
Impact of Complications on the Quality of Life of Patients Who Underwent Surgery for Adult Spinal Deformity
*Corresponding Author(s):
Esteban Blanco MartaDepartment Of Orthopedic Surgery, Universitary Hospital Of Leon, Leon, Spain
Tel:+34 650894501,
Email:mestebanb.asitec@saludcastillayleon.es
Abstract
Study Design: A multicenter, retrospective review of surgical patients with adult spine deformity.
Objective: Analyze the impact on the quality of life of patients who suffer complications in adult spine deformity surgery.
Summary of Background Data: Adult spine deformity surgery is classically associated with a high rate of complications, in particular it is estimate around 40%. The knowledge of the impact these complications could be a useful to improve the outcome in quality of life of patients.
Methods: Retrospective analysis of a prospective database of a cohort of patients who underwent spinal deformity surgery. Patients with 4 or more instrumented vertebras and 2 years follow-up of were included. We created two groups based on the development or not of complications. VAS, ODI and SRS22, as a quality of life questionnaires, were used. Statistical analysis was performed using: T Student and U Mann-Whitney tests depending if variables were adjusted or not to normality; independent and related samples were analyzed with W Wilcoxon test.
Results: 65 patients from primary surgery completed all the protocols (75.4% female), mean age of the cohort was 68±6.21 years, the average number of levels fused was 7±3.37, with an operative time of 305.47±116.90 minutes with 406.50±92.7mL of estimated blood loss. 24 patients suffered complications including PJK, instrumentation rupture, malposition material and infection. The results of the quality of life of patients with complications showing a significant statistical improvement in all parameters except the function subdomain (Pre-Complication: 2.55±0.66; Post-Complication 2.93±0.85, p=0.082) and satisfaction subdomain (Pre-Complication 3.25±1.25; Post-Complication 3.84±0.91, p=0.095) of the SRS-22 regarding the preoperative. The disability, that the ODI shows, is better and statistically significant than the preoperative one although it remains at high levels (Pre-Complication 57.58±16.01; Post-Complication 43.47±17.1, p<0.05). Considering the pain in the VAS back [(Pre-Complication 8 (5.50-9); Post-Complication 4 (1.50-7.50), p<0.05] and VAS leg [(Pre- Complication: 8 (5-8); Post 2 (0.50-5), p<0.05] this significant improvement after complication. Quality of life parameters in patients with complications were affected, although with no statistically significant differences in comparison to the group of patients without re-surgery for some complication.
Conclusion: The impact on quality of life of subjects who suffer complications in comparison to those that do not is reflected in greater functional limitations and worse results in subdomains of the SRS-22 questionnaire, despite improving after the surgery and without significant differences in comparison to the group of patients free from complications.
Keywords
Adult spinal deformity; Deformity surgery; Underwent surgery
Introduction
Spinal deformity is defined as a curvature in the spine where the alignment is outside of defined normal limits and as a consecuence with a significant and measurable impact on Health-Related Quality of Life (HRQoL) [1,2]. Considering that Adult Spinal Deformity (ASD) surgery is a complex procedure that involve many risks, a benefit of the surgery must be achieved [3]. The prevalence of adult scoliosis in the general population has been reported to be up to 32% and as high as 68% in the older population [4-8].
The complications in deformity surgery are diverse, there are a variety of authors who talk about them and the rate at which they occur is highly variable [9,10]. Glassman et al. [11], reported that 108 of 434 (24.9%) of ASD patients developed a complication, a combined medical and surgical complications. Schwab et al. [12], found that 80 of 953 (8.4%) ASD patients had a major complication in their study the series was retrospective and also combined surgical and medical complications.
The evaluation of the impact that ASD has on health has been facilitated by the development of validated HRQoL questionnaires [13,14]. General health questionnaires are designed to assess the overall physical and mental health status of the individual for example the Medical Outcomes Short Form 36 (SF-36) and EuroQol Five Dimension questionnaire (EQ5D). Disease-specific questionnaires are designed to assess the impact that a specific disease process has upon quality of life, two examples of this are the Oswestry Disability Index (ODI) which measure disability percent that people suffer in their daily life [15] and the Scoliosis Research Society (SRS) questionnaire, which is designed to evaluate functional limitations secondary to spinal deformities and which provide 5 subdomais: function, pain, self-image, mental health and satisfaction [13,16-18].
