffering from AN seek medical help at the Emergency Department (ED) due to complications of hypokalemia, such as hypokalemic paralysis. We present a rare case of a patient with AN who presented with life-threatening ventricular tachycardia.
Case Report
A 20-year-old Chinese woman was brought to the ED due to generalized weakness for the entire day. Associated symptoms were intermittent vertigo and tinnitus, as well as one episode of vomiting. She was not taking any medications, including laxative or diuretics, and denied alcohol or drug use. Her family and past medical histories were unremarkable. On physical examination, her blood pressure was 120/70mm Hg, heart rate was 70 beats/min, respiratory rate was 20 beats/min, and body temperature was 36.7°C. Her body weight was 36kg and she was 1.55m tall, with a Body Mass Index 14.9 (BMI) of kg/m2. Other physical examination findings were unremarkable.
At the ED, the patient suddenly lost consciousness and collapsed. An electrocardiogram revealed ventricular tachycardia, which progressed to asystole (Figure 1a). Immediate advanced cardiac life support was performed for resuscitation, and return of spontaneous circulation was achieved after 8 min of Cardiopulmonary Cerebral Resuscitation (CPCR) and electrical defibrillation (Figure 1b). Arterial blood gas analysis revealed metabolic alkalosis and severe hypokalemia of 1.7mmol/L (reference 3.5-5.0mmol/l); the other biochemical data are shown in table 1. Further evaluation of urine potassium (K+) excretion revealed inconsistent results, such as low urine K+ to urine creatinine ratio (UK+/Cr, 0.29mmol/mmol; reference: 1.5-2.0mmol/mmol) and high transtubular K+ gradient (TTKG, 3.60; reference: >3). Her serum magnesium concentration was 0.9mmol/l (reference: 0.7-1.1mmol/l). Aggressive Potassium Chloride (KCl) replacement therapy was given for hypokalemia. Her heart rhythm was restored to sinus rhythm when plasma K+ concentration reached 2.5mmol/l. KCl supplementation (250mEq) increased serum K+ to 3.7mmol/l. There were no structural abnormalities on echocardiography.
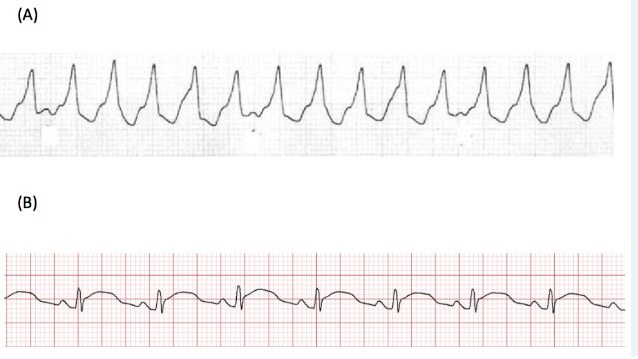 Figure 1: Electrocardiogram of the patient in this case. (a): Tracing after syncope shows ventricular tachycardia, with regular heart beats and widening of the QRS complex; (b): After resuscitation, cardiac rhythm is restored to sinus but with PT interval prolongation and mild QRS complex widening.
Figure 1: Electrocardiogram of the patient in this case. (a): Tracing after syncope shows ventricular tachycardia, with regular heart beats and widening of the QRS complex; (b): After resuscitation, cardiac rhythm is restored to sinus but with PT interval prolongation and mild QRS complex widening.
