
Idiopathic Portal Hypertension in a Celiac Disease Patient: A Rare Association
*Corresponding Author(s):
Yeshaswini ReddyInternal Medicine Department, University Of Illinois College Of Medicine, Peoria, IL, United States
Tel:3093970821,
Email:psyeshaswini@gmail.com
Abstract
Idiopathic portal hypertension (IPH) is a disorder of unknown etiology and is associated with Celiac disease (CD). A literature review yielded only 11 reported cases making this a rare entity. We present an asymptomatic 39 year old male found to have IPH with persistently elevated liver enzyme for several years. His liver biopsy was consistent with IPH; duodenal biopsies showed intraepithelial lymphocytosis and villous blunting confirming the diagnosis of CD. Initiation of a gluten free diet (GFD) resulted in significant improvement in the liver function panel and resolution of varices on surveillance exams.
Keywords
Celiac disease; Cirrhosis; Gluten free diet; Idiopathic portal hypertension
Abbreviations
AMA: Antimitochondrial antibody; ANA: Antinuclear antibody; ASMA: Anti smooth muscle antibody; CD: Celiac Disease; CMV: Cytomegalovirus; EBV: Epstein Barr Virus; EGD: Esophagogastroduodenoscopy; GFD: Gluten Free Diet; HIV: Human Immunodeficiency Virus; INF: Interferon; IPH: Idiopathic Portal Hypertension; MRI: Magnetic resonance imaging
Introduction
IPH can be referred to as non cirrhotic portal hypertension without a known etiology and can manifest with splenomegaly, ascites, pancytopenia, and esophageal varices [1-3]. Liver involvement in IPH entails a wide array of non specific features ranging from either minimal change, dilatation of the sinusoids, phlebosclerosis, portal fibrosis, or nodular regenerative hyperplasia [4]. Celiac disease (CD) also known as autoimmune gluten sensitive enteropathy is a hereditary malabsorption gastrointestinal disorder [5-7,2]. This is a systemic disease and can also manifest with a variety of extraintestinal features [5,7,8]. Liver involvement has been noticed in CD patients and can present with asymptomatic elevation of transaminases, hepatitis, or cirrhosis [5,7-9]. The exact pathophysiology for IPH is unknown, but some theories suggest it is due to obliteration of the portal venous microcirculation leading to liver injury [1,2,10]. Early recognition and initiation of GFD is recommended to prevent further progression of liver dysfunction [9,10].
Case Presentation
We report a 39 year old white man with no significant past medical history that was referred to our facility for evaluation of chronic transaminitis. He was asymptomatic, without any alcohol/drug use, or family history of liver diseases. Physical exam was grossly unremarkable. Initial workup several years prior was inconclusive and had included liver biopsy that showed early stage liver disease.
Repeat laboratory test results were significant for elevated total bilirubin, alkaline phosphatase, alanine aminotransferase, and aspartate aminotransferase. The celiac panel showed elevated levels of serum tissue transglutaminase immunoglobulin A and deamidated gliadin immunoglobulin A. Investigation for other causes of hepatitis including viral (Hepatitis A, B & C; HIV; EBV; CMV), autoimmune (ANA, AMA, ASMA), Hemochromatosis, and Wilson’s disease were normal/negative. Abdominal Magnetic resonance imaging (MRI) with intravenous contrast showed evidence of portal hypertension including moderate splenomegaly, trace mesenteric edema along with ascites, and numerous distal esophageal and proximal gastric submucosal varices.
Abnormal hepatic morphology consistent with chronic liver disease was noted along with mild atrophy of the right liver and compensatory hypertrophy of the left lateral and caudate lobes. A repeat liver biopsy showed benign parenchyma without evidence of cirrhosis; ductal fibrosis and nodular regenerative changes were noted consistent with non cirrhotic portal hypertension (Figure 1 and 2).
Esophagogastroduodenoscopy (EGD) showed large varices requiring banding in the distal esophagus, as well as significant scalloping and villous atrophy of the duodenal mucosa. Duodenal biopsies showed significant intraepithelial lymphocytosis, villous blunting and crypt hyperplasia, consistent with Marsh 3B-C classification diagnostic for celiac disease (Figure 3). A gluten free diet was initiated and he was noted to have normalization of the liver function tests along with a significant decrease in tissue transglutaminase antibody levels (Table 1). On surveillance luminal exams there was significant improvement in the varices noted as well.
