
Hyponatremia: It’s in the Eye of the Beholder: Pitfalls in the Diagnosis and Treatment of SIADH with Desalination due to Herpes Zoster Ophthalmicus (HZO)
*Corresponding Author(s):
Richard N HellmanDepartment Of Medicine, Division Of Nephrology And Hypertension, Indiana University School Of Medicine, Indiana, United States
Tel:+1 3174406641,
Email:rhellman@iupui.edu
Abstract
Herpes Zoster Ophthalmicus (HZO) is a rare cause of SIADH (Syndrome of Inappropriate Anti-Diuretic Hormone secretion). It occurs when herpesvirus type 3 activation presents in the first division, or ophthalmic division of the trigeminal nerve. We describe an elderly women hospitalized with right eye pain and swelling, headache, scalp tenderness, and hypertensive urgency who initially was felt to have Giant Cell Arteritis (GCA) treated with corticosteroids. She was subsequently found to have HZO and developed symptomatic hyponatremia due to SIADH after infusion with isotonic saline. Treatment of hyponatremia and acyclovir led to normalization of serum sodium, mental status and blood pressure. Diagnosis and treatment of hyponatremia in SIADH are discussed with particular emphasis on the pitfall of desalinization in the estimation of hyponatremia correction.
Abbreviations
GCA: Giant Cell Arteritis
HZO: Herpes Zoster Opthalmicus
SIADH: Syndrome of Inappropriate Anti-Diuretic Hormone
Introduction
Syndrome of Inappropriate Anti Diuretic Hormone (SIADH) secretion is the most common cause of euvolemic hyponatremia and can be a result of a variety of etiologies including medications, pain, nausea, anesthesia, malignancies, pulmonary disorders, and central nervous system disorders [1-5]. Generally urine osmolarity (Uosm) is taken as a measure of ADH levels and activity however co-peptin levels which are a by-product of the vasopressin prohormone breakdown can also be used as an indirect measurement of vasopressin levels [6-10]. Cases of SIADH with high Uosm levels can also be seen with the phenomenon of desalination where expansion with an isotonic solution results in net electrolyte free water gain [11,12]. Here we present a case of HZO as a cause of SIADH with accompanying desalination phenomena and pertinent calculations highlighting hyponatremia correction issues with desalination.
Case Report
An 85 year old female was admitted to the hospital with a 2 day history of worsening right eye pain associated with a headache, scalp tenderness, hypertensive urgency without a prior history of hypertension, and a presumptive diagnosis of Giant Cell Arteritis (GCA). She had been started on high dose prednisone in the ER prior to admission. She had a past medical history of keratoconjunctivitis sicca, osteoarthritis, central retinal vein occlusion of the left eye and a sternal fracture post motor vehicle accident in 2019. There was a surgical history of hysterectomy. She lived at home with her husband, daughter and grandchildren. She was a life-time non-smoker and had no alcohol or recreational drug use. History was negative for recent travel and she had no ill contacts exposure. Family history was negative for kidney disease.
Initial labs on admission showed a serum sodium (Na) of 131 mmol/L, with prior normo-natremia, a serum creatinine of 0.42 mg/dL, potassium 4.4 mmol/L, chloride of 97 mmol/L a bicarbonate of 25 mmol/L, a blood glucose of 118 mg/dL and a low serum uric acid of 2.2 mg/dL. Complete blood count showed normal indices. Inflammatory markers were elevated with ESR of 75 mm/hr and C reactive protein of 3 mg/dL. Hypertensive urgency was treated with labetalol and amlodipine, while the pain was managed with opioids.
Over the course of the next 36 hours she developed somnolence and reduced oral intake. She was given a normal saline bolus and normal saline infusion. This resulted in a consistent drop in her serum sodium acutely to 116 mmol/L and a nephrology consultation was requested (Figure 1). There was no evidence of cerebral salt wasting.
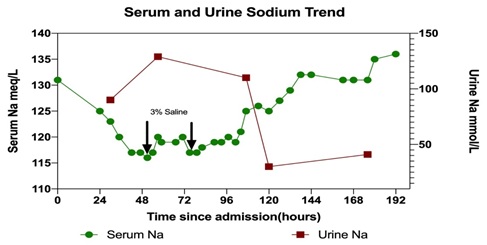 Figure 1: Serum and urine sodium are plotted over time. Arrows indicate initial normal saline administration and 3% saline administration. Note a fall in serum sodium and increase in urinary sodium (desalination) after NS. Serum sodium normalizes at 8 days and is associated with a fall in urine sodium.
Figure 1: Serum and urine sodium are plotted over time. Arrows indicate initial normal saline administration and 3% saline administration. Note a fall in serum sodium and increase in urinary sodium (desalination) after NS. Serum sodium normalizes at 8 days and is associated with a fall in urine sodium.
