Imaging of Normal and Abnormal Cranio-Vertebral Junction - A Pictorial Review
*Corresponding Author(s):
Venkatraman BhatDepartment Of Radiology, Mazumdar Shaw Medical Center, Narayana Health City, Bangalore, India
Tel:91 9481027387,
Email:bvenkatraman@gmail.com
Abstract
Craniovertebral Junction (CVJ) is an important region in the human body designed for optimal movements of head while maintaining structural integrity and to allow smooth transition of vital neural and supporting structures to the lower body.Thus anatomical structures of CVJ are designed for stability as well as flexibility. CVJ is a frequent site of various pathological processes; some of them are unique to the location. Also being a transitional zone, many developmental variations and malformations are noted in the region. This essay attempts to provide quick reference to regional anatomy, variations and pathology, illustrated with relevant images and diagrams. Multiple examples of some common developmental abnormalities and few acquired regional pathology are presented.
Introduction
The Craniovertebral Junction (CVJ) [also called cranio cervical region] is a collective term that refers to the following structures-occiput (posterior skull base), atlas, axis and supporting ligaments. It encloses the soft tissue structures of cervico-medullary junction. (Medulla, spinal cord and lower cranial nerves) CVJ is well visualised in many imaging studies, namely the conventional radiography, Computed tomography and Magnetic resonance imaging (MRI) studies. It is partially visible in the routine imaging studies of the brain. These imaging studies can additionally provide dynamic information when performed with appropriate movements. On radiographs cranio-caudal range of CVJ extends from a line drawn between the internal occipital protuberance and the midpoint of the distance from the dorsum sellae and anterior margin of the Foramen Magnum (FM) to the level of second and third cervical inter-vertebral space [1].
There are objective measurements for position of various bony components of CVJ on radiography. Measurements can be done using conventional or cross sectional radiological examinations. Evaluation of these measurements helps in confirming and documenting CVJ relationship. Also serves as guide to objective post-surgical follow up. Following anatomical landmarks are needed on lateral and coronal views, to assess CVJ relationships and to perform basic craniometric measurements [1] (Figure 1a) (Table 1).
|
Important landmaks for CVJ Craniometry |
|
|
Cranial |
Nasion (N) |
|
Tuberculum sella (T) |
|
|
Basion [anterior margin of the foramen magnum](B) |
|
|
Opisthion [posterior margin of the foramen magnum] (O) |
|
|
Lowermost part of Occipital bone |
|
|
Cervico-Facial |
Posterior pole of the Hard Palate (HP) |
|
Anterior arch of the atlas (AA) |
|
|
Posterior arch of the Atlas (PA) |
|
|
Odontoid Process (OD) |
|
Table 1: Shows important landmarks for drawing Cranial and Cranio-cervical planes [1-3].
Utilizing these landmarks, many lines/planes are drawn. Description,interpretation and significance of the lines/plane are provided herewith in (Table 2).
|
Cranio-Vertebral Junction |
|||
|
Categories |
Subgroups |
Observations |
Importance |
|
Cranial landmarks |
Basal angle |
128-148º |
Assessing skull deformity |
|
|
Boogards angle |
119-135º |
|
|
|
Bi-mastoid line |
Intrinsic inclination of skull base |
|
|
|
McRays Line |
|
Reference plane for FM |
|
Cranio-cervical landmarks |
Bimastoid-diagastic lines |
Cranio-cervical abnoramal transtion |
Basilar invagination |
|
|
Chamberlein Line |
Normally Odontoid tip = 7 mm or below |
Measure of Cranio-cervical transition |
|
|
Mc Gregor line |
Normally Odontoid tip = 8-10 mm or below |
|
|
|
Wakenheims line/angle |
150-180º |
|
|
|
Atlanto-occipital axis angle |
124-127º (average) |
|
Table 2: Measurement and values for Cranio-vertebral normalcy and common pathological conditions [1,4-6].
Chamberlain's line (CL): A line extending between posterior pole of the hard palate and opisthion (Figure 1b)
Interpretation:
- • Tip of dens commonly lies below or just tangential to this line or occasionally it may normally project few mm above this line
- • Maximum distance accepted above the line is 1 ± 6.6 mm [1]
- • If distance of more than 7 mm it is considered abnormal [2]
McGregor line: McGregor developed a modification of the CL in situations when opisthion could not be identified. This line is drawn between the posterior pole of the hard palate to the most inferior surface of occipital bone (Figure 1b).
Interpretation: In 90% of individuals the odontoid apex should not lie above this line > 8 mm in males and > 10 mm in females
- • If more than the defined value it is suggestive of Basilar Invagination (BI) [2]
McRae's line: This is the plane of foramen magnum, drawn by a line drawn between the basion and opisthion. (Figure 1d)
Tip of the dens should be below this line, if above this line suggestive of BI [7]
Wackenheim clivus baseline (basilar line): Refers to the line along the clivus, which is tangential to posterior aspect of the dens. If the tip of the odontoid process remains significantly superior to Wackenheim’s clival line, it represents an abnormality (Figure 2b).
Interpretation: BI results with rostral positioning of the plane of the FM in relation to the brainstem [8].
Clivus canal angle: Constitutes the angle formed at the intersection of the Wackenheim clivus baseline with a line constructed along posterior surface of axis body and dens (Figure 2c).
Normally the angle 150-180° ventral cord compression can occur if angle is < 150º [4].
Welcher basal angle: Angle formed by intersection of the nasion-tuberculum line and tuberculum-basion line (Figure 2a).
It averages 132º and should remain below 140º. It is increased in platybasia [9].
Boogard's angle: This angle is formed between MacRae’s line and line along plane of the clivus (from dorsum sellae to basion). Normally it ranges from 119º to 135º [2] (Figure 2d).
Atlanto-occipital joint axis angle: This angle is formed at the intersection of tangents drawn parallel to the atlanto-occipital joints. These tangents typically intersect at centre of the odontoid process when the condyles are symmetric. Normally the average angle measures 124º to 127º (Figure 2f). Angle becomes more obtuse in occipital condylar hypoplasia [3].
Fishgold's Digastric Line: This is the line between the incisurae mastoideae (origin of the digastric muscles). (Figure 2e).
Normal: Tip of the dens should be within the range of 11 mm (± 4) [3].
Bimastoid Line: Refers to line connecting the tips of both mastoid processes (Figure 2e).