|
|
Reference Range |
Values |
|
Plasma |
|
|
|
PH |
7.38-7.42 |
7.46 |
|
HCO3−, mmol/l |
23-25 |
34.5a |
|
Na+, mmol/l |
135-142 |
137 |
|
K+, mmol/l |
3.5-5.0 |
1.7a |
|
Cl− , mmol/l |
96-108 |
91 |
|
Phosphate, mmol/l |
0.8-1.6 |
1.4 |
|
Calcium, mmol/l |
2.15-2.58 |
2.3 |
|
Magnesium, mmol/l |
0.7-1.1 |
0.9 |
|
Blood urea nitrogen, mmol/l |
2.9-8.9 |
2.5 |
|
Creatinine, μmol/l |
60-130 |
53.38 |
|
Osmolality, mosm/kgH2O |
278-305 |
279 |
|
Urine |
|
|
|
Na+, mmol/l |
|
13 |
|
K+, mmol/l |
|
12 |
|
Cl−, mmol/l |
|
13 |
|
Calcium, mmol/l |
|
1 |
|
Phosphate, mmol/l |
|
5.26 |
|
Creatinine, μmol/l |
|
40522 |
|
Osmolality, mosm/kg.H2O |
|
547 |
|
Ca2+/Cr, mmol/mmol |
0.1-0.25 |
0.02 |
|
K+/Cr, mmol/mmol |
<1.5 |
0.29 |
|
TTKG |
<3 |
3.60 |
Table 1: Baseline biochemical values on admission.
Note: Abbreviation: TTKG: Transtubular K+ Gradient; a Indicates abnormal values.
Tracing back her history, she suffered from eating disorder with recurrent vomiting due to fear of being overweight. The overall clinical profile of this patient was compatible with a diagnosis of renal involvement of AN, including metabolic alkalosis and hypokalemia from renal wasting. She was then treated with oral KCL (600mg, 8mEq K+) thrice daily. There was no recurrent arrhythmia thereafter during hospitalization. However, she lost to follow up after discharge.
Discussion
This patient experienced life-threatening ventricular tachycardia due to severe hypokalemia. According to the flow chart of approaching a patient with hypokalemia [4-8] (Figure 2), a remote gastrointestinal problem with volume contraction was highly suspected due to the high urine K+ secretion, metabolic alkalosis, normal blood pressure, and low urine sodium and chloride levels; for the measurement of K+ secretion, TTKG was more reliable in our case because the urine creatine level was too high, presumably related to muscle injury after CPCR.
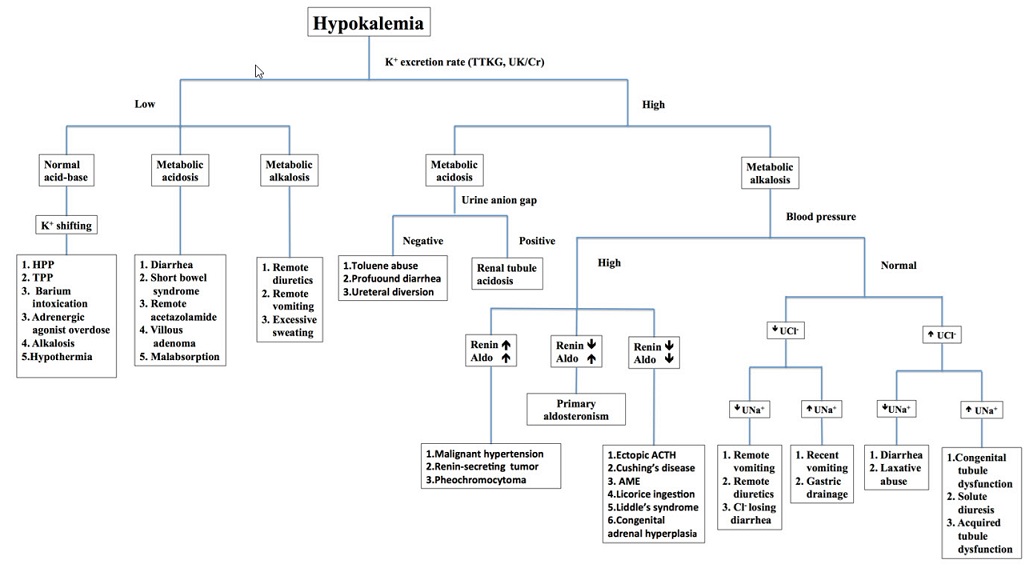 Figure 2: Approach to the diagnosis of hypokalemia [4-8].