Nephrology evaluation showed a confused and obtunded elderly lady with right periocular pain. Additional history was obtained from family. Examination revealed moist mucous membranes, and no edema consistent with euvolemia. Serum and urinary labs showed serum osmolality of 265 mosm/kg, urine osmolality of 626 mosm/L and Urine Na 130 mEq/L (Figure 2).
 Figure 2: The use of calculations based on the simplified Edelman formula: [Na+]=(eNa++eK+)/TBW clinically simplified as Serum [Na+]=Total Body (Na+ + K+)/ TBW can help in estimating serum sodium as a result of therapy. Addition or subtraction of solute from the numerator or volume from the denominator in this equation can estimate changes in [Na+] as a result of therapy. For clinical calculation TBK+ is omitted from the equation. Examples are given at 24-48 hours with calculations showing how NS can be associated with worsening hyponatremia and at 72-96 plus hours when increased solute, water restriction and furosemide help predict the results of therapy by accounting for desalination.
Figure 2: The use of calculations based on the simplified Edelman formula: [Na+]=(eNa++eK+)/TBW clinically simplified as Serum [Na+]=Total Body (Na+ + K+)/ TBW can help in estimating serum sodium as a result of therapy. Addition or subtraction of solute from the numerator or volume from the denominator in this equation can estimate changes in [Na+] as a result of therapy. For clinical calculation TBK+ is omitted from the equation. Examples are given at 24-48 hours with calculations showing how NS can be associated with worsening hyponatremia and at 72-96 plus hours when increased solute, water restriction and furosemide help predict the results of therapy by accounting for desalination.
A diagnosis of SIADH with desalination was made as she fulfilled the diagnostic criteria for SIADH [6-8]. Due to the acute change in serum sodium corresponding with a change in mentation, she was given 3% hypertonic saline [9,10,12]. This was in addition to free water restriction, and furosemide. SerumNa improved to 120 mmol/L with 3% hypertonic saline however it dropped again the next day to 117 mmol/L requiring repeated doses of 3% Saline. Once mentation improved salt tablets were added to increase solute intake. Daily urine osmolality continued to decrease to 500s mosm/L and later to 360 mosm/L as did urinary sodium 48 hours after these interventions. (Figure 1). A serum Copeptin pro-AVP (arginine vasopressin) was 34.8 pmol/L (H) with a serum Na of 125 mEq/L consistent with SIADH. The only prior measurement of plasma vasopressin by Kucukardali with a patient with SIADH due to HZO was increased at 40 pg/mL [3].
On follow up clinical exam peri-ocular swelling and a herpes zoster rash appeared 48 hours later. PCR was positive for varicella-zoster virus. Acyclovir was started and corticosteroids stopped. Additional findings were an e. coli urinary tract infection treated with Augmentin, and mild hyperthyroidism felt due to iodinated contrast and a multinodular goiter. A chest X-ray was normal and an MRI of the head revealed right periorbital edema and inflammation and CNS microvascular disease with no cerebral edema. Over the following 5 days the hyponatremia resolved with HZO treatment. Hypertension resolved and the patient’s mental status normalized.
Six months post HZO the patient’s SIADH and hypertension have resolved, and she has residual Post Herpetic Neuralgia (PHN).
Discussion
HZO represents 10-20% of Herpes Zoster (HZ) cases. Localized herpes zoster is a rare cause of SIADH and that due to HZO is even more unusual. The trigeminal nerve branches are ophthalmic, maxillary and mandibular [2,4]. SIADH with HZO is thought to be due to dysregulation of stimulating signals from nucleus tractus solitarious to the supraoptic and paraventricular nuclei in the brainstem leading to increased ADH release [5]. Pain, opioids, and other medications, e.g. acyclovir, carbamazepine, may also cause SIADH.
Localized HZ with SIADH has been reported in 16 cases to date including our case of which 7/16 (44%) involved the trigeminal nerve with HZO, 11/16 (69%) were female, 5/16 (31%) had PHN, average age was 75 years and 2/16 (8%) died. Hyponatremia was severe 112.2 mEq/L in all localized HZ cases and 114.2 mEq/L in HZO [1-3,5,11]. In our case the presence of an elevated Copeptin level with hyponatremia suggests classic SIADH with the release of ADH. Hyponatremia correction in HZO takes an average of 7 days although SIADH of 4 months has been reported in a case series [6]. Additionally in some cases the persistence of PHN has been associated with delayed resolution of SIADH which was not apparent in our case as PHN persisted despite the resolution of hyponatremia and SIADH [5].