Tip of the dens should be < 10mm above this line [3]
Klaus height index: This is the vertical distance between the tip of the dens and line drawn from the tuberculum sellae to the internal occipital protuberance (Figure 1c).
If values remain between 30-36 mm, it indicated tendency towards basilar impression.
If dimension is
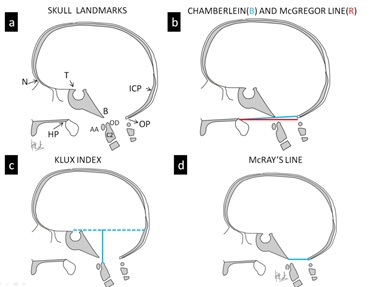 Figure 1: Skull landmarks and lines. (a) Skull diagram in the lateral perspective shows important landmarks. Diagrams illustrate Chamberlain, McGregor lines (b), Klux index (c) and McRays line (d).
Figure 1: Skull landmarks and lines. (a) Skull diagram in the lateral perspective shows important landmarks. Diagrams illustrate Chamberlain, McGregor lines (b), Klux index (c) and McRays line (d).
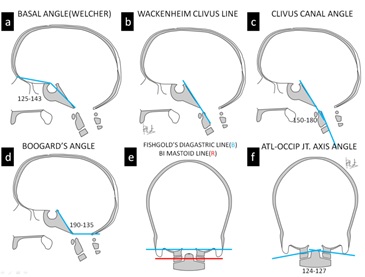
Figures 2: Additional Skull lines (a) Skull diagram in the lateral perspective shows (a) Basal angle (b) Wackenheims clivus line, (c) Clivus-canal angle, (d) Boogards angle, (e) Bi-diagastic (Blue), Bi-mastoid lines (Red) and (f) Atlanto-occipital joint axis angle.
Abbreviations: N-Nasion,T-Tuberculum sellae, D-Dorsum sellae, B-Basion, OP_Opthion, IOP-Internal occipital protuberance, HP-Hard palate, OD-Odontoid process and AA-Anterior arch of atlas.
Most of the above descriptions refers either to the relationship between intrinsic parts of skull base (e.g. platybasia) or to the relationship between skull base and cervical spine. (e.g. Basilar invagination or impression) Malformations at CVJ sometimes complicate the measurement process due to absence of standard reference points. Some conditions of CVJ may be asymptomatic, others manifest with long standing consequences. Hence it is vital for the imaging specialist to report anatomical integrity of the region, predict stability of the articulations; record standard measurements for immediate and long term follow up. Equally important is to recommend MRI or dynamic studies when there is likelyhood of associated neural or ligamentous abnormality or likely possibility of instability.
Basilar Invagination
This condition refers to an abnormally high position of the part of the vertebral column, protruding into the skull base (Figure 3). BI is an intrinsic skull condition with skull base deformity and abnormal relationship between FM and posterior fossa structures [3,10]. There is often deficient development of clivus, transitional anomalies of components of occipital bone and/or abnormal inclination of skull base around the region of foramen magnum.
As mentioned earlier, the following reference standards are used for diagnosis of basilar invagination.
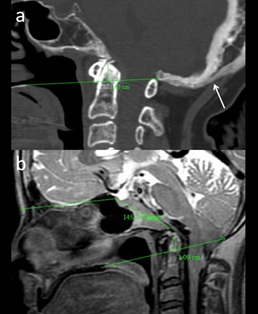 Figure 3: (a) 55-yr-old patient with neck pain, diagnosed with Paget’s disease with Basilar Impression. Sagittal CT image demonstrates skull bone expansion cortex thickening (arrow) and basilar invagination (b) 15-yr-old patient with limitation of neck movement, diagnosed with platybasia with basilar invagination. Sagittal T2 MR image demonstrates increased Welcher Basal angle. Basilar Invagination (tip of dens – 10.9 mm above Chamberlain’s line).
Figure 3: (a) 55-yr-old patient with neck pain, diagnosed with Paget’s disease with Basilar Impression. Sagittal CT image demonstrates skull bone expansion cortex thickening (arrow) and basilar invagination (b) 15-yr-old patient with limitation of neck movement, diagnosed with platybasia with basilar invagination. Sagittal T2 MR image demonstrates increased Welcher Basal angle. Basilar Invagination (tip of dens – 10.9 mm above Chamberlain’s line).
Chamberlain's line: Tip of dens commonly lies below or just tangent to this line or it may normally project few mm above this line. Maximum distance that it generally observed is 1 ± 6.6mm [1]. If extends more than 7 mm, it is considered abnormal [2].
McGregor line: In 90% of individuals the odontoid apex should not lie above this line > 8 mm in males and > 10 mm in females. If more than that it is suggestive of BI [2].
McRae's line: Tip of the dens should be below this line, if above this line suggestive of BI [7].
Wackenheim clivus baseline: If the tip of the odontoid process remains significantly superior to Wackenheim’s clival line represents abnormality. BI results with rostral positioning of the plane of the FM in relation to the brainstem [8].
Basilar Impression (BIM)
In BI and BIM there is similar cranial migration of vertebral column. In BI there is abnormal development of anatomical components of CVJ whereas BIM is associated with bone softening in a normal developed bone [1]. Condition can be either congenital or acquired. Similar mal-positioning of the odontoid process can be seen following deformity secondary to trauma.
Deformation due to bone softening is seen in many diseases such as Paget disease, osteomalacia, severe osteoporosis, osteogenesis imperfecta, rickets, hyperparathyroidism, renal osteodystrophy, skull base infection and in mucopolysaccharidosis. Deformity in these conditions is also referred to as secondary BI [11].
Platybasia
‘Platybasia’ refers to abnormal flattening of the skull base, can be seen in association with basilar invagination. Platybasia occur in a variety of congenital disorders like craniofacial anomalies, osteogenesis imperfecta, cleido-cranial dysostosis and ACM. Similar changes may be seen in association with deformity due to bone softening in Paget disease, osteomalacia, rickets and trauma [12].
On radiographic measurement, platybasia is associated with abnormal obtuseness of the Welcher Basal angle. Normally the angle should be < 140º; Angle is increased in the platybasia [5].
Decreased Boogard's angle can also be observed. Normally angle ranges from 119º to 135º [2].