According to HRQoL and complications found that the incidence of implant-related complications was 31.7% and 52.6% of these patients were re-operated, rod breakage accounted for 47% of implant-related complications, and Proximal Junction Kyphosis (PJK) accounted for 54.5% of radiographic complications, all these complications negatively affected HRQoL measurement [19]. Apart of this, early revision surgery for unforeseen complications has a negative impact on health, 41.3% of complications were implant related, 19.6% due to deep surgical site infections, 19.6% due to PJK [20].
The purpose of this study was to further examine the impact of postoperative complications on clinical outcome. In particular, we analyze the impact on the quality of life of patients suffering complications in ASD surgery.
Material And Methods
Database
This study is a retrospective analysis of a multicenter prospective database of consecutively enrolled patients with ASD.
Inclusion criteria
Inclusion criteria for the whole database were age more than 18 years and presence of spinal deformity, as defined by at least 1 of the following: scoliosis Cobb angle of 20° or greater, Sagittal Vertical Axis (SVA) of 5 cm or greater, Pelvic Tilt (PT) of 25° or greater, and/or thoracic kyphosis of 60° or more. The minimum of instrumented vertebra were 4. The present study included patients only with completed and 2 years follow-up. Exclusion criteria were spinal deformity of a neuromuscular etiology, presence of malignancy and patients who were not able to complete the questionnaires.
Data collection
Demographic and surgical data: The demographic and clinical data were obtained for each patient: age, sex, Body Mass Index (BMI), instrumented levels, time of surgery and bleeding.
Health-Related Quality of Life (HRQoL): Standardized HRQoL measures included Visual Analogue Scale (VAS) spine and leg, Oswestry Disability Index (ODI), Refined Scoliosis Research Society-22 (SRS-22), and were collected at baseline and post-complication and at the end of follow-up.
Complications
Complications included were instrumentation rupture, material malposition and PJK (Figure 1). Medical complication registered was infection with revision surgery.
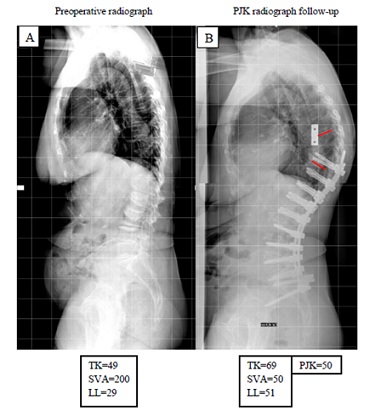 Figure 1: (A) Preoperative lateral radiograph showing global sagittal malalignment with 49° Thoracic Kyphosis (TK), 29º lumbar lordosis and 200mm of Sagittal Vertical Axis (SVA) in a patient with a history without previous instrumentation surgery. (B) A radiograph obtained 1 year postoperatively showing a 50 degrees of Proximal Junctional Kyphosis (PJK).
Figure 1: (A) Preoperative lateral radiograph showing global sagittal malalignment with 49° Thoracic Kyphosis (TK), 29º lumbar lordosis and 200mm of Sagittal Vertical Axis (SVA) in a patient with a history without previous instrumentation surgery. (B) A radiograph obtained 1 year postoperatively showing a 50 degrees of Proximal Junctional Kyphosis (PJK).
Statistical analysis
Statistical analysis was performed using SPSS v21 (IBM). Statistical analysis was performed using T Student test and U Mann-Whitney test depending on whether the variables adjusted to normality or not for independent samples and for related samples W-Wilcoxon test.
Results
Of 83 cases enrolled, 65 (79%) with 2 years follow-up were therefore included in the study. Within this population, 75.4% (n=49) were female, mean age of the cohort was 68±6.21 years, the average number of levels fused was 7±3,37, with an operative time of 305.47±116.90 minutes with 406.50±92.7mL of estimated blood loss. Implant-related complications were seen in 18 (27.69%) and medical complications were observed in 6 patients (9.23%).