Figure 2: Approach to the diagnosis of hypokalemia [4-8].
Note: Abbreviation: HPP: Hypokalemic Periodic Paralysis; TPP: Thyrotoxic Periodic Paralysis; UCl-: Urine Chloride; UNa+: Urine Sodium; Aldo: Aldosterone; ACTH: Adrenocorticotropic Hormone; AME: Apparent Mineralocorticoid Excess Syndrome.
Indeed, upon further questioning, the patient was discovered to suffer from AN, an increasingly prevalent psychiatric disease that is characterized by self-enforced starvation and vomiting to maintain body weight [9]. This may result in severe reduction of body mass and disturbances in body fluid homeostasis. Restricted diet and episodic vomiting may induce sodium and volume depletion and hypokalemia. Subsequent activation of the renin–angiotensin–aldosterone system in response to volume depletion aggravates renal wasting related to hypokalemia with metabolic alkalosis. In addition, hypokalemia increases ammonium production and promotes bicarbonate reabsorption to maintain alkalosis [10]. Furthermore, chronic hypokalemia can cause renal parenchymal changes, including epithelial vacuolization, glomerulosclerosis, interstitial nephritis, tubular atrophy, and cystic formation [11]. Several studies have reported that over 50% of patients with AN do not recover completely; AN is associated with an overall mortality rate of 5%-10% within 10 years [12] and leads to chronic illness in more than 20% cases [13].
In a cardiomyocyte, hypokalemia can cause the negative resting membrane potential to hyperpolarize the cell membrane. Ventricular repolarization can be delayed and cause typical changes in electrocardiogram, including T wave inversion, ST segment depression, and appearance of U waves. When K+ depletion is severe, PR interval prolongation and QRS complex widening may be observed, leading to an increased risk of ventricular arrhythmia, particularly in patients with pre-existing cardiac disease. Ewan et al. had reported an AN patient presenting with cardiac arrest due to hypokalemia [14]. However, the provided laboratory data in this case for hypokalemia approaching was insufficient compared to our case. In patients with AN, long-term weight loss may cause structural and functional changes in the heart. Cardiac examinations, such as echocardiography, treadmill exercise test, and electrocardiography, have been previously evaluated in patients with AN [15]. In all these patients with AN, the influence of hypokalemia on cardiac rhythm and function could be excluded because serum electrolytes were normal. In this study, cardiac parameters, including left ventricular end-diastolic dimension, left ventricular wall thickness, and aortic root dimension, were all below the normal mean values for a healthy adult. After weight gain, these parameters increased significantly; 24-h electrocardiographic monitoring detected ventricular ectopic beats and short runs of ventricular tachycardia on exercise. In addition, the OT interval was noted to be longer in patients with AN but was reversible after refeeding [16]. These findings suggest that patients with AN may be prone to cardiac arrhythmias, independent of serum K+ levels. Therefore, further reductions in serum K+ may aggravate this predisposition and contribute to life-threatening conditions, as seen in our patient.
In a medical emergency secondary to profound hypokalemia, immediate and adequate correction to raise serum K+ to a safe range (approximately 3.0mmol/l) is crucial; total body K+ deficit can be replaced slowly thereafter [17]. It should be noted that high concentrations of K+ at a rapid infusion rate can be safely given only via a central venous catheter with cardiac monitoring. In addition, infusion of fluids with glucose or bicarbonate may redistribute K+ from the extracellular to the intracellular fluid space, which may aggravate hypokalemia and delay the rate of correction [18]. These should be avoided in a medical emergency.
Conclusion
Our case illustrated the importance of maintaining normal serum K+ levels when managing patients with AN, because their cardiac function is vulnerable to arrhythmias. Prompt diagnosis and aggressive correction to restore normal serum K+ levels are crucial and life-saving in this condition.
Acknowledgement
We thank our patient for contributing clinical data to this report.