On the etiological basis, CVJ abnormalities can be divided into two broad categories; congenital and acquired conditions (Table 3).
|
Common pathological conditions of CVJ |
|||
|
Category |
Specific entity |
Presentation-features |
Additional significance |
|
Congenital anomaly |
Rachischisis |
Incidental |
Associated anomalies |
|
Clival hypoplasia |
Incidental |
||
|
Pro-atlas anomaly |
Occipitalisation of C1, Condylar defects |
Limitation of movement Susceptible for trauma |
|
|
Atlanto-axial instabilty |
Unstable |
||
|
Fusion-segmentation defect |
Scoliosis |
||
|
Klippel Feil anomaly |
Syndromic, Multisystem |
Short spine, Anomalies |
|
|
Syndromic |
Morquios Syndrome |
Congenital entities with variable presentation |
Subluxation, spinal compression. Late manifestation of symptoms |
|
Spondylo-epiphyseal dysplasia, Cleido cranial dysplasia |
|||
|
Down’s Syndrome |
A-A Subluxation |
||
|
Trauma |
Non-displaced Fracture |
Minor |
Stable |
|
Displaced Injury/dislocation |
High velocity injury |
Unstable, Neural injury |
|
|
Rotatory subluxation |
Pediatric, Trauma, inflammatory |
Self limiting |
|
|
Inflammatory |
Septic |
Diabetic, acute symptoms |
Epidural abscess |
|
Tuberculosis |
Insidious onset, subluxation |
Subluxation, epidural abscess |
|
|
Rheumatoid |
Systemic,Erosions |
Subluxation |
|
|
Eosinophilic granuloma |
lytic lesions |
Healing-recovery |
|
|
Neoplastic |
Primary - Chordoma, Sarcoma, GCT |
Expansion, osteolysis /sclerosis, new-bone formation |
Needs MRI, PET |
|
Secondary |
Breast, Thyroid, Lung |
||
|
Misc |
Paget’s disease |
Skull softening, BI, deformity |
Deformity Cord compression |
|
Osteogenesis imperfecta |
|||
|
Osteomalacia, Hyperparathyroidism |
|||
Table 3: Table showing various entities affecting the CVJ.
Congenital Causes [1,5,10]
In this category, depending upon specific entity either there is structural abnormality of components of CVJ or deformity secondary to bone softening due to a congenital condition. Often there are associated neural anomalies or secondary neural compression. Syndromic associations demonstrate more extensive systemic involvement. In conditions like Downs’s syndrome, Achondroplasia, MPS and spondyloepiphyseal dysplasia, the atlanto-odontoidal instability may manifest later in life. Following is a brief list of abnormalities.
- Occiput: Condylus tertius (Figure 4a) Condylar hypoplasia, Basi-occiput hypoplasia (Figure 5) and Atlanto-occipital assimilation (AOA) (Figures 6 and 7).
- Atlas: Anterior and posterior arch anomalies, Split atlas, Aplasia of arch and Hypoplasia of arch.
- Axis: Persistent ossiculum terminale (Figure 4c), Odontoid aplasia, Os Odontoideum (Figure 4b), Dens bicornis, Os Avis and Anteverted odontoid.
- Arnold-Chiari Malformations (Figure 8)
- Atlanto-Axial dislocation
- Syndromes: Klippel-Feil (Figure 9) and Down ’s syndrome (Figure 10c)
- Skeletal Dysplasia: Achondroplasia, Spondylo-epiphyseal dysplasia and Mucopolysaccharidosis (MPS 4) (Figures 10d and 11)
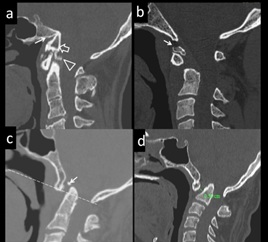
Figure 4: Asymptomatic, 16yr-old-male, diagnosed with a Proatlas anomaly. (a) Condylus tertius. Sagittal CT image shows clival hypoplasia (arrow), condylus tertius (open arrow) and C2-C3 block vertebrae. (b)12 yr-male with neck pain, diagnosed with Os odontoideum. Sagittal CT image demonstrates Os odontoideum (arrow). (c) 10-yr-old with neck stiffness diagnosed with Persistent ossiculum terminale. Sagittal CT image reveal Persistent ossiculum terminale (arrow). There is associated basilar invagination. (d) 13-yr-old male with limitation of neck movement diagnosed with Atlanto-axial dislocation. Sagittal CT Image shows increased atlanto-dental distance (5.6 mm) indicating atlanto-axial dislocation. Also there is fusion of anterior arch of C1 with clivus and basilar invagination.
 Figure 5: 22-yr-old presened with recurrent neck and backache, diagnosed with shortened clivus, basilar invagination and basiocciput hypoplasia. Sagittal T1W MRI image shows shortened clivus and basi-occiput hypoplasia (arrow), basilar invagination. (open arrow) and crowding at foramen magnum.
Figure 5: 22-yr-old presened with recurrent neck and backache, diagnosed with shortened clivus, basilar invagination and basiocciput hypoplasia. Sagittal T1W MRI image shows shortened clivus and basi-occiput hypoplasia (arrow), basilar invagination. (open arrow) and crowding at foramen magnum.
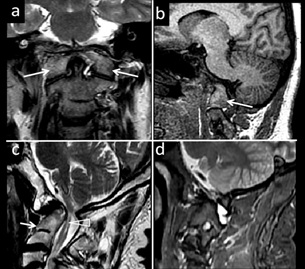 Figure 6: 23-yr old male with lower limb weakness,neck pain diagnosed with altalto-occipital assimilation. (a) Coronal T2W MR image shows with atlanto-occipital assimilation.(arrows) (b) Para-Sagittal T1W MR image demonstrates atlanto-occipital assimilation. . (c) Case of C2-C3 block vertebra with myelomalacia Sagittal T2W MR image shows C2-C3 block vertebra(arrow) and myelomalacia (triangle) (d) Parasagittal T1W image demonstrates C2-C3 block vertebra.
Figure 6: 23-yr old male with lower limb weakness,neck pain diagnosed with altalto-occipital assimilation. (a) Coronal T2W MR image shows with atlanto-occipital assimilation.(arrows) (b) Para-Sagittal T1W MR image demonstrates atlanto-occipital assimilation. . (c) Case of C2-C3 block vertebra with myelomalacia Sagittal T2W MR image shows C2-C3 block vertebra(arrow) and myelomalacia (triangle) (d) Parasagittal T1W image demonstrates C2-C3 block vertebra.