In patients who had complications, there were no significant statistical differences in SRS22 function subdomain pre-surgery before complication (2.55±0.66) compared to one year postoperative (2.93±0.85, p=0.082) and neither between SRS22 satisfaction subdomain pre-surgery (3.25±1.25) and one year postoperative (3.84±0.91, p=0.095). There were no significant differences in remain domains of SRS-22 scores, VAS back, VAS leg and ODI questionnaires among pre-surgery before complication and at one year postoperation (Table 1).
|
Pre |
Post |
p-Value |
|
|
VAS back* |
8 (5.50-9) |
4 (1.50-7.50) |
<0.05 |
|
VAS leg* |
8 (5-8) |
2 (0.50-5) |
<0.05 |
|
ODI |
57.58 (16.01) |
43.47 (17.1) |
<0.05 |
|
SRS22 Function |
2.55 (0.66) |
2.93 (0.85) |
0.082 |
|
SRS22 Pain* |
1.80 (1.40-2.90) |
3.00 (2.20-4.00) |
<0.05 |
|
SRS22 Self-image |
2.23 (0.86) |
3.04(0.70) |
<0.05 |
|
SRS22 Mental health |
2.30 (0.81) |
3.65 (0.77) |
<0.05 |
|
SRS22 Satisfaction |
3.25 (1.25) |
3.84 (0.91) |
0.095 |
|
SRS22 Total |
2.33 (0.69) |
3.19 (0.76) |
<0.05 |
Table 1: Health-Related Quality of Life Scores in patients pre-surgery before complication and at one year post operation.
Note: Values expressed in means and standard deviations. P-values calculated with the Student's T test for related samples. * No-normal values: data expressed in medians and interquartile ranges. P-value calculated with the Wilcoxon W test.
Patients with HRQoL at 2 years follow-up were divided in two groups, with and without complications. 24 patients (36.95%) had some type of complication (Table 2). There was no significant statistics differences in all questionnaires SRS-22, VAS back, VAS leg and ODI between groups, biggest limitation was observed in patients who suffered complications (46.00±15.99) compared to no complications (39.22±19.47, p=0.175) (Table 3).
|
Complication Type |
Prevalence |
|
Proximal Junctional Kyphosis (PJK) |
16.92% |
|
Instrumentation rupture |
6,15 % |
|
Malposition material |
34.62% |
|
Infection |
9.23% |
Table 2: Complications in study population.
|
|
No complication |
Yes complication |
P-Value |
|
VAS Back* |
2.50 (0-6) |
5 (2.50-8) |
0.086 |
|
VAS Leg* |
2 (0-5.25) |
4 (1-7.75) |
0.204 |
|
ODI |
39.22 (19.47) |
46 (15.99) |
0.175 |
|
SRS22 Function |
3.01 (0.81) |
2.86 (0.79) |
0.543 |
|
SRS22 Pain |
2.96 (0.93) |
2.88 (1.02) |
0.781 |
|
SRS22 Self-image* |
3 (2.45-3.80) |
3 (2.20-3.40) |
0.285 |
|
SRS22 Mental health |
4 (2.65-4.509 |
3.80 (3-4) |
0.190 |
|
SRS22 Satisfaction* |
4.25 (3.50-4.88) |
4 (3-4.50) |
0.389 |
|
SRS22 Total |
3.25 (0.80) |
3.11 (0.72) |
0.520 |
Table 3: Health-related quality of life scores in two groups (yes o no complication) 2 years follow-up.
Note: Values expressed in means and standard deviations. P-values calculated with the Student's T test for related samples.
* No-normal values: data expressed in medians and interquartile ranges. P-value calculated with test U de Mann-Whitney.
Discussion
The diversity of complications are a reflect that the complexity of spinal surgery. These complications may occur months and years later because this procedures are a complex and high- risk. Surgical treatment for ASD is increasing due to high number of elderly patients in the general population. The initial decision from these patients would likely to be based avoiding unnecessary risk and adopt conservative measures, but when this decision failed the surgery could be the only option. Under this premise, every effort should be undertaken to avoid as much as possible to appear a lot of future complications in ASD surgery [10,21,22].