|
|
Normal Range |
Before GFD |
After GFD ( 5 months follow up) |
|
Hemoglobin (g/dL) |
13.0 - 16.5 |
15.2 |
14.0 |
|
Whit blood count [10(3)/mcL] |
4.00 - 12.00 |
9.20 |
4.27 |
|
Platelet [10(3)/mcL] |
140 - 440 |
143 |
118 |
|
MCV (fL) |
82.0 - 96.0 |
87.6 |
90.3 |
|
Serum Albumin (g/dL) |
3.5 - 5.0 |
4.1 |
3.9 |
|
INR |
0.9 - 1.2 |
1.1 |
1.1 |
|
AST (U/L) |
5 - 34 |
90 |
45 |
|
ALT (U/L) |
0 - 55 |
90 |
45 |
|
ALP (U/L) |
40 - 150 |
160 |
139 |
|
Total Bilirubin (mg/dL) |
0.2 - 1.2 |
3.1 |
0.9 |
|
Creatinine (mg/dL) |
0.70 - 1.30 |
0.83 |
1.03 |
|
tTG IGA (U/mL) |
<15.0 |
> 250.0 |
17.1 |
|
Deamidated gliadin IGA (U/mL) |
<15.0 |
> 250.0 |
|
|
Spleen length (cm) |
11 |
19 (MRI abdomen) |
15.9 (ultrasound abdomen) |
Table 1: Table showing laboratory values before and after initiation of Gluten free diet.
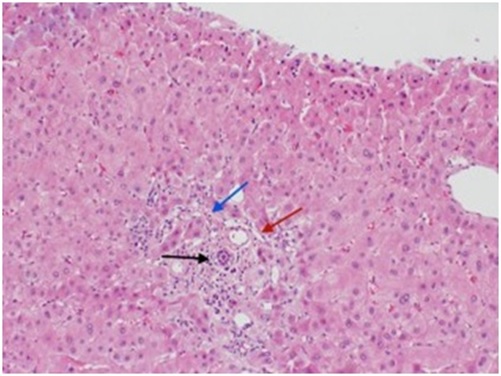 Figure 1: Liver biopsy showing inflammatory cell infiltrates (black arrow), slit-like spaces representing narrowing of portal veins (red arrow) and sinusoidal fibrosis (blue arrow).
Figure 1: Liver biopsy showing inflammatory cell infiltrates (black arrow), slit-like spaces representing narrowing of portal veins (red arrow) and sinusoidal fibrosis (blue arrow).
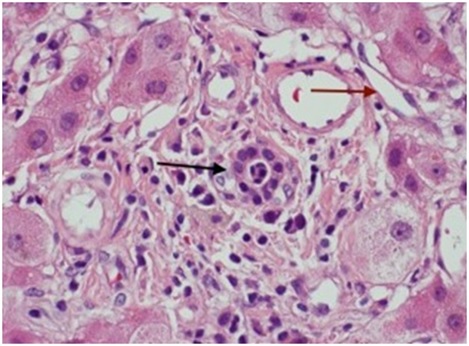 Figure 2: Shows a closer look of the nodular regenerative changes with inflammatory cell infiltrates (black arrow) and narrowing of the portal veins (red arrow).
Figure 2: Shows a closer look of the nodular regenerative changes with inflammatory cell infiltrates (black arrow) and narrowing of the portal veins (red arrow).
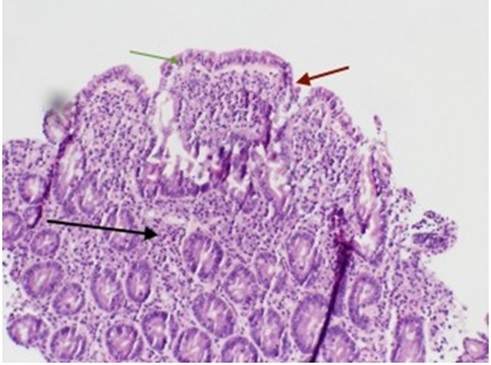 Figure 3: Duodenal biopsy showing villous atrophy (red arrow), crypt hyperplasia (black arrow), and intraepithelial lymphocytosis (green arrow).
Figure 3: Duodenal biopsy showing villous atrophy (red arrow), crypt hyperplasia (black arrow), and intraepithelial lymphocytosis (green arrow).
Discussion
IPH is diagnosed after excluding other causes of portal hypertension such as cirrhosis or extrahepatic portal vein obstruction [1]. The exact pathophysiology is still unknown but literature review thus far suspects this to be due to obliteration of the intra hepatic microcirculation [2,4,6,9,10]. Due to this obliteration there is decreased blood perfusion to the hepatocytes causing atrophy of these cells in the central region with compensated hyperproliferation in the portal regions ultimately leading to nodular reactive hyperplasia [4]. The progression of liver injury in these patients is due to extension of thrombosis into the sinusoids, kupffer cells, and small hepatic veins from the portal venous microcirculation [2,10]. In 2015 Schouten Jeoffrey, et al proposed 5 categories for the pathogenesis of IPH: immunologic, infectious mostly chronic, medication/toxic exposure, genetic conditions, and prothrombotic conditions [4]. Some studies also mention the repetitive antigen stimulation of the portal veins can also contribute to portal hypertension and thus the process of thrombus formation [2].