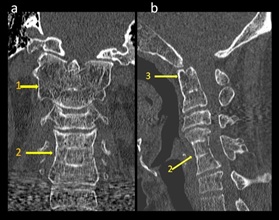 Figure 7: 24-yr –old female presenting with short neck, neck stiffness, diagnosed with Atlanto axial fusion and C4-6 block vertebra (a) Coronal CT Image shows fusion of lateral masses of C1 with C2 bilaterally (1); C4- 6 block vertebra (2) shows diffuse osteopenia. (b) Sagittal CT Image shows C4, C5, C6 block vertebra (2) and fusion of anterior arch of C1 with dens (3).
Figure 7: 24-yr –old female presenting with short neck, neck stiffness, diagnosed with Atlanto axial fusion and C4-6 block vertebra (a) Coronal CT Image shows fusion of lateral masses of C1 with C2 bilaterally (1); C4- 6 block vertebra (2) shows diffuse osteopenia. (b) Sagittal CT Image shows C4, C5, C6 block vertebra (2) and fusion of anterior arch of C1 with dens (3).
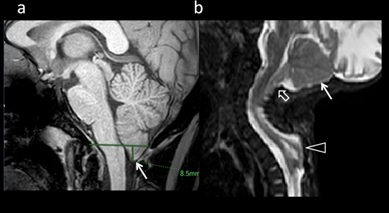 Figure 8: 6 yr old male with intermittant neck pain, diagnosed with(a) Chiari malformation type 1. Chiari Malformation type 1. Peg-like herniation of cerebellar tonsil, 8.5 mm below McRae’s line is noted. (b) 7-month-old, female presented with dorsal swelling, diagnosed with Chari malformation II. T2W Sagittal MRI demonstrates small posterior fossa (arrow), descent of cerebellum (open arrow) and brainstem in to the spinal canal. There is associated thoracic meningocele (Triangle).
Figure 8: 6 yr old male with intermittant neck pain, diagnosed with(a) Chiari malformation type 1. Chiari Malformation type 1. Peg-like herniation of cerebellar tonsil, 8.5 mm below McRae’s line is noted. (b) 7-month-old, female presented with dorsal swelling, diagnosed with Chari malformation II. T2W Sagittal MRI demonstrates small posterior fossa (arrow), descent of cerebellum (open arrow) and brainstem in to the spinal canal. There is associated thoracic meningocele (Triangle).
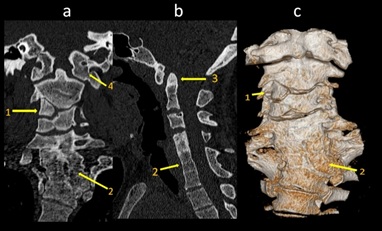 Figure 9: 7-yr-old female with torticollis, short neck, diagnosed with Klippel – feil syndrome(a) Coronal CT Image demonstrates C3 hemivertebra (1); C5, C6, C7 block vertebra (2) and Atlanto-occipital assimilation (4) (b) Sagittal CT image reveals basilar invagination (3); C5, C6, C7 block vertebra (2) (c) Volume rendered 3D Image shows C3 hemivertebra (1);C5, C6, C7 block vertebra (2).
Figure 9: 7-yr-old female with torticollis, short neck, diagnosed with Klippel – feil syndrome(a) Coronal CT Image demonstrates C3 hemivertebra (1); C5, C6, C7 block vertebra (2) and Atlanto-occipital assimilation (4) (b) Sagittal CT image reveals basilar invagination (3); C5, C6, C7 block vertebra (2) (c) Volume rendered 3D Image shows C3 hemivertebra (1);C5, C6, C7 block vertebra (2).
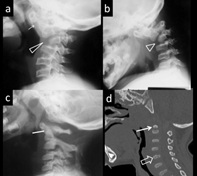 Figure 10: 3-yr-old with neck deformity diagnosed with hypoplastic C3, A-A subluxation. (a and b) Extension and flexion views of lateral cervical spine demonstrate A-A subluxation (arrow) and Dysplastic C3 vertebra. (c ) 11-month-old with Down’s’ syndrome diagnosed with hypoplastic dens ( line). (d) 6-month-old female of Morquio syndrome. Sagittal CT image of an infant shows platyspondyly with vertebral beaking (open arrow) and hypoplastic dens (arrow).
Figure 10: 3-yr-old with neck deformity diagnosed with hypoplastic C3, A-A subluxation. (a and b) Extension and flexion views of lateral cervical spine demonstrate A-A subluxation (arrow) and Dysplastic C3 vertebra. (c ) 11-month-old with Down’s’ syndrome diagnosed with hypoplastic dens ( line). (d) 6-month-old female of Morquio syndrome. Sagittal CT image of an infant shows platyspondyly with vertebral beaking (open arrow) and hypoplastic dens (arrow).
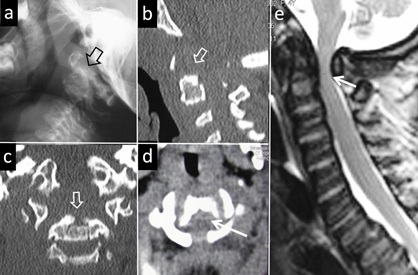 Figure 11: 4-year-old female, known case of MPS-4 syndrome with the neck stiffness. (A) Lateral radiograph of the neck reveals the hypoplasia and deformity (arrow-head) of odontoid process. Rest of the cervical vertebral bodies also demonstrate deformity. Sagittal (b) and coronal(c) reconstruction of CT re-demonstrate hypoplasia and deformity of the odontoid. Deformed C1 and the rest of the cervical vertebra are also visualised. Axial image at the level of C2 (d)shows compression of the cord (arrow) due to dorsally displaced odontoid. (e) Extent of cervico- medullary compression is the demonstrated in a Sagittal T2 MR image (arrow).
Figure 11: 4-year-old female, known case of MPS-4 syndrome with the neck stiffness. (A) Lateral radiograph of the neck reveals the hypoplasia and deformity (arrow-head) of odontoid process. Rest of the cervical vertebral bodies also demonstrate deformity. Sagittal (b) and coronal(c) reconstruction of CT re-demonstrate hypoplasia and deformity of the odontoid. Deformed C1 and the rest of the cervical vertebra are also visualised. Axial image at the level of C2 (d)shows compression of the cord (arrow) due to dorsally displaced odontoid. (e) Extent of cervico- medullary compression is the demonstrated in a Sagittal T2 MR image (arrow).