Complications associated with ASD surgery have been evaluated thoroughly. The complications in deformity surgery are diverse, there are a variety of authors who talk about them and the rate at which they occur is highly variable [9,10]. The ISSG group conducted a systematic review that concluded the total number of complications was 3.615 in relation of 11.692 people population of study. The overall rate complication rate was 55%. And long-term complications occurred at an average rate of 20.5% [23]. In our study, we found that 18 of 65 (36.92%) of patients developed a complication, the complication rate in our series is according to the literature.
One of the most relevant complication in ASD is PJK but at the moment authors have no agreement on its definition, Bridwell and colleagues were first defined PJK in the literature as a “the caudal endplate of the UIV to the cephalad endplate two vertebrae proximal. Abnormal PJK was defined by 2 criteria: (1) proximal junction sagittal Cobb angle≥10° and (2) proximal junction sagittal Cobb angle at least 10° greater than the preoperative measurement” [24]. Other researcher defined as Bridwell but the angle was 20 degrees [25]. Different studies reported that angulation varied from 5 to 20 degrees [24-28]. To date, more accepted angulation for PJK in the literature is 10 degrees greather than preoperative measurement [24,29-31]. For that reason our PJK angle was defined as at least 10 degrees regarding preoperatory. The prevalence of PJK is not defined completely because depends on variety of factors [32-34]. Therefore, PJK prevalence rates fluctuate widely, it is possible to find that PJK occurs in 5% to 46% of patients who go through spinal deformity surgery [35]. Our PJK prevalence (16.92%) is not much elevate according to this information.
Infections from surgery can manifest months or years later even 8 years after surgery. 5-10% of patients developing deep infections its produced the next 11-45 months after surgery [36-38]. Infections reportedly are becoming more common, perhaps due to larger instrumentation used or maybe due to the increasing prevalence of multi-drug resistant bacteria in hospital settings [10,39]. We analyzed a combined complications but we know our infection percentage was 9.23% its higher than studies reported about medical complications for example this author Charosky et al. [40], showed in a retrospective serie that 3.7% ASD patients experienced a medical complication. Additionally, Blamoutier et al. [41], in their retrospective review of ASD patients, demonstrated that 5.5% had a medical complication. Plitter et al42 had a 11.8% infection rate that was higher than our outcome that involve infection incidence is highly variable.
The impact of complications on HRQoL after ASD surgery is controversial in the literature but is associated with a significant negative impact on HRQoL in affected individuals [4,19]. Some studies suggest that complications significantly affect HRQoL scores, with patients who experience late complications having a lesser improvement in ODI this occur in our patients who suffer complications in comparison with 1 year and 2 years follow-up [11,43,44].
When the SRS questionnaire scores of ASD patients are compared to scores reported by age-matched individuals without spinal deformity, patients with ASD have greater pain like our patients in VAS outcomes greater limitations in function, as well as poorer selfimage and mental health however we don´t found significant differences in both groups in this terms [4,45]. Complications also demonstrated no significant effect on satisfaction agree on Hamilton et al. [46]. Our patients obtain an improvement in HRQoL after surgery despite suffer complications.
One of the limitations of the study might be the inherent limitations to all multicentre studies and this study is a retrospective study. This introduces susceptibility to unidentified confounders and both selection and information bias. These prejudice were mitigated, however, by the fact that the data was collected in a prospective manner. Other limitation very important is the small sample size and the lack of statistical power to detect differences between groups. With a bigger sample, possible differences might be better delimited and/or patients could be stratified according to complication characteristics.
Conclusion
The impact on the quality of life of patients who have complications is reflected in a greater functional limitation and worse results in the SRS-22 subdomains, but despite these patients have an improvement in their HRQoL. Knowing the complication rate of ASD surgery can allow us to establish and to improve as much the surgery planing as the quality of life to potential patients.
Acknowledgment
We are grateful for support from the Complejo Asistencial Universitario de León.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Halawi MJ (2015) Outcome measures in total joint arthroplasty: Current status, challenges, and future directions. Orthopedics 38: 685-689.
- Good CR, Auerbach JD, O’Leary PT, Schuler TC (2011) Adult spine deformity. Curr Rev Musculoskelet Med 4: 159-167.
- Riley MS, Bridwell KH, Lenke LG, JDalton J, Kelly MP (2018) Health-related quality of life outcomes in complex adult spinal deformity surgery. J Neurosurg Spine 28: 194-200.