Celiac disease or celiac sprue, is an autoimmune response against the gluten proteins usually found in food such as wheat, barley, and rye [5,7,9,11]. Patients with CD have a wide spectrum of symptoms ranging from silent/asymptomatic to severe diarrhea, steatorrhea, metabolic bone disease, anemia, neurological symptoms, weight loss, and malabsorption [1,5,8,11]. CD is associated with immunological liver disorders such as autoimmune hepatitis and primary biliary cirrhosis, but is less commonly associated with portal hypertension alone [8]. Several hypotheses suggest increased intestinal permeability due to immunoreactivity against gluten leads to greater exposure of toxins, antigens, and cytokines to the portal circulation [6,9]. Subsequent hepatic injury is suspected to be a result of inflammatory and immunological activation of cellular immunity, and specific T cells against gluten. These immune cells produce inflammatory cytokines such as immune interferon (INF) alpha and Interleukin 10, which causes injury of the endothelial cells [3,5,6,9]. The increased Immunoglobulin A anticardiolipin antibodies and protein-phospholipid complex depositions in the portal vein also leads to thrombus formation by affecting the ability of vascular remodeling of small branches of the portal vein [4,6]. CD patients are at increased risk of thrombus formation due to the malabsorption of vitamin K resulting in a deficiency of prothrombotic factors such as protein C and S [7,11,12]. The improvement of liver function and portal hypertension after initiation of a GFD suggests that the decrease in the immunological response to gluten results in fewer immune complex deposits and aberrant immune response [3,6,9,11].
Conclusion
Celiac disease and its coexistence with idiopathic portal hypertension is a very rare entity. This association is most commonly found in the Eastern countries. The highest risk of deaths in IPH are related to variceal bleeding followed by hepatic failure as this is a progressive disease if left untreated. Therefore serological testing for celiac disease should be incorporated as a part of work up in patients with unexplained transaminitis. Early recognition and initiation of gluten free diet in these patients have shown significant improvement in their overall health and prognosis.
References
- Matar K, Musallam R, Sharma M (2017) Celiac Disease and “Idiopathic” Portal Hypertension: A Case Report and Review of Gastro Med Res 1.
- Yazdani S, Abdizadeh A (2018) Coeliac disease as a potential cause of idiopathic portal hypertension: a case report. Gastroenterol Rep 6: 149-151.
- Zamani F, Amiri A, Shakeri R, Zare A, Mohamadnejad M (2009) Celiac disease as a potential cause of idiopathic portal hypertension: a case J Med Case Reports 3: 68.
- Schouten JNL, Verheij J, Seijo S (2015) Idiopathic non-cirrhotic portal hypertension: a review. Orphanet J Rare Dis 10:67.
- Kara B, Sandikci M (2007) Successful treatment of portal hypertension and hypoparathyroidism with a gluten free diet. J Clin Gastroenterol 41: 724-725.
- Biecker E, Fischer HP, Schepke M (2011) Nodular regenerative hyperplasia and portal hypertension in a patient with celiac disease. Case Rep Gastrointest Med
- Kochhar R, Masoodi I, Dutta U, Singhal M, Miglani A, et al. (2009) Celiac disease and Budd Chiari syndrome: report of a case with review of literature. Eur J Gastroenterol Hepatol 21: 1092-1094.
- Sharma BC, Bhasin DK, Nada R (2006) Association of celiac disease with non-cirrhotic portal J Gastroenterol Hepatol 21: 332-334.
- Gaur K, Sakhuja P, Puri AS, Majumdar K (2016) Gluten-Free Hepatomiracle in “Celiac Hepatitis”: A Case Highlighting the Rare Occurrence of Nutrition-Induced Near Total Reversal of Advanced Steatohepatitis and Cirrhosis. Saudi J Gastroenterol 22: 461-464.
- Eapen CE, Nightingale P, Hubscher SG, Lane PJ, Plant T, et al. (2011) Non-cirrhotic Intrahepatic Portal Hypertension: Associated Gut Diseases and Prognostic Factors. Dig Dis Sci 56: 227-235.
- Scully RE, Mark EJ, Mcneely WF, Ebeling SH, Phillips LD, et al. (1999) Case Records of the Massachusetts General Hospital. N Engl J Med.
- Singh B, Shah P, Rajmani M, Pokharna RK, Ashdhir P, et al. (2015) Association of celiac disease and portal hypertension: Cirrhotic or noncirrhotic. Indian J Gastroenterol 34: 77.
Citation: Reddy Y, Asif A, Jandura D, Pisoh WNE (2021) Idiopathic Portal Hypertension in a Celiac Disease Patient: A Rare Association. J Gastroenterol Hepatology Res 6: 033.
Copyright: © 2021 Yeshaswini Reddy, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