Acquired Causes [2,12]
Large majority of acquired conditions either belong to infective processes or result of trauma. CT and MRI imaging optimally demonstrate the bony and soft tissue abnormalities. Evaluation of dynamic status of CVJ when clinically needed is performed voluntarily or passively under the supervision of physician.
- Infectious causes: CVJ Tuberculosis (Figure 12) and Septic arthritis
- Arthritis: Rheumatoid arthritis (Figure 13) and Ankylosing Spondylitis
- Trauma: Fractures of occipital condoyle, atlas, axis and ligament injuries (Figure 14)
- Neoplastic:
- Extradural Osseous and soft tissue: Chordoma, Chondrosarcoma, Osteoblastoma, Giant cell tumour, Aneurysmal bone cyst, Plasmacytoma, Eosinophilic granuloma (Figure 15) and Metastasis. (b) Intradural, extramedullary lesions: Meningioma, Arachnoid cyst and Nerve sheath tumours (Figures 16 and 17). Intramedullary lesions: Ependymoma, Astrocytoma and Hemangioblastoma
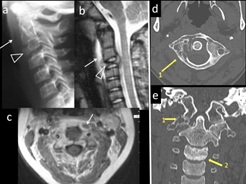 Figure 12: 5-yr-old child with fever, neck stiffness, diagnosed with tuberculosis of C2-3 vertebra. (a) Lateral cervical spine shows pre-vertebral soft tissue swelling (arrow), Loss of C2-3 disc space and C3 osteolytic lesion [triangle]. (b and c) T2W and T1 Contrast MR images show pre-vertebral and spinal collection and vertebral collapse. (d) 30 yr-old with weight loss and neck pain, diagnosed with tuberculosis of C1. Axial CT Image in an adult show lytic area in the right lateral mass of atlas (1). Coronal CT Image (e) reveals lytic areas in right lateral mass of atlas, C1-2 articulation (1) and sclerosis of C3 (2).
Figure 12: 5-yr-old child with fever, neck stiffness, diagnosed with tuberculosis of C2-3 vertebra. (a) Lateral cervical spine shows pre-vertebral soft tissue swelling (arrow), Loss of C2-3 disc space and C3 osteolytic lesion [triangle]. (b and c) T2W and T1 Contrast MR images show pre-vertebral and spinal collection and vertebral collapse. (d) 30 yr-old with weight loss and neck pain, diagnosed with tuberculosis of C1. Axial CT Image in an adult show lytic area in the right lateral mass of atlas (1). Coronal CT Image (e) reveals lytic areas in right lateral mass of atlas, C1-2 articulation (1) and sclerosis of C3 (2).
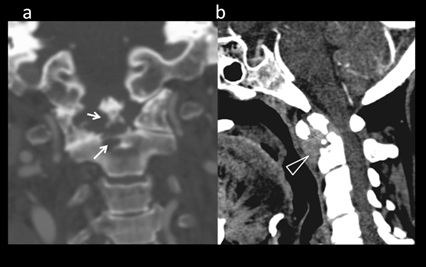 Figure 13: 49-yr-old with neck and multiple joint pain, diagnosed with Rheumatoid arthritis. (a) Coronal CT bone window shows erosions of odontoid process (arrows). Sagittal soft tissue window (b) shows pathological fracture at dens base. There is enhancing soft tissue surrounding the odontoid process (‘pannus’ formation) (triangle).
Figure 13: 49-yr-old with neck and multiple joint pain, diagnosed with Rheumatoid arthritis. (a) Coronal CT bone window shows erosions of odontoid process (arrows). Sagittal soft tissue window (b) shows pathological fracture at dens base. There is enhancing soft tissue surrounding the odontoid process (‘pannus’ formation) (triangle).
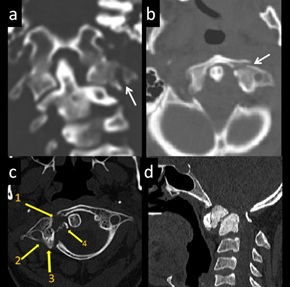 Figure 14: Fracture C1 examples. 25-yr-old involved in a road traffic accident, diagnosed with C1 fracture. (a and b) Coronal and axial CT image (a) demonstrates minimally displaced comminuted fracture of left C1 lateral mass (arrow). (c) 21 yr-old with h/o trauma, diagnosed with C1 fracture. Axial CT image- Comminuted fracture of anterior arch (1), right lateral mass (2) and posterior arch (3). Fracture fragment (4) (d) 7-yr-old with previous neck trauma, persistent neck deformity, diagnosed with old fracture odontoid. CT Sagittal image shows Chronic Type II fracture of odontoid process with sclerosis.
Figure 14: Fracture C1 examples. 25-yr-old involved in a road traffic accident, diagnosed with C1 fracture. (a and b) Coronal and axial CT image (a) demonstrates minimally displaced comminuted fracture of left C1 lateral mass (arrow). (c) 21 yr-old with h/o trauma, diagnosed with C1 fracture. Axial CT image- Comminuted fracture of anterior arch (1), right lateral mass (2) and posterior arch (3). Fracture fragment (4) (d) 7-yr-old with previous neck trauma, persistent neck deformity, diagnosed with old fracture odontoid. CT Sagittal image shows Chronic Type II fracture of odontoid process with sclerosis.
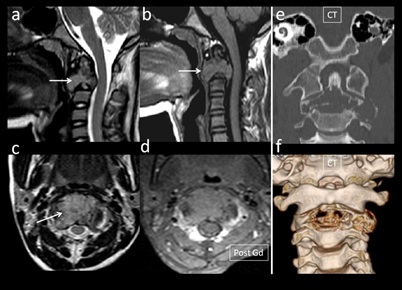 Figure 15: 11-yr-male with neck pain, diagnosed with epitheloid Sarcoma of C2 Vertebra.(a) T2W sagittal image shows iso to hyperintense (arrow) C2 body lesion, hyperintense in T1 image(b) (arrow) Axial T2W Image reveals T2w iso-hyperintense lesion(arrow: No significant enhancement on post-contrast image (d). Coronal CT image (e) shows expansile, osteolytic lesion in C2 body. Volume rendered image demonstrates lytic lesion involving C2 (f).