- Ames CP, Scheer JK, Lafage V, Smith JS, Bess S, et al. (2016) Adult spinal deformity: Epidemiology, health impact, evaluation, and management. Spine Deform 4: 310-322.
- Carter OD, Haynes SG (1987) Prevalence rates for scoliosis in US adults: Results from the first National Health and Nutrition Examination Survey. Int J Epidemiol 16: 537-544.
- Kostuik JP, Bentivoglio J (1981) The incidence of low-back pain in adult scoliosis. Spine 6: 268-273.
- Pérennou D, Marcelli C, Hérisson C, Simon L (1994) Adult lumbar scoliosis. Epidemiologic aspects in a low-back pain population. Spine 19: 123-128.
- Schwab F, Dubey A, Gamez L, El Fegoun AB, Hwang K, et al. (2005) Adult scoliosis: Prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine 30: 1082-1085.
- Yadla S, Maltenfort MG, Ratliff JK, Harrop JS (2010) Adult scoliosis surgery outcomes: A systematic review. Neurosurg. Focus 28: 1-7.
- Weiss HR, Goodall D (2008) Rate of complications in scoliosis surgery - A systematic review of the Pub Med literature. Scoliosis 3: 9.
- Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, et al. (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine 32: 2764-2770.
- Schwab FJ, Hawkinson N, Lafage V, Smith JS, Hart R, et al. (2012) Risk factors for major peri-operative complications in adult spinal deformity surgery: A multi-center review of 953 consecutive patients. Eur Spine J 21: 2603-2610.
- McCormick JD, Werner BC, Shimer AL (2013) Patient-reported outcome measures in spine surgery. J Am Acad Orthop Surg 21: 99-107.
- Pellisé F, Vila-Casademunt A, Ferrer M, Domingo-Sàbat M, Bagó J, et al. (2015) Impact on health related quality of life of Adult Spinal Deformity (ASD) compared with other chronic conditions. Eur Spine J 24: 3-11.
- Mehra A, Baker D, Disney S, Pynsent PB (2008) Oswestry disability index scoring made easy. Ann R Coll Surg Engl 90: 497-499.
- Baldus C, Bridwell KH, Harrast J, Edwards C, Glassman S, et al. (2008) Age-gender matched comparison of SRS instrument scores between adult deformity and normal adults: Are all SRS domains disease specific? Spine 33: 2214-2218.
- Bridwell KH, Cats-Baril W, Harrast J, Berven S, Glassman S, et al. (2005) The validity of the SRS-22 instrument in an adult spinal deformity population compared with the Oswestry and SF-12: A study of response distribution, concurrent validity, internal consistency, and reliability. Spine 30: 455-461.
- Asher MA, Min Lai S, Burton DC (2000) Further development and validation of the Scoliosis Research Society (SRS) Outcomes Instrument. Spine 25: 2381-2386.
- Soroceanu A, Diebo BG, Burton D, Smith JS, Deviren V, et al. (2015) Radiographical and implant-related complications in adult spinal deformity surgery: Incidence, patient risk factors, and impact on health-related quality of life. Spine 40: 1414-1421.
- Yagi M, Fujita N, Okada E, Tsuji O, Nagoshi N, et al. (2018) Impact of frailty and comorbidities on surgical outcomes and complications in adult spinal disorders. Spine 43: 1259-1267.
- Glassman SD, Bridwell KH, Shaffrey CI, Edwards CC, Lurie JD, et al. (2018) Health-related quality of life scores underestimate the impact of major complications in lumbar degenerative scoliosis surgery. Spine Deform 6: 67-71.
- Carreon LY, Glassman SD, Shaffrey CI, Fehlings MG, Dahl B, et al. (2017) Predictors of health-related quality-of-life after complex adult spinal deformity surgery: A scoli-RISK-1 secondary analysis. Spine Deform 5: 139-144.
- Sciubba DM, Yurter A, Smith JS, Kelly MP, Scheer JK, et al. (2015) A comprehensive review of complication rates after surgery for adult deformity: A reference for informed consent. Spine Deform 3: 575-594.
- Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, et al. (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: Incidence, outcomes, and risk factor analysis. Spine 30: 1643-1649.