Desalination needs to be considered in the correction of hyponatremia in SIADH as commonly used hyponatremia treatment formulas assume only water excess as hyponatremia etiology (Figure 2). If high urinary sodium losses are not recognized inadequate correction of hyponatremia may occur. In our case the use of normal saline was associated with an actual fall in serum sodium due to the desalination phenomena. Steele noted a fall in serum sodium of about 4 mmol/L after infusion of 2-3 Liters of isotonic sodium chloride (154 mmol/L) or Ringers Lactate (130 mmol/L) in 22 women undergoing uncomplicated gynecologic surgery. This was due to the generation of electrolyte-free water during the excretion of hypertonic urine or a desalination process [9]. Musch and Decaux studying 17 asymptomatic patients with SIADH who received isotonic saline found only 6/17 had worsening hyponatremia and these patients had a urine osmolality Uosm of >530 mosm/kg [13].
The use of calculations based on the simplified Edelman formula: [Na+]=(eNa++eK+)/ TBW clinically simplified as Serum [Na+]=Total Body (Na+ + K+)/ TBW can help in estimating more accurate therapy [6,8,10]. Addition or subtraction of solute from the numerator or volume from the denominator in this equation can estimate changes in [Na+] as a result of therapy (Figure 2). Despite these estimates there is no substitute for careful and frequent laboratory monitoring in the correction of hyponatremia especially when it is severe to assure an appropriate serum sodium correction rate (6-8 mEq/24 hr.) and avoid delayed or overshoot correction [6-8,10,12].
General measures of water restriction, increased solute (NaCl or urea), hypertonic saline in symptomatic patients, use of furosemide to initiate a more hypotonic urine, frequent monitoring of electrolytes, fluid in & out measurement, and vaptans such as tolvaptan may be indicated in selected cases of chronic hyponatremia. More specifically in HZO the use of antiviral agents and potential prevention of HZO in patients with zoster vaccine is indicated.
Conclusion
HZO is a rare cause of hyponatremia due to SIADH. SIADH may be associated with desalinization. The worsening of hyponatremia with isotonic saline occurs more commonly in patients with Uosm >530 mosm/kg due to desalinization. Hyponatremia correction formulas assume pure water excess in SIADH, and desalinization needs to be recognized for appropriate estimation of serum sodium correction.
Acknowledgement
Dr. Michael Peregrim MD (Assistant Professor of Clinical Medicine, Indiana University School of Medicine), for consultation referral regarding this case.
References
- Bassi V, Fattoruso O, Santinelli C (2017) Localized herpes zoster infection: A rare cause of syndrome of inappropriate secretion of antidiuretic hormone. Oxf Med Case Reports 11: 065.
- Cruccu G, Di Stefano G, Truini A (2020) Trigeminal neuralgia. N Engl J Med 383: 754-762.
- Kucukardali Y, Solmazgul E, Terekeci H, Oncul O, Turhan V (2008) Herpes zoster ophthalmicus and syndrome of inappropriate antidiuretic hormone secretion. Intern Med 47: 463-465.
- Vrcek I, Choudhury E, Durairaj V (2017) Herpes Zoster Ophthalmicus: A Review for the Internist. Am J Med 130: 21-26.
- Wang CC, Shiang JC, Chen JT, Lin SH (2011) Syndrome of inappropriate secretion of antidiuretic hormone associated with localized herpes zoster ophthalmicus. J Gen Intern Med 26: 216-220.
- Ellison DH, Berl T (2007) Clinical practice. The syndrome of inappropriate antidiuresis. N Engl J Med 356: 2064-2072.
- Hoorn EJ, Zietse R (2017) Diagnosis and treatment of hyponatremia: Compilation of the guidelines. J Am Soc Nephrol 28: 1340-1349.
- Seay NW, Lehrich RW, Greenberg A (2020) Diagnosis and management of disorders of body tonicity-hyponatremia and hypernatremia: Core curriculum 2020. Am J Kidney Dis 75: 272-286.
- Steele A, Gowrishankar M, Abrahamson S, Mazer CD, Feldman RD, et al. (1997) Postoperative hyponatremia despite near-isotonic saline infusion: A phenomenon of desalination. Ann Intern Med 126: 20-25.
- Sterns RH (2014) Disorders of plasma sodium - causes, consequences, and correction. N Engl J Med 372: 55-65.
- Foppiani L (2018) SIADH with severe hyponatremia in an elderly man with herpes zoster infection: A Causal or casual association? Intern Med 57: 3393-3398.
- Sterns RH (2018) Treatment of severe hyponatremia. Clin J Am Soc Nephrol 13: 641-649.
- Musch W, Decaux G (1998) Treating the syndrome of inappropriate ADH secretion with isotonic saline. QJM 91: 749-753.
Citation: Jan MY, Hellman RN (2021) Hyponatremia: It’s in the Eye of the Beholder: Pitfalls in the Diagnosis and Treatment of SIADH with Desalination due to Herpes Zoster Ophthalmicus (HZO). J Nephrol Renal Ther 7: 054.
Copyright: © 2021 Muhammad Yahya Jan, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