Figure 15: 11-yr-male with neck pain, diagnosed with epitheloid Sarcoma of C2 Vertebra.(a) T2W sagittal image shows iso to hyperintense (arrow) C2 body lesion, hyperintense in T1 image(b) (arrow) Axial T2W Image reveals T2w iso-hyperintense lesion(arrow: No significant enhancement on post-contrast image (d). Coronal CT image (e) shows expansile, osteolytic lesion in C2 body. Volume rendered image demonstrates lytic lesion involving C2 (f).
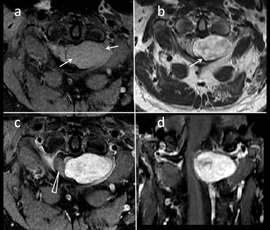 Figure 16: 25-yr-old with stiff neck, unsteady gait, diagnosed with a Neurofibroma.(a and b) Axial images demonstrate T1 isointense and T2w hyperintense (arrows) intradural extramedullary lesion at C1-C2 level left lateral aspect (c and d) T1w post contrast axial and coronal image shows enhancing intradural extramedullary lesion at C1-C2 with associated cord compression (triangle).
Figure 16: 25-yr-old with stiff neck, unsteady gait, diagnosed with a Neurofibroma.(a and b) Axial images demonstrate T1 isointense and T2w hyperintense (arrows) intradural extramedullary lesion at C1-C2 level left lateral aspect (c and d) T1w post contrast axial and coronal image shows enhancing intradural extramedullary lesion at C1-C2 with associated cord compression (triangle).
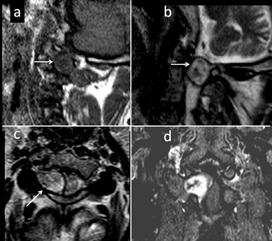 Figure 17: 27-yr-patient with shooting pain on right side on neck, diagnosed with a nerve root Schwannoma. (a and b) Parasagittal T1W(a) and T2W image (b) show TI hypo,T2 hyperintense extradural lesion. (c) T1W axial image shows isointense component (arrow). (d) T1W coronal contrast enhanced image shows enhancing lesion from right C2 exiting nerve root.
Figure 17: 27-yr-patient with shooting pain on right side on neck, diagnosed with a nerve root Schwannoma. (a and b) Parasagittal T1W(a) and T2W image (b) show TI hypo,T2 hyperintense extradural lesion. (c) T1W axial image shows isointense component (arrow). (d) T1W coronal contrast enhanced image shows enhancing lesion from right C2 exiting nerve root.
Some specific conditions are described in greater detail:
1. CVJ in Syndromic condition and Skeletal dysplasia:
In Down syndrome there is hypoplasia of odontoid in association with poorly developed ligaments (Figure 10c) Hence may show instability of occipitocervical or atlantoaxial joints. There is relatively low association of neurological symptoms, hence surgical management for stabilisation is considered controversial [14].
In Klippel-Feil syndrome a long term complication can occur due to alteration of cervical movement kinetics at fused and mobile vertebral segments. Occasionally C1 vertebra articulates with rest of the fused spine and act as site of maximal movement of cervical spine (Figure 9). Subsequently degenerative changes and secondary cervical myelopathy occur at C1-2 region.
CVJ and Spinal involvement is frequent in MPS-IV patients, may result in vertebral deformity, instability, canal stenosis and cervical myelopathy.(Fig 11) Changes in the bodies of vertebra are evident, even at early age (Fig 10 d) Screening MRI and follow up of patient is necessarily for detecting early neurological signs [15]. It has been observed that once objective neurological signs become evident in patients with MPS IVA, they tend to progress despite surgical intervention [16], hence surgical options should be carefully weighed.
Tuberculosis of the CV junction is an important cause of spastic quadriparesis in endemic region. It should be considered as a potential diagnosis in young patients, immune-compromised persons presenting with occipital neuralgia, upper cervical cord compression or atlanto-axial subluxation either occurring spontaneously or after a trivial injury. Early diagnosis and treatment are important in preventing long term neurological sequelae. Spinal TB accounts for 1% of all TB cases, in 6% in extra-pulmonary TB and comprises 50% of skeletal TB. CVJ-TB is still rarer with the reported incidence of 0.3% to 1% of all spinal TB [17]. CT is the most practical modality of imaging. Bony abnormalities like erosion of odontoid/axis-body/anterior-arch/posterior arch/clivus/occipital condoyle/ lateral mass, Atlanto-axial dislocation, increased prevertebral soft tissues and spinal compression are well (Figure 12). Grading of lesion is helpful in patient management. On the basis of CT CVJ, Lifeso graded CVJ TB into the following grades: Grade 2 and 3 are unstable; Grade3 has a poor prognosis [17].
Grade 1- increased prevertebral shadow
Grade 2- AAD and early bony changes
Grade 3- AAD, Gross destruction of bone and pathological fracture
MRI with gadolinium contrast enhancement better delineates the soft tissue abnormalities. Like collections in prevertebral, paravertebral and epidural planes/ extent of granulation tissue and secondary effect on the spinal cord.
2. Rheumatoid arthritis
The cervical spine can be involved in 17%–86% of patients with rheumatoid arthritis. It can involve the supra-axial or sub-axial spine along with the cranio-vertebral junction. In rheumatoid Arthritis there is an immunologic dysfunction leading to hypertrophy of the synovial tissue, pannus formation and erosion of the articular cartilage and subchondral bone (Figure 13). RA has a prevalence of 1-2% with an incidence is 27 per 100.000 of the general population [18].
The preferred modality for evaluation CVJ assessment in RA patients is MRI. It provides information about the size of rheumatoid pannus, the extent of bony and soft-tissue destruction and the status of the spinal cord. MRI also assesses migration of the odontoid, by measuring the Cervico-Medullary Angle (CMA). Values less than 135º are significant (Normal 135º and 175º) and vertical settling changes (basilar impression) correlate with myelopathy [18]. Flexion and extension MRI adds further information in RA. It has been observed that the subarachnoid space is significantly narrowed at the atlanto-axial and subaxial regions of spine in flexion in patient with RA. Subarachnoid space less then 6mm in flexion correlates with higher occurrence of paralysis [18].