Ethical Statement
Ethical approval was not necessary for this study as our study was focused on the retrospective observation of a patient’s hospital course, which did in no way to affect his treatment. Informed Consent was not obtained from the patient because she lost to follow-up after discharge.
Conflict of Interest
All authors of this manuscript have no financial or personal relationships to disclose.
References
- Leaf DE, Bukberg PR, Goldfarb DS (2012) Laxative abuse, eating disorders, and kidney stones: A case report and review of the literature. Am J Kidney Dis 60: 295-298.
- Miller KK, Grinspoon SK, Ciampa J, Hier J, Herzog D, et al. (2005) Medical findings in outpatients with anorexia nervosa. Arch Intern Med 165: 561-566.
- Kunin AS, Surawicz B, Sims EA (1962) Decrease in serum potassium concentrations and appearance of cardiac arrhythmias during infusion of potassium with glucose in potassium-depleted patients. N Engl J Med 266: 228-233.
- Tsai MH, Lin SH, Leu JG, Fang YW (2015) Hypokalemic paralysis complicated by concurrent hyperthyroidism and chronic alcoholism: A case report. Medicine (Baltimore) 94: 1689.
- Lin SH, Chiu JS, Hsu CW, Chau T (2003) A simple and rapid approach to hypokalemic paralysis. Am J Emerg Med 21: 487-491.
- Chiang WF, Hsu YJ, Chang CC, Lin SH (2012) Hypokalemic paralysis in a young obese female. Clin Chim Acta 413: 1295-1297.
- Sung CC, Cheng CJ, Chiang WF, Chau T, Hsu YJ, et al. (2015) Etiologic and therapeutic analysis in patients with hypokalemic nonperiodic paralysis. Am J Med 128: 289-296.
- Lin SH, Lin YF, Chen DT, Chu P, Hsu CW, et al. (2004) Laboratory tests to determine the cause of hypokalemia and paralysis. Arch Intern Med 164: 1561-1566.
- Hay PJ, Mond J, Buttner P, Darby A (2008) Eating disorder behaviors are increasing: Findings from two sequential community surveys in South Australia. PLoS One 3: 1541.
- Mars DR, Anderson NH, Riggall FC (1982) Anorexia nervosa: A disorder with severe acid-base derangements. South Med J 75: 1038-1042.
- Luthra M, Davids MR, Shafiee MA, Halperin ML (2004) Anorexia nervosa and chronic renal insufficiency: A prescription for disaster. QJM 97: 167-178.
- Garcia CS (2002) Binge eating disorders and obesity. Nutr Hosp 17: 55-59.
- Treasure J, Claudino AM, Zucker N (2010) Eating disorders. Lancet 375: 583-593.
- Ewan SL, Moynihan PC (2013) Cardiac arrest: First presentation of anorexia nervosa. BMJ Case Rep 2013: 2013200876.
- Gottdiener JS, Gross HA, Henry WL, Borer JS, Ebert MH (1978) Effects of self-induced starvation on cardiac size and function in anorexia nervosa. Circulation 58: 425-433.
- Cooke RA, Chambers JB, Singh R, Todd GJ, Smeeton NC, et al. (1994) QT interval in anorexia nervosa. Br Heart J 72: 69-73.
- Lin SH, Halperin ML (2007) Hypokalemia: A practical approach to diagnosis and its genetic basis. Curr Med Chem 14: 1551-1565.
- Cohn JN, Kowey PR, Whelton PK, Prisant LM (2000) New guidelines for potassium replacement in clinical practice: A contemporary review by the national council on potassium in clinical practice. Arch Intern Med 160: 2429-2436.
Citation: Hsu JH, Tsai MH, Fang YW (2021) Hypokalemia-Induced Ventricular Tachycardia in a Patient with Anorexia Nervosa: A Case Report. J Nephrol Renal Ther 7: 064.
Copyright: © 2021 Jung-Hui Hsu, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.