- O?Shaughnessy B, Bridwell KH , Lenke LG, Cho W, Baldus C, et al. (2012) Does a long-fusion ‘T3-sacrum’ portend a worse outcome than a short-fusion ‘T10-sacrum’ in primary surgery for adult scoliosis? Spine 37: 884-890.
- Helgeson MD, Shah SA, Newton PO, Clements DH, Betz RR, et al. (2010) Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine 35: 177-181.
- Hostin R, McCarthy I, O?Brien M, Bess S, Line B, et al. (2013) Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine 38: 1008-1015.
- Lee GA, Betz RR, Clements DH, Huss GK (1999) Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine 24: 795-799.
- Cho SK, Shin JI, Kim YJ (2014) Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J 23: 2726-2736.
- Hart RA, McCarthy I, Ames CP, Shaffrey CI, Hamilton DK, et al. (2013) Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am 24: 213-218.
- Park SJ, Lee CS, Chung SS, Lee JY, Kang SS, et al. (2017) Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: Survivorship analysis of 160 patients. Neurosurgery 80: 279-286.
- Kim HJ, Lenke LG, Shaffrey CI, Alstyne EMV, Skelly AC (2012) Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery: A systematic review. Spine 37: 144-164.
- Arlet V, Aebi M (2013) Junctional spinal disorders in operated adult spinal deformities: Present understanding and future perspectives. Eur Spine J 2: 276-295.
- Maruo K, Ha Y, Inoue S, Samuel S, Okada E, et al. (2013) Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine 38: 1469-1476.
- Lau D, Clark AJ, Scheer JK, Daubs MD, Coe JD, et al. (2014) Proximal junctional kyphosis and failure after spinal deformity surgery: A systematic review of the literature as a background to classification development. Spine 39: 2093-2102.
- Muschik M, Lück W, Schlenzka D (2004) Implant removal for late-developing infection after instrumented posterior spinal fusion for scoliosis: Reinstrumentation reduces loss of correction. A retrospective analysis of 45 cases. Eur Spine J 13: 645-651.
- Clark CE, Shufflebarger HL (1999) Late-developing infection in instrumented idiopathic scoliosis. Spine 24: 1909-1912.
- Asher M, Cook S, Lai SM (2001) Re: Late operative site pain with isola posterior instrumentation requiring implant removal: Infection or metal reaction? Spine 26: 2516-2517.
- Richards BS, Emara KM (2001) Delayed infections after posterior TSRH spinal instrumentation for idiopathic scoliosis: Revisited. Spine 26: 1990-1996.
- Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D, et al. (2012) Complications and risk factors of primary adult scoliosis surgery: A multicenter study of 306 patients. Spine 37: 693-700.
- Blamoutier A, Guigui P, Charosky S, Roussouly P, Chopin D (2012) Surgery of lumbar and thoracolumbar scolioses in adults over 50. Morbidity and survival in a multicenter retrospective cohort of 180 patients with a mean follow-up of 4.5years. Orthop Traumatol Surg Res 98: 528-535.
- Pitter FT, Lindberg-Larsen M, Pedersen AB, Dahl B, Gehrchen M (2019) Revision risk after primary adult spinal deformity surgery: A nationwide study with two-year follow-up. Spine Deform 7: 619-626.
- Glassman SD, Schwab F, Bridwell KH, Shaffrey C, Horton W, et al. (2009) Do 1-year outcomes predict 2-year outcomes for adult deformity surgery? Spine J 9: 317-322.
- Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, et al. (2007) Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine 32: 2232-2237.
- Bombardier C (2000) Outcome assessments in the evaluation of treatment of spinal disorders: Summary and general recommendations. Spine 25: 3100-3103.
- Hamilton DK, Kong C, Hiratzka J, Contag AG, Ailon T, et al. (2017) Patient satisfaction after adult spinal deformity surgery does not strongly correlate with health-related quality of life scores, radiographic parameters, or occurrence of complications. Spine 42: 764-769.
Citation: Marta EB, Jesus BN, Jose HE, Ana LM, Andrés BH, et al. (2022) Impact of Complications on the Quality of Life of Patients Who Underwent Surgery for Adult Spinal Deformity. Archiv Surg S Educ 4: 038.
Copyright: © 2022 Esteban Blanco Marta, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