3. Injury and Rotatory subluxation:
This is an extensive subject; complete description is beyond the scope of present discussion. Generally there are six injury types, which often coexist in a given patient:
- Occipital condyle fractures
- Craniocervical dissociation
- Fractures of the atlas
- C1–C2 ligamentous instability
- Odontoid fractures, and
- Traumatic spondylolistheses (hangman’s fractures) of C2
Cranio-Cervical Dissociation
Atlanto-odontoidal dislocation (AOD) is a devastating and often a fatal association in trauma. The head most often displaces anteriorly, but posterior AOD can also occur. The spectrum of injury includes complete loss of articulation to subtle subluxation. Signs of instability are translation or distraction of more than 2 mm in any plane, neurologic injury, or concomitant cerebro-vascular trauma.
The Harris technique, or the “rule of 12,” is the most useful, sensitive, and reproducible technique for characterizing AOD. This technique uses Basion-Dens Interval (BDI) and ADI. Lateral radiographs, midsagittal CT is recommended for diagnosis of AOD. The key component of analysis is based on assessing bony relationships using a number of lines on the lateral horizontal shoot-through cervical spine film: Following lines are of value [19].
- • Basion-dens interval (BDI) > 12 mm in adults
- • Basion-axial interval (BAI) > 12 mm in adults
- • Powers ratio > 1 (insensitive to a vertical distraction injury or posterior dissociation)
Atlantodental interval (ADI) > 3mm in adult males, >2.5mm in adult female
Atlanto-Axial Rotatory Subluxation (AARS)
This entity is of special interest in children who present with torticollis following trauma or retro-pharyngeal inflammation. (Grisel’s syndrome) [20]. Ligamentous laxity and hypermobility of C1-C2 articulations predispose to rotatory subluxation following injury. CT imagining demonstrates rotary subluxation of C1-C2 and excludes bony injury (Figure 18). 3-D reconstructions are helpful. The condition is often self limiting. Management is mostly conservative [20].
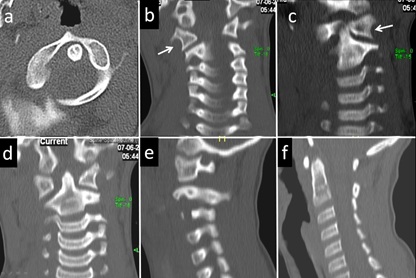 Figure 18: 2-year-old child with torticollis and restricted neck movement diagnosed with the rotatory subluxation C1/C2. (a) axial CT image at C1 level demonstrate anticlockwise rotation of the body of C1. The atlanto-odontoid relation is normal. Coronal CT images (b, c and d) reveal rotation of the first C2 in relation to C1 as demonstrated by altered relation of lateral mass articulation. (arrow) Odontoid remains central in position. Parasagittal CT reconstruction redemonstrating C2 body rotation in relation to the lateral mass of atlas. (f) Midline anatomy nearly remains normal.
Figure 18: 2-year-old child with torticollis and restricted neck movement diagnosed with the rotatory subluxation C1/C2. (a) axial CT image at C1 level demonstrate anticlockwise rotation of the body of C1. The atlanto-odontoid relation is normal. Coronal CT images (b, c and d) reveal rotation of the first C2 in relation to C1 as demonstrated by altered relation of lateral mass articulation. (arrow) Odontoid remains central in position. Parasagittal CT reconstruction redemonstrating C2 body rotation in relation to the lateral mass of atlas. (f) Midline anatomy nearly remains normal.
Tumors of the Craniovertebral Junction
The neoplasm in the region occurs either in osseous structures or extensions from the surrounding soft tissue. Rarely neoplasms arise from the neural structures. The diagnosis may be challenging by conventional imaging methods, presently the evaluation is greatly facilitated by cross sectional imaging modalities.
Regional Pathology And Differential Diagnosis
Regional pathology includes extra-axial lesions such as meningiomas and neurinomas. Meningiomas are more frequent than neuroma (3 times) occur often in females.
Neurofibromas of the CVJ are seen in association of neurofibromatosis, can be multiple. Enlarged foramen and evidence of bony erosion may help in the determination between meningioma and neurilemmoma (Figure 16). Tumors originating from the jugular foramen (schwannomas, glomus tumors, or paragangliomas) may extend to the CVJ (Figure 19). Other occasional osseous neoplastic lesions are chordoma, chondrosarcoma, plasmacytoma, osteoblastoma, fibrous dysplasia, metastatic tumor and giant cell tumor.
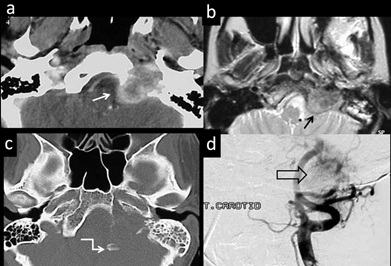 Figure 19: 69-year-old lady, known case of recurrent glomus jugulare tumour presenting with the torticollis and neck stiffness. (a) Axial contrast CT image demonstrate destructive vascular lesion centred in the left jugular fossa (arrow). (b) Axial T2 MR Image demonstrates salt-and-pepper appearance (black arrow). (c) CT bone window demonstrate extensive bone destruction of the occipital bone, adjacent body and condoyle with fragments in the posterior fossa (as zigzag arrow). Carotid angiogram (d) demonstrates tumour blush (open black arrow) and anterior displacement of the internal carotid artery at skull base.
Figure 19: 69-year-old lady, known case of recurrent glomus jugulare tumour presenting with the torticollis and neck stiffness. (a) Axial contrast CT image demonstrate destructive vascular lesion centred in the left jugular fossa (arrow). (b) Axial T2 MR Image demonstrates salt-and-pepper appearance (black arrow). (c) CT bone window demonstrate extensive bone destruction of the occipital bone, adjacent body and condoyle with fragments in the posterior fossa (as zigzag arrow). Carotid angiogram (d) demonstrates tumour blush (open black arrow) and anterior displacement of the internal carotid artery at skull base.
Rare lesions like desmoids, teratoma, neurenteric cysts, arachnoid cysts and fatty tumors are reported in the region. Metastatic involvement of CVJ is an important affection of the region, should be evaluated by MRI when there is a limitation of movement or neuralgia in a patient with known primary neoplasm. CVJ metastasis accounts for 0.5% of all spine metastases. Leading cause in many series is from the breast malignancy (Figure 20). Other primary malignancy included thyroid, lung, breast, renal and prostate carcinoma [21].
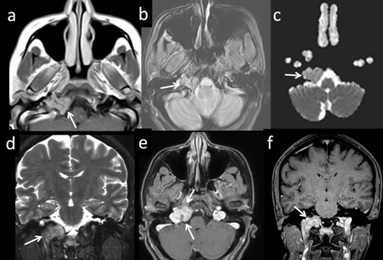 Figure 20: 50-year-old female with the h/o surgery for breast mass, presenting with the abnormal tongue movement. MRI images (T1, gradient, DWI and postcontrast) demonstrate (arrows) enhancing osteolytic lesion involving the right side of the occipital bone, extending to adjacent hypoglossal canal and jugular foramen (a, b, c, e and f). Involvement of the base of right occipital condoyle (arrows) is seen in the coronal views (D and F) Finding indicative of metastatic skull base involvement from breast malignancy.
Figure 20: 50-year-old female with the h/o surgery for breast mass, presenting with the abnormal tongue movement. MRI images (T1, gradient, DWI and postcontrast) demonstrate (arrows) enhancing osteolytic lesion involving the right side of the occipital bone, extending to adjacent hypoglossal canal and jugular foramen (a, b, c, e and f). Involvement of the base of right occipital condoyle (arrows) is seen in the coronal views (D and F) Finding indicative of metastatic skull base involvement from breast malignancy.
Conclusion
Craniovertebral junction is functionally and anatomically a complex region. It is often a site for congenital and acquired anomalies, some of which are treatable neurological disorders. Imaging of this complex region and reaching to a specific diagnosis continues to be a challenge for imaging specialists. While plain radiographs have an important role initially, multiplanar imaging with CT and MRI provides more specific and detailed information on bony and soft tissue structures. Adequate knowledge of regional embryology, understanding the anatomical complexity and range of regional disease processes are essential for arriving at an accurate diagnosis. Topographic relationships of important landmarks should be observed, measured with craniometrical data and well documented. Multiple radiological methods are essential in the diagnosis, categorisation of abnormality, predicting possible aetiology and enable effective management of patients, thus preserving the quality of life of patients suffering from these abnormalities. This presentation provides a quick reference and an image gallery to facilitate the analysis/interpretation of the anatomically complex region.
Acknowledgements
Authors profondly thank the collegues from Imaging service for the support and valuable inputs. Special thanks to the Chairman, Dr Devi Prasad Shetty, Narayana Health, Bengaluru for continued academic and administrative support.
References
- Smoker WR (1994) Craniovertebral junction: Normal anatomy, craniometry and congenital anomalies. Radiographics 14: 255-277.
- Joaquim AF (2013) Management of Basilar Invagination 24: 288-294.
- Mead LB II, Millhouse PW, Krystal J, Vaccaro AR (2016) C1 fractures: A review of diagnoses, management options and outcomes. Curr Rev Musculoskelet Med 9: 255-262.
- Bhuvaneswari V, Elangovan S (2000) Radiological quiz - head and neck. Indian J Radiol Imaging 10: 258.
- Chellapandian D, Panchapekesa CR, Rukmangatha SR, Parthiban M, Mahesh A (2004) The cervical spine involvement in rheumatoid arthritis and its correlation with disease severity. J Indian Rheumatol Assoc 12: 468-471.
- Van JJ, Sanchez GM, Alwyn L (2010) The Edwin Smith papyrus: A clinical reappraisal of the oldest known document on spinal injuries. Eur Spine J 19:1815-1823.
- Goel A (2009) Basilar invagination, Chiari malformation, syringomyelia: A review. Neurol India 57: 235-246.
- Bocciolini C, Dall'Olio D, Cunsolo E, Cavazzuti PP, Laudadio P (2005) Grisel's syndrome: A rare complication following adenoidectomy. Acta Otorhinolaryngol Ital 25: 245-249.
- Jain N, Verma R, Garga U, Baruah B, Jain S, et al. (2016) CT and MR imaging of odontoid abnormalities: A pictorial review. Indian J Radiol Imaging 26: 108-109.
- Piatt JH (2008) Surgical management of the Chiari malformation Type I: The way forward. J Neurosurg Pediatr 2: 50-51.
- Lopez AJ, Scheer JK, Leibl KE, Smith ZA, Dlouhy BJ, et al. (2014) Anatomy and biomechanics of the craniovertebral junction. Neurosurg Focus 38: E2.
- Smoker WRK, Khanna G (2008) Imaging the craniocervical junction. Child’s Nerv Syst 24: 1123-1145.
- Pinter NK, McVige J, Mechtler L (2016) Basilar Invagination, Basilar Impression, and Platybasia: Clinical and Imaging Aspects. Curr Pain Headache Rep 20: 49.
- Hankinson TC, Anderson RC (2010) Craniovertebral junction abnormalities in Down syndrome. Neurosurgery 66: 32-38.
- Borgo A, Cossio A, Gallone D, Vittoria F, Carbone M (2018) Orthopaedic challenges for mucopolysaccharidoses. Ital J Pediatr 44: 123.
- Broomfield A, Zuberi K, Mercer J, Moss G, Finnegan N, et al. (2018) Outcomes from 18 years of cervical spine surgery in MPS IVA: a single centre's experience. Childs Nerv Syst 34: 1705-1716.
- Behari S, Mehrotra A, Sharma P, Nayak S (2005) In Tuberculosis of Craniovertebral junction. Pg no: 167-177.
- Ferrante A, Ciccia F, Giammalva GR, Iacopino DG, Visocchi M, et al. (2019) The Craniovertebral Junction in Rheumatoid Arthritis: State of the Art. Acta Neurochir Suppl 125:79-86.
- Rojas CA, Bertozzi JC, Martinez CR, Whitlow J (2007) Reassessment of the Craniocervical Junction: Normal Values on CT. AJNR Am J Neuroradiol 28: 1819-1823.
- Powell EC, Leonard JR, Olsen CS, Jaffe DM, Anders J, et al. (2017) Atlantoaxial Rotatory Subluxation in Children. Pediatr Emerg Care 33: 86-91.
- O'Sullivan MD, Lyons F, Morris S, Synnott K, Munigangaiah S, et al. (2018) Metastasis Affecting Craniocervical Junction: Current Concepts and an Update on Surgical Management. Global Spine J 8: 866-871.
Citation: Maheshwari S, Bhat V, Kumar KBN (2021) Imaging of Normal and Abnormal Cranio-Vertebral Junction - A Pictorial Review. J Brain Neursci 5: 018.
Copyright: © 2021 Venkatraman Bhat, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.